Higher Cortical Functions: Introduction
The human cerebral cortex represents, in some ways, the pinnacle of evolution. In addition to containing networks of neurons related to the initiation of movement and to sensation from the body and the special sensory organs, the cortex is the substrate for functions that include comprehension, cognition, communication, reasoning, problem-solving, abstraction, imagining, and planning.
Frontal Lobe Functions
The frontal lobes contain phylogenetically “new” parts of the cortex, and serve as an “executive” part of the cortex. They participate in higher order functions that include reasoning and abstraction; planning and initiating of activity; monitoring and shaping of behavior to ensure adaptive actions; inhibiting maladaptive behavior; prioritizing and sequencing actions; problem solving; and coordinating elementary motor and sensory functions into a coherent and goal-directed stream of behavior.
Damage to the frontal lobes (as can occur, eg, with brain tumors or head trauma) can produce profound behavioral changes. Several syndromes are especially common: Following damage to the dorsolateral part of the frontal lobes (the convexity), patients tend to become indifferent, abulic, or apathetic (mute and motionless in some cases). Following damage to the orbitofrontal area of the cortex, there is a syndrome of disinhibition, in which the patient appears labile and irritable. These patients are inattentive and distractible, with impaired judgment and loss of the usual inhibitions and social graces. Damage to the medial part of the frontal lobes can produce a syndrome of akinesia (lack of spontaneous movements) and apathy. Injury to the basal part of the frontal lobes can also result in impairment of memory. These frontal lobe syndromes are more frequently seen in patients with bilateral lesions.
Language and Speech
Language is the comprehension and communication of abstract ideas. This cortical function is separate from the neural mechanisms related to primary visual, auditory, and motor function.
The ability to think of the right words, to program and coordinate the sequence of muscle contractions necessary to produce intelligible sounds, and to assemble words into meaningful sentences depends on Broca’s area (areas 44 and 45) within the inferior frontal gyrus, located just anterior to the motor cortex controlling the lips and tongue.
The ability to comprehend language, including speech, is dependent on Wernicke’s area. This area is located in the posterior part of the superior temporal gyrus within the auditory association cortex (area 22).
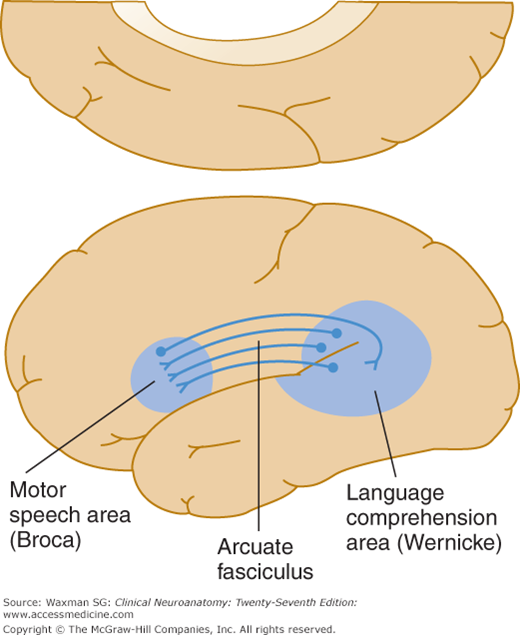
The arcuate fasciculus provides a crucial are-shaped pathway within the hemisphere white matter, connecting Wernicke’s and Broca’s areas (Fig 21–1). Because the arcuate fasciculus connects the speech comprehension area (Wernicke’s area) with the area responsible for production of speech (Broca’s area), damage to this white matter tract produces impairment of repetition.
Dysarthria is a speech disorder in which the mechanism for speech is damaged by lesions in the corticobulbar pathways; in one or more cranial nerve nuclei or nerves V, VII, IX, X, and XII; in the cerebellum; or in the muscles that produce speech sounds. Dysarthria is characterized by dysfunction of the phonation, articulation, resonance, or respiration aspects of speech.
