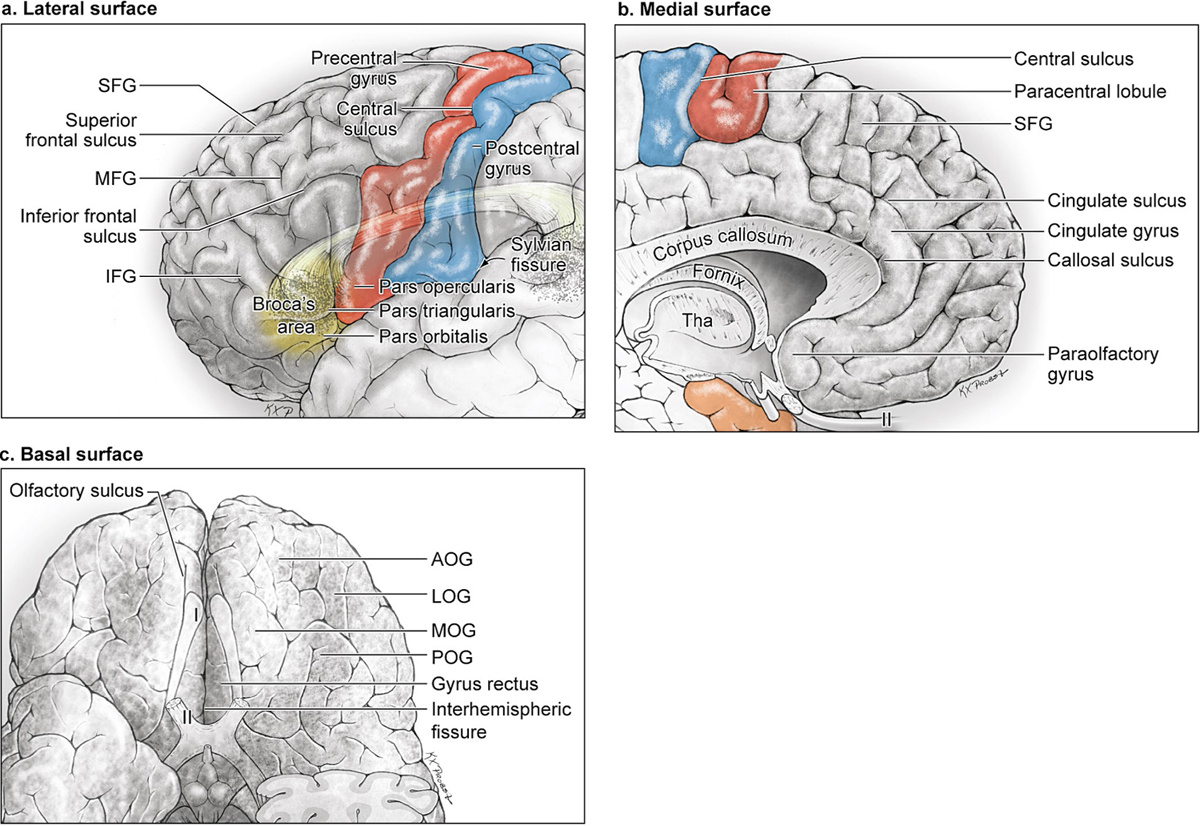
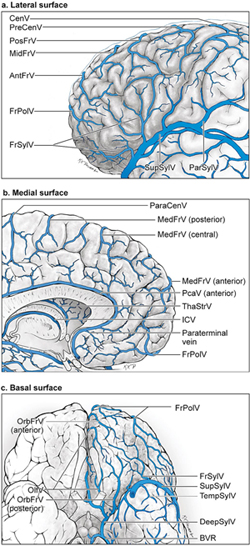
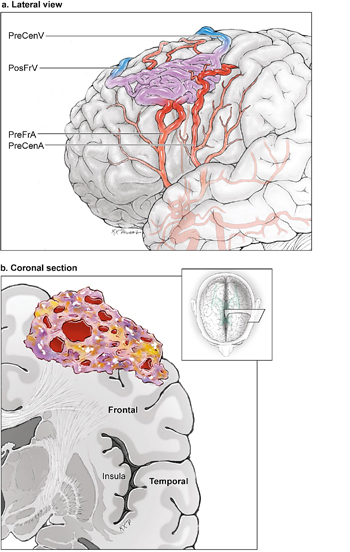
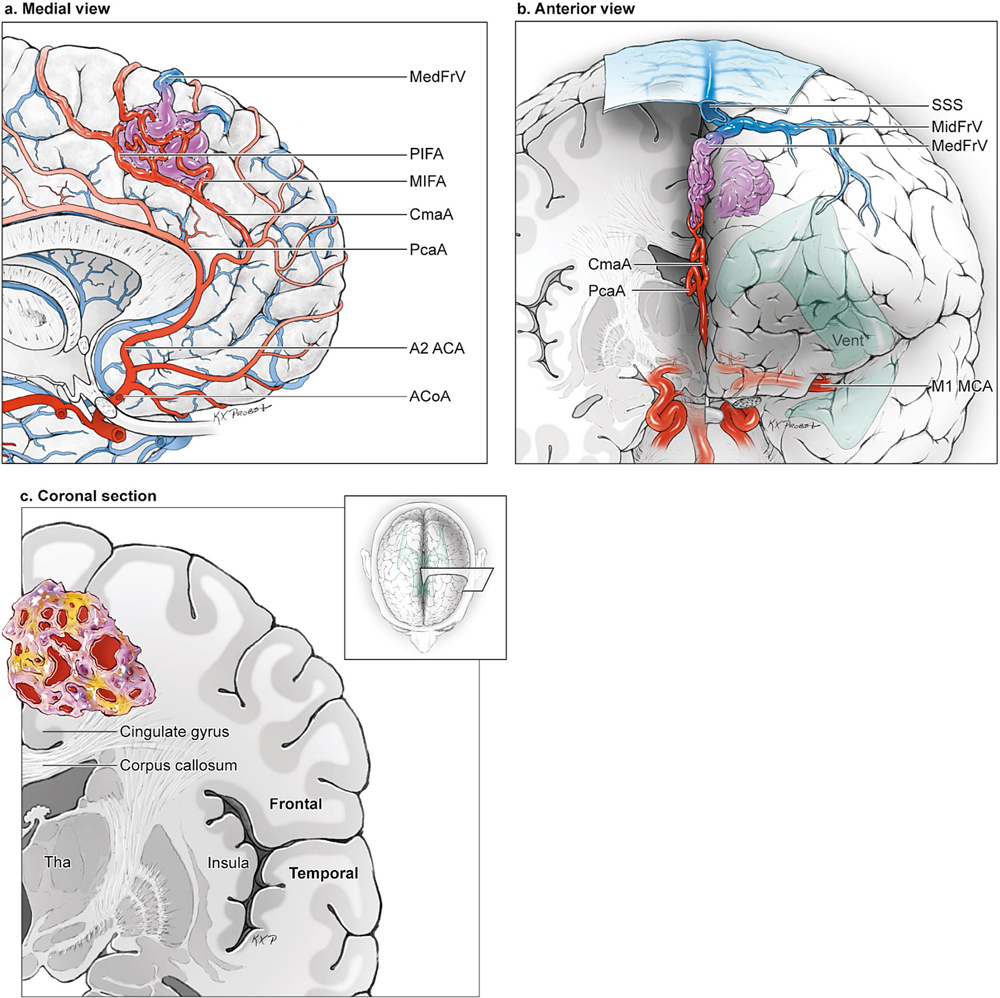
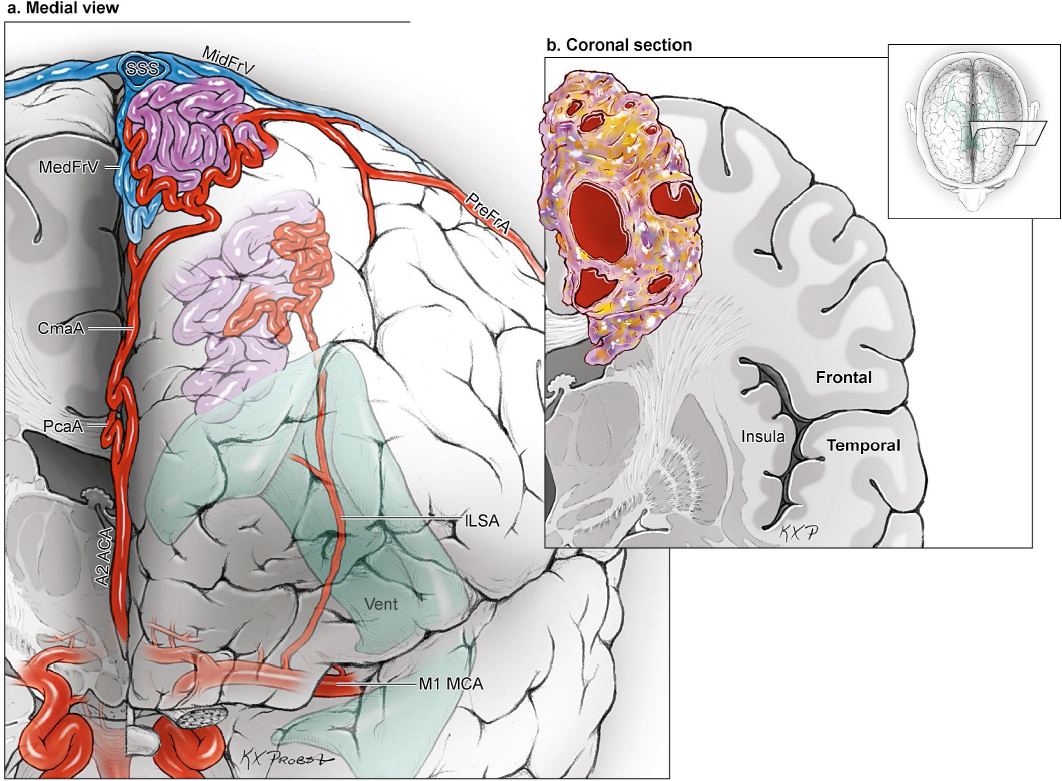
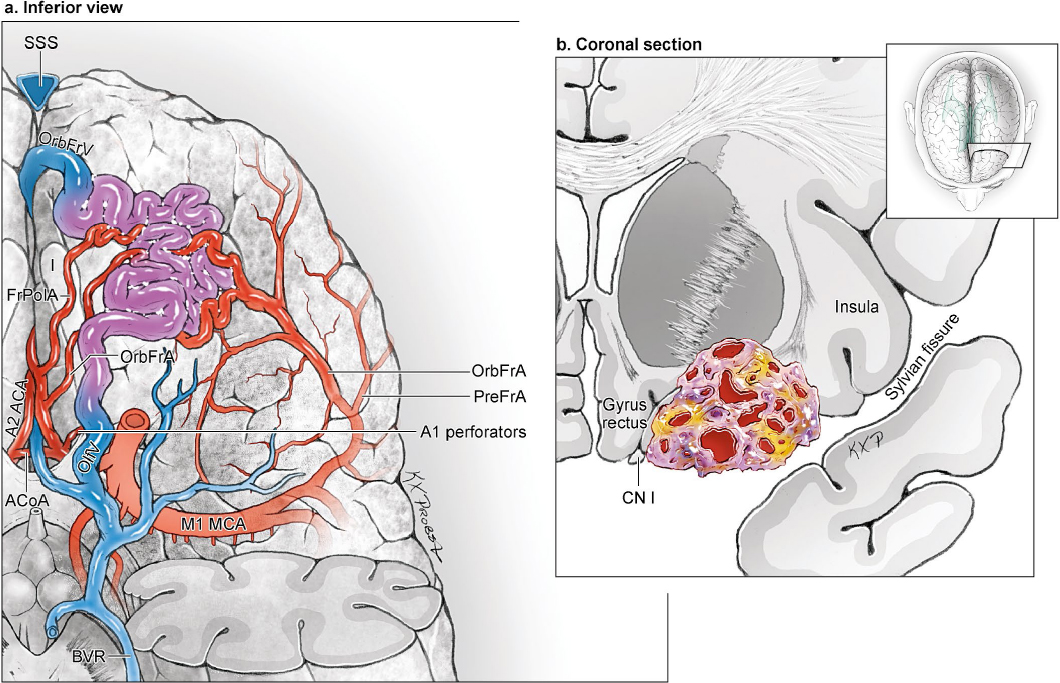
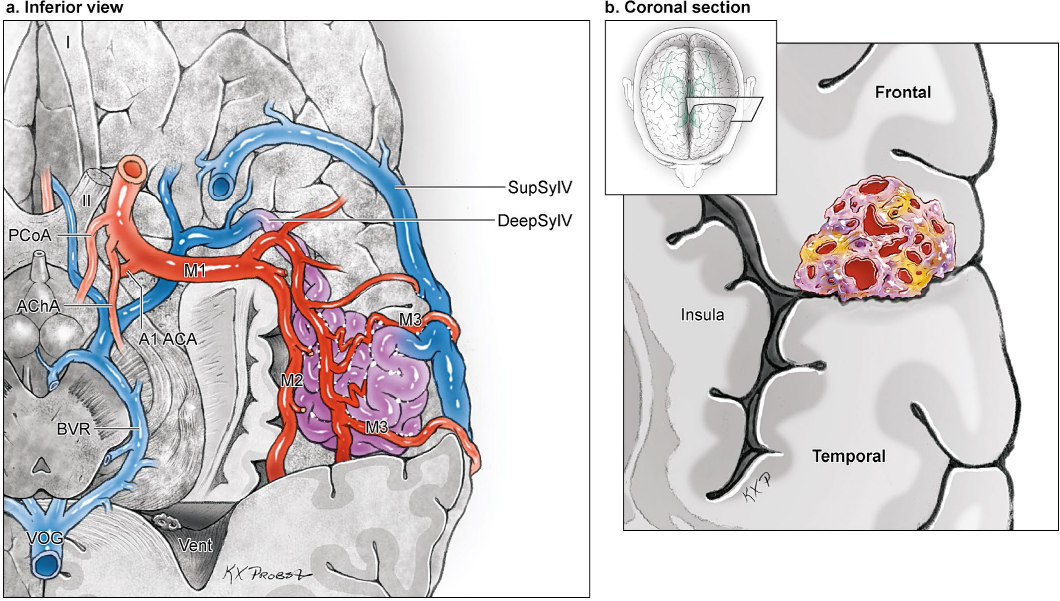
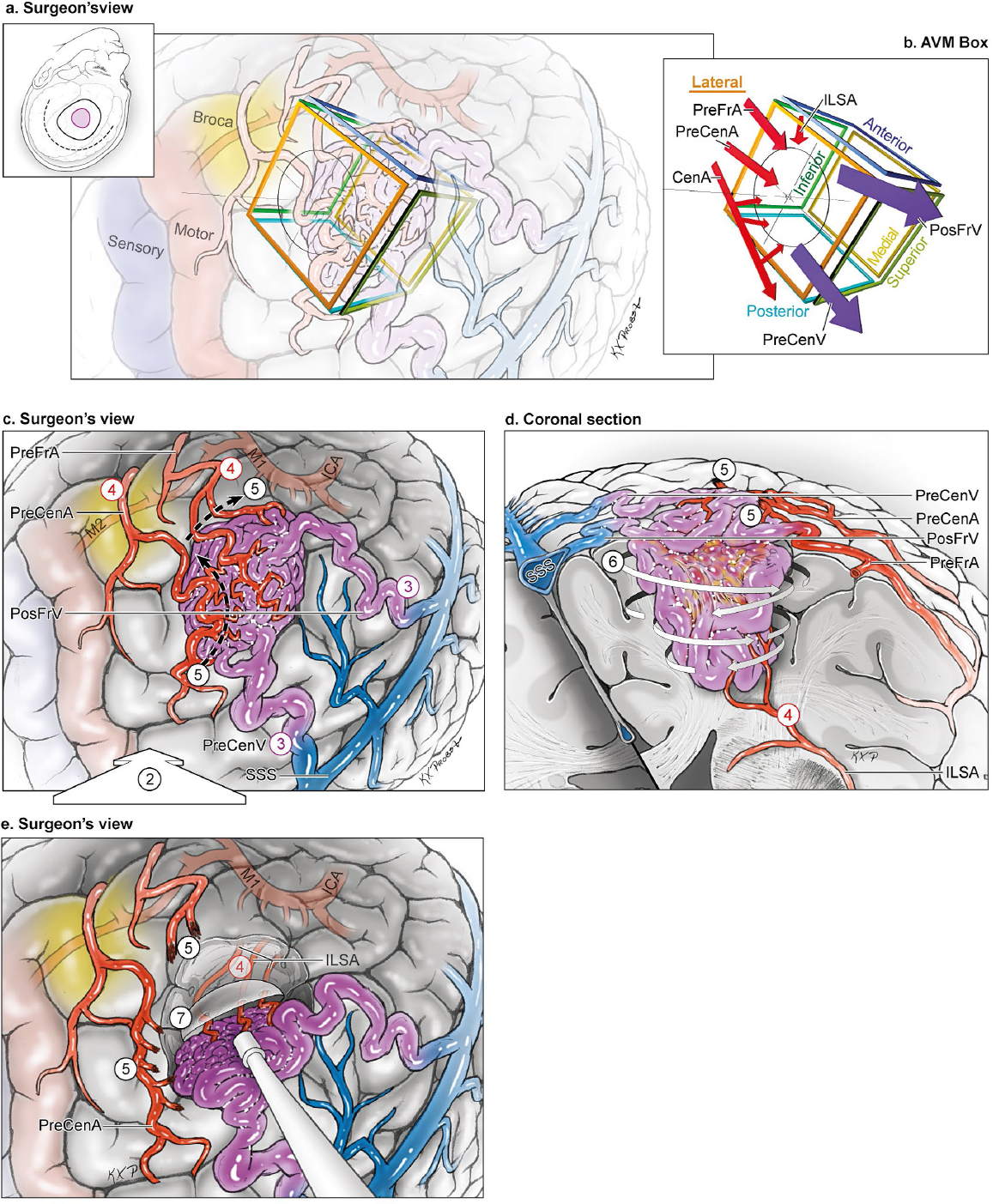
11 Frontal Arteriovenous Malformations The frontal lobe has four surfaces: lateral, medial, basal, and sylvian (Fig. 11.1). The lateral surface is composed of three horizontal gyri (superior, middle, and inferior frontal gyri; SFG, MFG, and IFG, respectively) that are separated by the superior and inferior frontal sulci. The posterior border of the frontal lobe is the central sulcus that courses from the midline to the sylvian fissure. Anterior and parallel to the central sulcus is its one vertical gyrus, the precentral gyrus. The sylvian surface of the frontal lobe is the continuation of IFG into operculum, and includes the pars orbitalis, pars triangularis, pars opercularis, and the end of precentral gyrus. The basal surface of the frontal lobe is composed of the gyrus rectus and the orbital gyri (medial (MOG), lateral (LOG), anterior (AOG), and posterior (POG). The medial surface of the frontal lobe is composed of the SFG’s medial aspect, paracentral lobule, and cingulate gyrus, as well as a small area below the rostrum with little surgical significance, consisting of paraolfactory and paraterminal gyri. Cortical areas of eloquence include the motor strip (precentral gyrus) and Broca’s speech area in the dominant hemisphere (pars triangularis and opercularis). Eloquent white matter tracts include the corticospinal or pyramidal tracts, language conduction tracts, and the olfactory tracts. Fig. 11.1 Microsurgical anatomy of the frontal lobe. (a) Lateral frontal surface (lateral view). (b) Medial frontal surface (medial view). (c) Basal frontal surface (inferior view with left temporal pole removed). Arterial supply to frontal arteriovenous malformations (AVMs) is from middle cerebral artery (MCA) branches laterally or anterior cerebral artery (ACA) branches medially (Fig. 11.2). Classically, the M1 segment divides into a superior trunk that supplies the frontal lobe and an inferior trunk that supplies the temporal lobe. However, anatomic variation produces trifurcations, quadrifurcations, and asymmetrical trunks that can be superior- or inferior-trunk dominant. In general, frontal AVMs are fed by