(1)
Neurological Department, Municipal Hospital Dessau, Dessau-Rosslau, Germany
Similar to autoimmune neuropathies, plexiform growth variants of tumors of the peripheral nerve sheath (plexiform neurofibroma, perineurioma) may lead to a focal, mostly fusiform, nerve swelling with hypertrophic fascicles. High resolution ultrasound then evaluates a focal enlargement of the cross sectional area of the affected nerve and its fascicles as well as a hypoechoic appearance or even a complete masking of the normal echotexture. Moreover, tumors of the peripheral nerve sheath are characterized by a gadolinium uptake on MRI, whereas different reports exist regarding this feature in the case of autoimmune neuropathies. However, careful anamnesis survey, clinical examination, and additional electrodiagnostic testing will help to differentiate between these entities (see Chaps. 5, 6 and 10).
In addition, a few, mostly very rare (except leprosy) disorders may lead to a focal nerve involvement corresponding to enlarged nerve segments or nerve roots. Clinical impairment is dependent on the underlying etiology including the type of affection, either axonal or demyelinating, and the time course (e.g. relapsing-remitting, chronic-progressive, self-limiting, etc.). Due to the enhanced imaging capabilities, including high-field MR-neurography and high resolution ultrasound, nowadays we are able to depict nearly every single nerve or nerve root of the human body. Therefore, to an increasing extent we see subjects with a focal neuropathy/mononeuropathy in whom the usual differential diagnosis provides none of the common causes of focal nerve enlargement such as in case of nerve compression, nerve sheath tumor, traumatic nerve fibrosis, poly-neuropathy, etc. In these special cases, differential diagnosis remains challenging, but it remains important because of different treatment options. However, a fascicular biopsy will mostly still become necessary to detect the underlying condition.
According to our own experience and to the available literature, the following section represents the standard of knowledge about these rare entities at the time of completion of this book. Beside plexiform growth variants of tumors of the peripheral nerve sheath and autoimmune neuropathies focal, fusiform, tumor-like nerve enlargement has been described in the following conditions:
Sarcoidosis affecting the peripheral nerve
Leprosy affecting the peripheral nerve
Amyloidosis affecting the peripheral nerve
Extramedullary affection of the peripheral nerve due to a plasmacytoma
Primary lymphoma affecting the peripheral nerve
Sarcoidosis is an inflammatory systemic disorder of unknown etiology, characterized histologically by the formation of non-caseating granuloma. In the majority of cases, lymph-nodes and lungs are involved, whereas affection of the nervous system counts for approximately 5–15 of the cases only [1, 2]. The overall incidence of this rare condition has been estimated to be around 20 per 100,000 [3]. Common manifestations of neuro-sarcoidosis within the central nervous system are non-caseating granuloma of the cranial nerves (mostly facial and optic nerves), hypothalamus and pituitary gland [1]. In contrast, involvement of the peripheral nervous system has been considered to be rare, subacute with a wide spectrum of clinical manifestations such as large-fiber mono-neuropathies, poly-radiculopathy, distal-symmetric (predominantly motor) and small fiber polyneuropathy [4–8]. Granulomatous affection of the peri- and epineurium as well as an ischaemic vasculitis may lead to axonal loss or focal demyelination due to local pressure [6, 7]. To our knowledge, one recent report exists on focal affection of the ulnar nerve due to an epineural and perineural lesion, confirmed histopathology as non-caseating sarcoid granuloma. After surgery the condition improved [9]. We ourselves observed a case with involvement of the superficial radial nerve, clinically characterized by slight numbness with swelling and erythema on the left distal forearm as well as skin manifestations of sarcoidosis (erythema nodosum). High resolution ultrasound was able to demonstrate a significant hypoechoic segmental swelling of fascicles of the superficial radial nerve as well as an encasement by an (also hypoechoic) granuloma. Moreover, we were able to demonstrate the hyper-vascularization of the epineurium and the granuloma (Fig. 14.1).