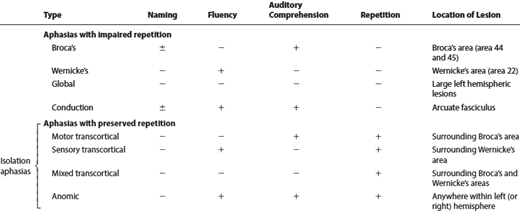
Aphasia refers to loss or impairment of language function as a result of brain damage. There are a number of distinct types of aphasia and most of these result from lesions in specific regions of the cerebral hemispheres (Table 21–1). In testing for aphasia, the clinician first listens to the patient’s spontaneous speech output and then explores the patient’s speech during conversation. Speech may be categorized as fluent (more than 50 words per minute, effortless, absence of dysarthria, normal phrase length, and normal intonation). In contrast, nonfluent aphasia is effortful, with decreased verbal output (less than 50 words per minute), poor articulation, degradation of inflection and melodic aspects of speech, and agrammatism (ie, the tendency to omit small, grammatical words, verb tenses, and plurals and to use only nouns and verbs). Naming (which is usually examined by asking patients to name objects presented to them), repetition of phrases such as “dog,” “automobile,” “President Kennedy,” “no ifs, ands, or buts,” and comprehension of spoken language are also tested. Comprehsion can be assessed in patients with impaired speech output by observing the response to yes-no questions of graded difficulty (“is your name John?” “Are we in a hospital room?” “Are we in a church?” “Do helicopters eat their young?”)
In most common forms of aphasia, the ability to repeat spoken language is impaired. Broca’s, Wernicke’s, and global aphasia are frequently seen in clinical practice.
Broca’s aphasia is common, and is usually caused by a lesion in the inferior frontal gyrus in the dominant hemisphere (Broca’s area; Fig 21–1). The patient has difficulty naming even simple objects. Repetition is impaired, but comprehension of spoken language is normal. The patient is usually aware of the deficit and appropriately concerned about it.
Most lesions that involve Broca’s area also involve the neighboring motor cortex. Patients are often hemiplegic, with the arm more affected than the leg. Broca’s aphasia often occurs as a result of strokes, most commonly affecting the middle cerebral artery territory.
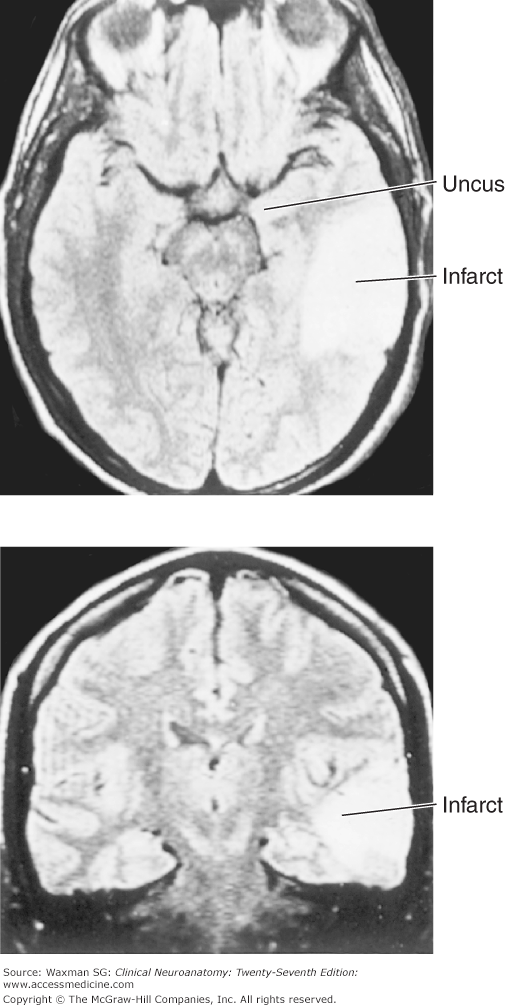
This common form of aphasia is caused by a lesion in or near the superior temporal gyrus, in Wernicke’s area (see Figs 21–1 and 21–2). Because this part of the cortex is not located adjacent to the motor cortex, there is usually no hemiplegia.
Figure 21–2
Magnetic resonance images of sections through the head. Top: Horizontal section with a large high-intensity area in the temporal lobe, representing an infarct caused by occlusion of a middle cerebral artery branch. Bottom: Coronal section showing the same area of infarction. (Parallel lines on the periphery of the brain represent artifacts caused by patient motion.) Large infarcts of this type, in the dominant cerebral hemisphere, can produce global aphasia that is accompanied by hemiparesis.
Patients with Wernicke’s aphasia have fluent speech, but repetition and comprehension are impaired. The patient usually has difficulty naming objects and produces both literal paraphasias (eg, “wellow” instead of “yellow”) and verbal paraphasias (eg, “mother” instead of “wife”). Neologisms (meaningless, nonsensical words, eg, “baffer”) are used commonly and speech may be circumlocutory (ie, wordy but meaningless). Patients with Wernicke’s aphasia usually do not appear concerned about, or even aware of, their speech disorder. Wernicke’s aphasia commonly occurs as a result of embolic strokes.