the superior trunks. The MCA trunks divide into unnamed stem arteries as they course through the insula (M2 segment) and operculum (M3 segment), on average eight per hemisphere. These stem arteries do not acquire names until they reach the cortex (M4 segment) to supply distinct territories. The frontal lobe is supplied by two to four stem arteries that then terminate in four cortical arteries: orbitofrontal (OrbFrA), prefrontal (PreFrA), precentral (PreCenA), and central arteries (CenA). The orbitofrontal artery, the most anterior and inferior branch, supplies the inferior frontal gyrus, middle frontal gyrus (anterior part), and pars orbitalis (inferior part). The prefrontal artery supplies the pars orbitalis (superior part), pars triangularis, pars opercularis, and most of the middle frontal gyrus. The precentral artery supplies the pars opercularis (posterior part), middle frontal gyrus (posterior part), and most of the precentral gyrus. The central artery supplies the precentral gyrus (superior part) and postcentral gyrus (inferior half). All four frontal arteries emerge from the sylvian fissure and course superiorly. The ACA branches course in the interhemispheric fissure and feed the medial frontal AVMs. Eight cortical branches radiate from the ACA as it courses around the corpus callosum: orbitofrontal (OrbFrA), frontopolar (FrPolA), callosomarginal (CmaA), anterior internal frontal (AIFA), middle internal frontal (MIFA), posterior internal frontal (PIFA), paracentral (ParaCenA), and pericallosal artery (PcaA). The orbitofrontal artery is the first cortical branch of the distal ACA, arising just beyond the anterior communicating artery (ACoA) and coursing forward and down to the anterior cranial fossa floor to supply the gyrus rectus, medial orbital gyrus, and olfactory bulb/tract. Note that there are two named orbitofrontal arteries, one from the ACA and the other from the MCA. The frontopolar artery, the second branch of the distal ACA, originates from the postcommunicating or infracallosal A2 segment, courses anteriorly in the interhemispheric fissure, and supplies the frontal pole’s medial and paramedian surfaces. The internal frontal arteries supply the medial and paramedian surfaces of the superior frontal gyrus, from the frontal pole anteriorly to the paracentral lobule posteriorly. The anterior internal frontal artery (AIFA) originates from the infracallosal A2 segment adjacent to the rostrum; the middle