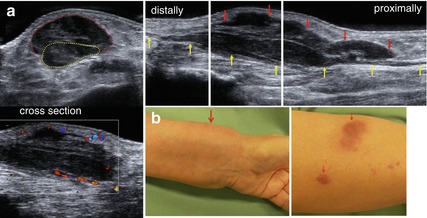
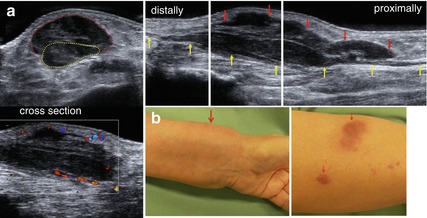
Fig. 14.1
Involvement of the superficial radial nerve in a patient with sarcoidosis. (a) HRUS, segmental hypoechoic swelling of the superficial radial nerve as well as effacement of its fascicles (yellow arrows, yellow dotted line). The encasement by the hypervascularized granuloma (red arrows, red dotted line) is clearly to be seen. (b) Clinical presentation with swelling and erythema on the left distal forearm as well as skin manifestations of sarcoidosis (erythema nodosum), red arrows
Leprosy (HANSEN´s disease) is an infectious disorder leading among others to a granulomatous affection of the peripheral nerves. It is caused by Mycobacterium leprae and Mycobacterium lepromatosis. The disorder is common in a few countries such as, e.g. India, China and Egypt with about 250,000 new cases being detected every year [10]. Lepromatous leprosy usually affects the peripheral nerves diffusely, whereas the tuberculoid form is restricted to a smaller area of a nerve due to an active immunologic response [10]. The reactions mentioned above will lead to a clinically palpable nerve thickening. Therefore, it is no surprise that high resolution ultrasound is also able to demonstrate these alterations. Recently, it has been shown that in patients with leprosy the peripheral nerves and the surrounding epineurium were significantly thicker as compared to controls. Furthermore, in 50 % of cases a partial or total loss of the normal nerve-echotexture, characterized by masking of fascicles or hypoechoic fascicles could be demonstrated. Moreover, an increased endo- or perineural flow suggestive of increased neural vascularity by colour-Doppler was observed in 26 % of involved patients, and it was always associated with leprosy treatment reactions in patients undergoing antibiotic therapy [11–13]. Therefore, in future ultrasonography may prove to be a useful technique for diagnosis as well as to assess the extent of the disease, the response to antibiotic therapy, and treatment reactions in patients undergoing antibiotic therapy. Surgery is restricted to releasing entrapment situations.
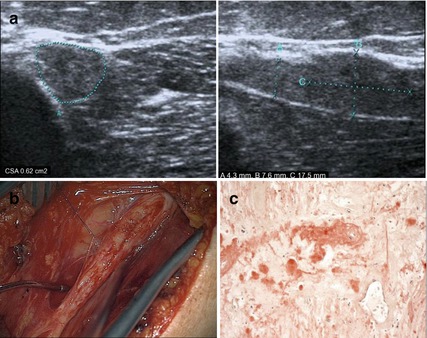
The term amyloidosis describes a rare condition wherein normally soluble proteins are deposited as insoluble amyloid in the extracellular space of body organs; they cause abnormal protein build-up in tissues and may lead to organ dysfunction [14]. Therefore, acquired amyloidosis is not a disease of its own but associated with other diseases like renal failure, which needs long-term haemodialysis [15]. On the other hand, inherited forms have been described. The prevalence is said to be fewer than 200,000 individuals within the Unites States of America [14]. There are 27 amyloidogenic proteins associated with known human diseases. For a detailed overview of the clinical features, diagnosis and therapy of the condition, please refer to the specialist literature [14]. If a biopsy of the affected organ was carried out, deposited amyloid can be identified histologically by a pink appearance after Congo red staining using bright-field microscopy, whereas in polarized light it demonstrates an apple-green birefringence [16]. However, the different types of amyloid are indistinguishable using light microscopy and other procedures like immunogold electron microscopy or mass spectrometry are needed instead [17]. The main presentation of AL-amyloidosis is a generalized distal symmetrical sensory-motor neuropathy. In a patient with AL-amyloidosis neuropathy, electrophysiologically characterized by a pure axonal loss, high resolution ultrasound could demonstrate a generalized thickening of the peripheral nerves, caused by an increasing number of the identifiable fascicles, but with no specific pattern to these changes [18]. Focal mononeuropathy, especially of the upper limbs, is an uncommon presentation of primary amyloidosis and was confirmed by nerve biopsy (AL, light chain amyloidosis) in one case [19]. On the other hand, only a few focal tumor-like lesions in some peripheral nerves of the lower extremities or cranial nerves due to amyloidosis have been described in the literature so far, also referred to as amyloidoma. One paper reported amyloidoma of the sciatic nerve and the potential value of highfield-MR for detection [20]. Another paper stated that in two cases the amyloidoma focally affected the lumbosacral roots and plexus [21]. Both, one case report and a small study, identified four cases of an amyolidoma of the trigeminal nerve affecting the Gasserian ganglion [22, 23]. Interestingly, almost all amyloidomas of the peripheral or cranial nerves were organ restricted neoplasms, unrelated to systemic amyloidosis and of the AL- lambda type. Their biological behavior was rather indolent, reminiscent of a lymphoma of mucosa-associated lymphoid tissue [23]. On MRI a gadolinium-uptake without significant surrounding tumor-oedema was seen. By means of high resolution ultrasound, we could identify a hypoechoic lesion of the common radial nerve involving its complete course from the axilla to the radial tunnel, with a marked segmental enlargement (CSA = 0.62 cm2, diameter 7.6 mm) at the distal part of the spiral groove. In this segment, sonography indicated the presence of calcification which was later histologically confirmed to be a small metaplastic ossification. Furthermore, fascicular biopsy revealed amyloid deposition using Congo red stain and polarized light microscopy (Fig. 14.2). Curative surgical treatment by means of microsurgery was impossible.