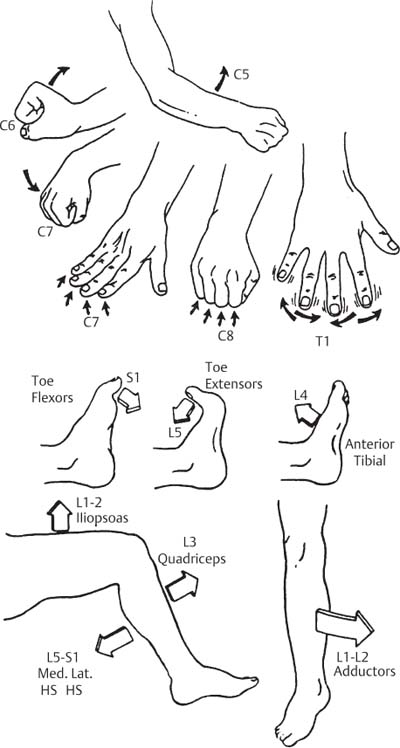
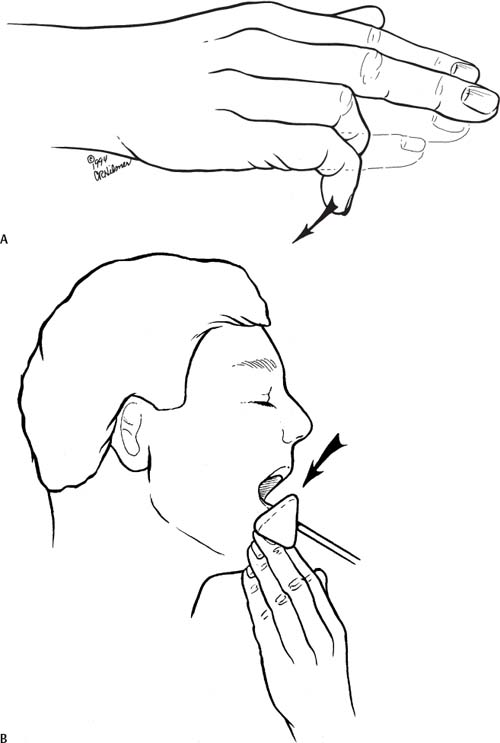
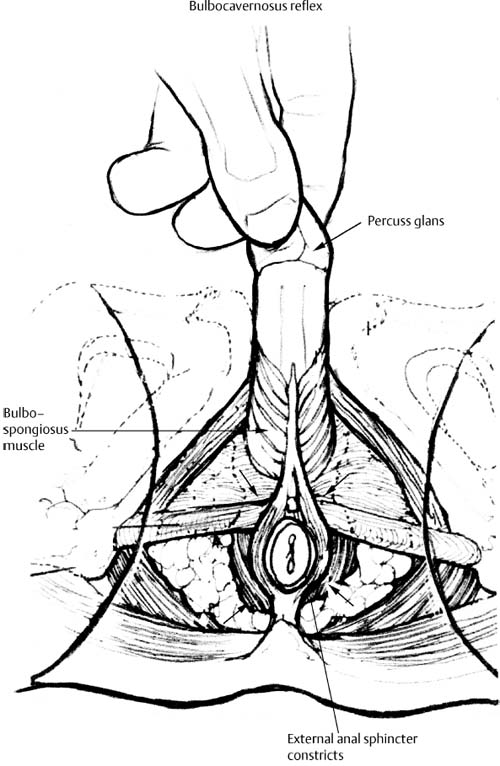
2 I. Degenerative disorders of the spine A. History is the most important component of the patient evaluation. 1. Establishes the initial differential diagnoses 2. Guides physical examination and selective diagnostic tests B. Spinal pain can be described as 1. Mechanical versus nonmechanical a. Mechanical pain tends to be associated with activity. (1) Relieved by rest (2) Progressively worse over the course of the day b. Nonmechanical pain is typically due to tumors and/or infections. (1) Independent of activity (2) Worse at night (3) Not relieved by rest or immobilization 2. Axial versus radicular a. Axial pain is usually diffuse. (1) Referred pain to the scapula or shoulder in cervical spine disorders (2) Buttock or posterior thigh in lumbar spine disorders b. Radicular pain is typically associated with paresthesia, numbness, or weakness in a dermatomal distribution (Fig. 2–1). (1) Associated with tension signs (Table 2–1) Figure 2–1 Motor examination for cervical and lumbar nerve roots. Figure 2–2 Myelopathic motor examination findings. (A) Finger escape sign. (B) Jaw-Jerk REflex. (C) Hoffman’s sign. (D) Babinski’s sign. (from An HS. Principles and Techniques of Spine Surgery. Baltimore: Williams and Wilkins; 1998. Reprinted with permission.) C. Myelopathy (Fig. 2–2) 1. Presents with poorly characterized pain a. Vague sensory and motor symptoms over a long period of time are also common. 2. Associated with neck, arm, or leg pain in a nondermatomal pattern or with pain in a cervical dermatome 3. Slow and broad-based gait 4. Problems with upper extremity fine motor functions a. Difficulty with fastening buttons is noted early. b. Lower extremity dysfunction and spasticity c. Bowel and bladder dysfunction noted later. 5. Associated with pathological long tract signs (Table 2–2)
History and Physical Examination
♦ History
| Cervical Tension Signs | Findings |
| Spurling’s | Neck extension and rotation toward the painful side causes radicular limb pain. |
| Compression | Axial loading on the head reproduces pain. |
| Distraction test | Skull traction relieves pain. |
| Shoulder Abduction | Elevation of painful limb relieves pain. |
| Lumbar Tension Signs | Findings |
| Lasegue [Straight leg raise (SLR)] | Elevation of painful limb causes radicular limb pain, not back pain. Pain should be reproduced with less than 60 degrees of hip flexion. |
| Bowstring | After reproducing the patient’s pain and obtaining a positive Lasegue’s sign, the knee is flexed. This is positive if the patient’s pain resolves with flexion of the knee. |
| Frajersztajn (Contralateral SLR) | Elevation of the nonpainful limb cause back and limb pain on the opposite side (usually means sequestered or large extruded herniated disk). |