internal frontal artery (MIFA) originates from the precallosal A3 segment adjacent to the genu, or from the callosomarginal artery; and the posterior internal frontal artery (PIFA) originates from the supracallosal A4 segment adjacent to the body of the corpus callosum. The paracentral artery arises from the A4 segment or the callosomarginal artery and supplies the paracentral lobule and its premotor, motor, and somatosensory areas. Fig. 11.2 Microsurgical anatomy of frontal lobe arteries. (a) The lateral frontal surface is supplied by the superior trunk of the MCA, which divides into stem arteries and terminates in four cortical arteries: OrbFrA, PreFrA, PreCenA, and CenA. Branches from the ACA also extend to the medial part of the lateral frontal surface. (b) The medial frontal surface is supplied by eight cortical ACA branches: OrbFrA, FrPolA, CmaA, AIFA, MIFA, PIFA, ParaCenA, and PcaA. (c) The basal frontal surface is supplied by orbitofrontal arteries from both the ACA and MCA, as well as FrPolA and PreFrA. Each frontal surface has its own network of cortical veins, anastomotic veins, and dural sinuses (Fig. 11.3). The lateral convexity is drained by the frontal veins that ascend to the superior sagittal sinus (SSS): the frontopolar vein (FrPolV); anterior (AntFrV), middle (MidFrV), and posterior frontal veins (PosFrV); and precentral (PreCenV) and central veins (CenV). The sylvian surface is drained by the frontosylvian veins (FrSylV) that descend to the superficial (SupSylV) and deep sylvian veins (DeepSylV). The medial surface of the frontal lobe is drained by the ascending medial frontal veins (MedFrV; anterior, central, and posterior). These veins course up to the superior margin of the hemisphere where they connect to the SSS or join the terminal ends of the lateral convexity veins before they connect to the SSS. The medial surface below the cingulate sulcus also has descending drainage to the anterior and posterior pericallosal veins (PcaV) that empty into the inferior sagittal sinus (ISS). The basal surface of the frontal lobe is drained by the orbitofrontal veins (OrbFrV, anterior and posterior), frontopolar vein (FrPolV), and olfactory vein (OlfV). The anterior veins (anterior OrbFrV and FrPolV) course forward to the frontal pole and empty in the SSS, whereas the posterior veins (posterior OrbFrV and OlfV) course backward to the DeepSylV in the medial sylvian fissure and continue to the basal vein of