Large lesions in the dominant hemisphere, which involve Broca’s area in the frontal lobe, Wernicke’s area in the temporal lobe, and the interconnecting arcuate fasciculus, can produce global aphasia (see Fig 21–2). In this nonfluent aphasia, both repetition and comprehension are severely impaired. Global aphasia most commonly occurs as a result of large infarctions in the dominant hemisphere, often because of occlusion of the carotid or middle cerebral artery.
In this unusual aphasia, verbal output is fluent and paraphasic. Comprehension of spoken language is intact, but repetition is severely impaired. Naming is usually impaired, although the patient often is able to select the correct name from a list. Conduction aphasia is a result of a lesion involving the arcuate fasciculus, in the white matter underlying the temporal–parietal junction; this lesion disconnects Wernicke’s area from Broca’s area.
In these unusual aphasias, repetition is spared, but comprehension is impaired. These aphasias are also referred to as transcortical aphasias because the lesion is usually in the cortex surrounding Wernicke’s or Broca’s area, or both. Depending on the location of the lesion, these aphasias may be fluent or nonfluent and comprehension may be impaired or preserved.
Anomia (difficulty finding the correct word) can occur in a variety of conditions, including toxic and metabolic encephalopathies. When anomia occurs as an aphasic disorder, speech may be fluent but devoid of meaning as a result of word-finding difficulty. The patient has difficulty naming objects. Comprehension and repetition are relatively normal. The presence of anomic aphasia is of little value in localizing the area of dysfunction. Focal lesions throughout the dominant hemisphere or, in some cases, in the nondominant hemisphere, can produce anomic aphasia, and anomia is also commonly present in toxic and metabolic encephalopathies.
Alexia (the inability to read) can occur as part of aphasic syndromes or as an isolated abnormality. Aphasic alexia refers to impaired reading in Broca’s, Wernicke’s, global, and isolation aphasias.
This disorder, in which there is impairment of reading and writing, is seen with pathologic lesions at the temporal–parietal junction area, particularly the angular gyrus. Because lesions of the angular gyrus also produce Gerstmann’s syndrome (see later section in this chapter) and anomia, the constellation of agraphia, Gerstmann’s syndrome, and anomia may occur together.
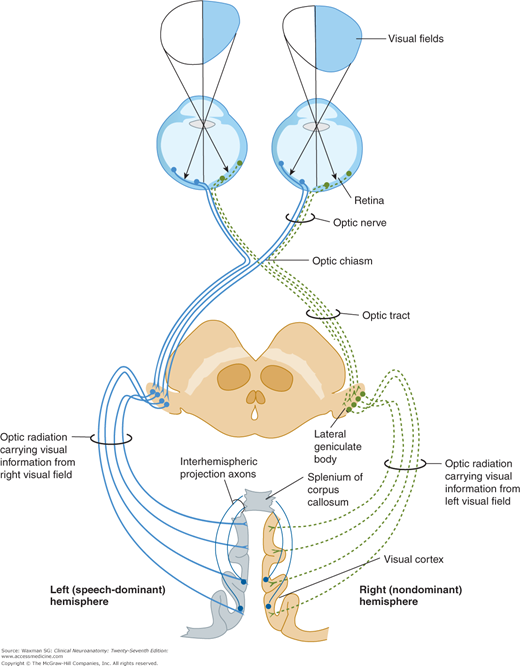
Alexia without agraphia is a striking disorder in which the patient is unable to read, although writing is not impaired. Patients with this disorder are capable of writing a paragraph but, when asked to read it, cannot do so.
This syndrome occurs when there is damage to the left (dominant) visual cortex and to the splenium of the corpus callosum (Fig 21–3). As a result of damage to the left visual cortex, there is a right-sided homonymous hemianopsia and written material in the right half of the visual world is not processed. Written material presented to the left visual field is processed in the visual cortex on the right side. However, neurons in the visual cortex on the two sides are normally interconnected via axons that project through the splenium. As a result of damage to the splenium, visual information in the right visual cortex cannot be transmitted to the visual cortex in the left (dominant) hemisphere and, thus, is disconnected from the speech comprehension (Wernicke’s) area.