| Femoral stretch (Reverse SLR) | Hip extension in either the lateral decubitus or prone position stretches the femoral nerve and reproduces pain in the L3 or L4 distribution. |
II. Traumatic disorders
A. The ABC (airway, breathing, and circulation) should be checked first in any trauma patient.
B. The mechanism of injury should be sought.
C. Pain and neurological symptoms should be documented.
III. Spinal deformity
A. Deformity and pain are the two most common presenting complaints.
1. Pain is a more ominous sign in the child.
a. Possible etiologies include
(1) Spinal cord or bony tumor
(2) Scheuermann’s disease
(3) Spondylolisthesis
2. In adults, pain associated with deformities tends to be present at the convexity.
a. Due to muscle fatigue early
b. Localizes to the concavity when degenerative changes have occurred later
B. Medical history, family history, onset of menarche, time of curve detection, and progression should be obtained in the adolescent scoliotic patient.
♦ Physical Examination
I. Inspection
A. Look for obvious deformities in both the coronal and sagittal plane
1. Coronal plane
a. Scoliosis evaluated by a plumb line dropped from the seventh cervical vertebra
b. Pelvic obliquity
c. Shoulder imbalance
d. Scapular protuberance
e. Rib prominence
2. Sagittal balance and regional deformities
a. Normal cervical lordosis: 20 to 40 degrees
b. Normal thoracic kyphosis: 20 to 45 degrees
c. Normal lumbar lordosis: 40 to 60 degrees
B. Look for skin or subcutaneous lesions
| Long Tract Sign/Reflex | Findings/Provocative Maneuver |
| Lhermitte’s | Neck flexion causes electric shock sensation or paresthesias radiating into the upper and lower extremities. |
| Finger escape | Ask the patient to keep the fingers in full extension and the ulnar digits tend to abduct. |
| Jaw jerk | Hyperreflexia on tapping the jaw suggests an upper motor neuron lesion at the level of the brain stem. Involves the masseter and temporalis muscles and the fifth cranial nerve. |
| Shimizu (scapulohumeral) | Tapping the tip of the spine of the scapula and the acromion elicits elevation of the humerus. Reflex suggests spinal cord compression at the upper cervical region. |
| Inverted radial | Tapping of the brachioradialis tendon causes spastic finger flexor contraction instead of normal extension of the wrist. Positive reflex suggest spinal cord compression at the C6 region. |
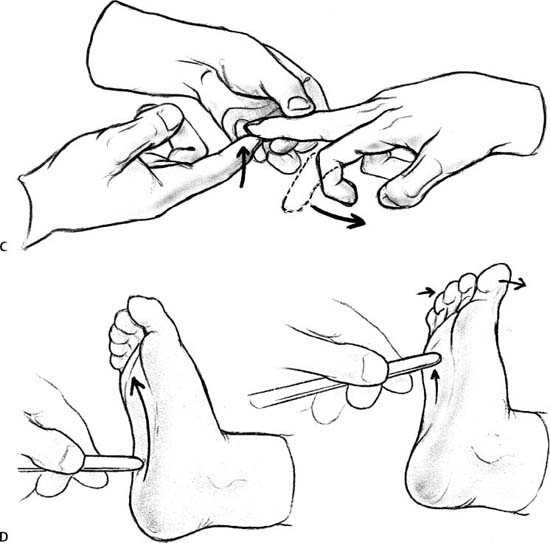
| Hoffman’s | Holding the middle finger extended and suddenly extending the Distal Interphalarged Joint (DIP) will produce finger and thumb flexion. |
| Babinski | Gentle stimulus applied to the lateral aspect of the sole of the foot starting over the heel extending toward the fifth digit. A positive Babinski’s sign refers to the initial dorsiflexion of the great toe upward and the spreading of the other toes. |
| Clonus | Rhythmic, nonvoluntary movements of the muscle with firm passive continuous stretch. |