Rosenthal (BVR). Frontal AVM subtypes include the lateral frontal, medial frontal, paramedian frontal, basal frontal, and sylvian frontal. There is a subtype for each of the four frontal lobe surfaces, and an additional subtype for AVMs that have sides on both the medial and lateral surfaces. The surgical exposure of paramedian frontal AVMs requires access to two surfaces and two arterial territories, which alters the surgical strategy to warrant the additional subtype. Other frontal AVMs that have sides on two surfaces (e.g., lateral + sylvian or lateral + basal) do not require access to an additional arterial territory and can be resected with the strategy defined by its predominant surface. Fig. 11.3 Microsurgical anatomy of frontal lobe veins. (a) Veins of the lateral frontal surface (lateral view). (b) Veins of the medial frontal surface (medial view). (c) Veins of the basal frontal surface (inferior view). Lateral frontal AVMs are the stereotypical cone-shaped convexity AVMs based on the lateral frontal surface with extension toward the ventricle (Fig. 11.4). The lateral convexity is such a large surface that this subtype was the most common frontal AVM subtype, accounting for over one third of all frontal AVMs and twice as many as the other frontal subtypes. Lateral frontal AVMs are fed by MCA branches that originate from the superior trunk. More anterior frontal AVMs are fed by OrbFrA and PreFrA; more posterior frontal AVMs are fed by PreCenA and CenA; and larger AVMs are fed by all four frontal arteries. These arteries emerge from the sylvian fissure and ascend on the cortical surface to reach the inferior AVM margin. Contributions from the ACA are absent or minimal. Venous drainage is superficial, ascending to the SSS (via FrPolV, AntFrV, MidFrV, PosFrV, PreCenV, and CenV), descending to superficial sylvian veins, or both. Eloquent areas associated with lateral frontal AVMs include the motor areas posteriorly and Broca’s area inferiorly in the dominant hemisphere. Fig. 11.4 The lateral frontal AVM: (a) lateral and (b) coronal cross-sectional views. This AVM is located on the lateral frontal surface, supplied by branches from the superior MCA trunk, and drained by ascending veins to the SSS or descending veins to SupSylV. Medial frontal AVMs are located on the medial frontal surface (Fig. 11.5). Not visible on the lateral surface, they are visible on the medial surface only after opening the interhemispheric fissure. They can be superficially located in the medial aspect of the superior frontal gyrus, or deeply located in the cingulate gyrus. Cingulate AVMs are included in the medial frontal subtype, but not callosal AVMs. In contrast to lateral frontal AVMs fed by MCA branches, medial frontal AVMs are fed by ACA branches. More anterior medial AVMs are fed by OrbFrA and FrPolA; more posterior medial AVMs are fed by the internal frontal arteries and ParaCenA; and deep medial AVMs are fed by the PcaA and CmaA. The ACA feeding arteries originate from various points around the corpus callosum and arrive at the nidus along its anteroinferior margins. Cortical branches from the MCA do not contribute to medial frontal AVMs. Drainage ascends to the SSS through the medial frontal veins, which may be the only sign of a medial frontal AVM at initial exposure. Cingulate AVMs and large medial AVMs have descending drainage to the pericallosal veins that empty into the ISS. Medial frontal AVMs are eloquent when they abut the motor strip in the paracentral lobule. Fig. 11.5 The medial frontal AVM: (a) medial, (b) anterior (with coronal cross section through the right hemisphere), and (c) coronal cross-sectional views. This AVM is located on the medial frontal surface, supplied exclusively by ACA branches, and drained by ascending medial frontal veins. The paramedian frontal AVM is a combination of lateral and medial frontal AVMs. The paramedian AVM occupies two surfaces at the medial corner of the frontal lobe, unlike the lateral and medial frontal AVMs that occupy just one (Fig. 11.6). The paramedian frontal AVM is visible on the lateral surface and on the medial surface after opening the interhemispheric fissure. The difference geographically between the medial and paramedian frontal AVMs is small. In order to transform a medial AVM into a paramedian AVM, one would pull the AVM up out of the interhemispheric fissure to gain additional representation on the lateral surface and enter the watershed between the MCA and ACA territories. In this spot, the paramedian AVM is supplied by two arterial territories, unlike the lateral and medial subtypes that are supplied by just one. Any of the four cortical MCA branches and any of the eight cortical ACA branches can feed the AVM, depending on its size and location in the anteroposterior plane. The paramedian nidus receives robust supply along two separate margins laterally and medially. Similarly, venous