1. Café au lait spots in neurofibromatosis patients
2. Midline tufts of hair, dimples, or rosy spots may indicate occult spinal dysraphism.
C. Muscle atrophy should be observed in neurologically impaired patients.
II. Palpation
A. Bony palpation
1. Spinous processes
2. Posterior superior iliac spines: “dimples”
3. Scapula and ribs
4. Iliac crests
5. Sacrum and coccyx
6. Trochanter and ischial tuberosity
B. Soft tissue palpation for spasm or trigger point tenderness
1. Trapezius muscle
2. Rhomboid/levator muscles
3. Paravertebral muscles
4. Gluteus muscles
5. Piriformis muscle
6. Sciatic nerve
III. Range of motion
A. Cervical spine
1. Flexion: 45 degrees (the chin touches the chest)
2. Extension: 75 degrees
3. Lateral bending: 40 degrees
4. Rotation: 75 degrees
B. Thoracolumbar spine
1. Flexion: 80 degrees (measure the distance from the tip of hands to the floor)
2. Extension: 40 degrees
3. Lateral bending: 40 degrees
4. Rotation: 45 degrees
IV. Neurological examination of individual roots
A. Sensory tests
1. Four distinct sensations with defined anatomic pathways in the spinal cord
a. Pain perception may be tested with defined anatomic pathways in the spinal cord.
b. Light touch may be tested with a cotton swab.
c. Temperature may be tested with two test tubes containing either a hot or cold solution.
d. Proprioception begins distally at the distal phalanx or great toe and proceeds proximally to each larger joint.
2. The aim of sensory testing is to identify whether there is a dermatomal pattern of sensory dysfunction, which would suggest spinal root pathology, or a possible glove/stocking distribution that would suggest a neuropathy (Table 2–3).
| Nerve Root | Dermatomal Distribution |
| C5 | Upper outer arm |
| C6 | Thumb |
| C7 | Long finger |
| C8 | Little finger |
| T1 | Medial forearm |
| T4 | Nipple |
| T10 | Umbilicus |
| L1 | Groin |
| L2 | Anterior thigh |
| L3 | Knee |
| L4 | Medial malleolus |
| L5 | Great toe |
| S1 | Small toe |
| S2 | Posterior thigh |
| S3–S5 | Anal |
B. Motor tests (Fig. 2–3)
1. Muscle strength
a. Grade 5: normal
b. Grade 4: weak against resistance
c. Grade 3: motion against gravity
d. Grade 2: motion with gravity eliminated
e. Grade 1: evidence of contractility
f. Grade 0: no evidence of contractility
2. Motor root testing/reflexes (Table 2–4)
V. Special provocative tests
A. Adson’s test
1. Test to evaluate thoracic outlet syndrome
2. Abduct, extend, and externally rotate the arm, while feeling the radial pulse. Also rotate the head toward the testing arm.
a. If the pulse disappears with reproduction of symptoms, the test is positive.
B. Sacroiliac tests
(1) Patrick’s test: flexion, abduction, and external rotation of the hip cause pain referred from the sacroiliac joint.
(2) Gaeslen’s test: dropping the leg on the table (extension of the hip) causes pain in the ipsilateral sacroiliac joint.