drainage is through both lateral and medial frontal veins that course to the SSS. Posteriorly located paramedian frontal AVMs are adjacent to eloquent motor areas. Fig. 11.6 The paramedian frontal AVM: (a) anterior (with coronal cross section through the right hemisphere), and (b) coronal cross sectional views. This AVM is located on both lateral and medial surfaces, supplied by both MCA and ACA branches, and drained by both lateral and medial frontal veins. Basal frontal AVMs are located on the basal frontal surface along the anterior cranial fossa floor (Fig. 11.7). They can be medial in the gyrus rectus and olfactory apparatus, or lateral in the orbital gyri. They can be anterior at the frontal pole or posterior adjacent to the anterior perforated substance. Basal frontal AVMs stay out of the interhemispheric and sylvian fissures, differentiating them from medial frontal and sylvian frontal subtypes, respectively. Like the paramedian frontal AVM, the basal frontal AVM receives a dual arterial supply from the MCA and ACA branches. OrbFrA and PreFrA from the MCA exit the sylvian fissure and travel to the AVM’s posterolateral border. OrbFrA and FrPolA from the ACA exit the interhemispheric fissure and travel to the AVM’s anteromedial border. Basal frontal AVMs also receive arterial input from unnamed A1 segment ACA branches that course over the olfactory tract and along the medial orbital gyrus to supply the AVM’s posteromedial border. Venous drainage is usually superficial to the SSS via an anterior OrbFrV or FrPolV, but occasionally may be deep to the BVR via OlfV or posterior OrbFrV. Basal frontal AVMs are located in non-eloquent cortex, but preservation of the patient’s smell, taste, and appetite requires careful handling of the olfactory apparatus and its blood supply. Although olfaction is not considered eloquent when grading AVMs, postoperative deficits are obvious to patients and impact their satisfaction with surgery. Fig. 11.7 The basal frontal AVM: (a) inferior (with left temporal pole removed), and (b) coronal cross-sectional views. This AVM is located on the basal frontal surface, supplied by both ACA branches (OrbFrA, FrPolA, and A1 segment perforators) and MCA branches (OrbFrA and PreFrA), and drained both superficially to the SSS and deep to the BVR. Fig. 11.8 The sylvian frontal AVM: (a) inferior (with left temporal pole removed), and (b) coronal cross-sectional views. This AVM is located on the sylvian surface of the frontal lobe in the pars orbitalis, pars triangularis, and/or pars opercularis as these gyri fold into the frontal operculum. Sylvian frontal AVMs are fed by M3 opercular branches and drained by sylvian veins, both superficial and deep. Sylvian frontal AVMs are based on the sylvian surface of the frontal lobe, facing the sylvian fissure and temporal lobe on the opposite side of the cistern (Fig. 11.8). The inferior frontal gyrus forms an inferior convolution that consists of the pars orbitalis, pars triangularis, and pars opercularis. Sylvian frontal AVMs are located in these gyri as they fold into the opercular surface of the frontal lobe. In contrast, lateral frontal AVMs are located in the inferior frontal gyrus above these convolutions, and basal frontal AVMs are located in the lateral or posterior orbital gyri anterior to pars orbitalis, neither of them with representation on the frontal operculum. Sylvian frontal AVMs are also different from insular AVMs, which lie deeper in insular cortex, medial to M2 segments of MCA. In contrast, sylvian frontal AVMs are deep to the M3 opercular segments that course along the frontal operculum, and are supplied by M3 branches. Cortical M4 arteries do not supply these AVMs unless they enter the nidus as they arrive at the cortical surface or double back to its superolateral margin. The ACA does not supply sylvian frontal AVMs. They drain through SupSylV, DeepSylV, or both. Pars opercularis and pars triangularis in the dominant hemisphere comprise Broca’s speech area, making these AVMs highly eloquent. Lateral frontal AVMs are convexity lesions that are among the easiest to expose (Fig. 11.9). A unilateral frontal craniotomy with the patient positioned supine and the head rotated to align the AVM box parallel to the neurosurgeon provides direct access to the cortical surface and circumferential access to the four sides (step 1). Sulcal dissection identifies the nidal margins, feeding arteries, and draining veins (step 2). Lateral frontal AVMs have dual drainage with ascending and descending venous systems. Draining veins are identified at the superior margin if ascending to the SSS, or at the inferior margin if descending to SupSylV or other anastomotic veins, with care devoted to the dominant vein (step 3). Feeding arteries from the superior trunk of the MCA are found along the frontal side of the sylvian fissure as they exit the fissure, making it unnecessary to split the fissure (step 4). These arteries are traced from the sylvian fissure to the nidus where they form an inferior front of cortical arteries (OrbFrA, PreFrA, PreCenA, and/or CenA) that joins the nidus at its inferior margin near the IFG (step 5). Parenchymal dissection preserves Broca’s area and motor strip, as well as deep white matter tracts containing corticospinal fibers (step 6). Deep dissection may extend to the frontal horn of the lateral ventricle where there may be an ependymal component of AVM (step 7). The lateral lenticulostriate arteries (lLSA) may also supply the deep plane and arterialize the nidus until the end to the dissection. These perforators are often difficult to visualize and cauterize, requiring AVM retraction and microclips (Figs. 11.10 and 11.11). Fig. 11.9 Resection strategy for lateral frontal AVMs. (a) Step 1, exposing the AVM with a unilateral frontal craniotomy [surgeon’s view, with scalp incision (dashed line), craniotomy (solid line), and AVM (purple circle) shown on inset]. (b) AVM box showing arterial inputs from the MCA branches, superficial venous drainage to the SSS, and proximity to Broca’s area (yellow) and motor cortex (red). Note that the AVM’s cortical surface is depicted with a circle on its base side and that side’s label underlined. The AVM’s axis is depicted with a line through the box. Arterial and venous anatomy is superimposed on the box with red inflow arrows and blue outflow arrows, respectively. (c) Step 2, dissecting margins in the lateral frontal sulci (broad white arrow); step 3, identifying ascending convexity veins; step 4, locating cortical MCA feeders; and step 5, interrupting the inferior front of arteries near the MFG (dashed black line), with care to preserve en passage flow in transit arteries (PreCenA, surgeon’s view). (d) Step 6, circumdissecting into frontal parenchyma (encircling arrows, coronal cross-sectional view). (e) Step 7, mobilizing the AVM (spherical scoop) to expose lenticulostriate artery feeders on inferior side.
 Microsurgical Anatomy
Microsurgical Anatomy
Brain
Arteries
Veins
 Five Frontal AVM Subtypes
Five Frontal AVM Subtypes
The Lateral Frontal AVM
The Medial Frontal AVM
The Paramedian Frontal AVM
The Basal Frontal AVM
The Sylvian Frontal AVM
 Frontal AVM Resection Strategies
Frontal AVM Resection Strategies
Lateral Frontal AVM Resection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Frontal Arteriovenous Malformations