Fig. 1.1
Transpedicular decancellization and closure of wedge
Purpose of this chapter is to summarize, and history review the common spinal osteotomy techniques utilized in complex spine deformity by details of techniques, indication, and related complication.
1.1 Surgical Techniques
1.1.1 Smith-Petersen Osteotomy
SPOs was first described in 1945 by Smith-Petersen and used principally for kyphosis deformity of ankylosing spondylitis. Subsequently, concepts of doing multiple SPOs have been useful for treatment of ankylosing spondylitis and iatrogenic fixed sagittal imbalance [7, 8].
1.1.1.1 Technical Details
Classical SPO is described as the resection of two or multisegments posterior elements between the facet joints, shorten posterior column and lengthen anterior column through disc open by forceful manual extension, then to acquire spine lordosis (Fig. 1.2).
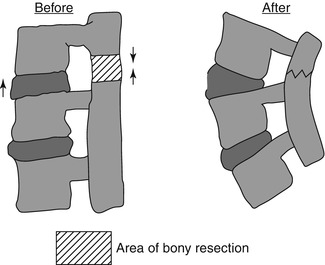
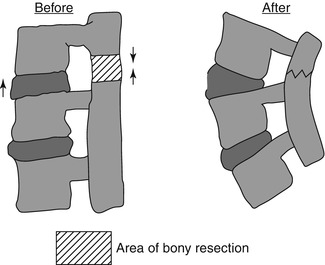
Fig. 1.2
Smith Petersen osteotomy: anterior open and closure of posterior wedge
Osteotome or high-speed bur can be used to remove the spinous process, edges of lamina, synostosed articular processed in a V-shape fashion and Kerrison punch for ligamentum flavum (Fig. 1.1). After rod implant, shorten posterior column can also be accomplished by combination of cantilever maneuvers and compressed forceps between pedicle screws or spinous processes, especially in osteoporosis circumstances. This manipulation can cause disruption of the anterior longitudinal ligament and thus create an anterior monosegmental intervertebral opening wedge.
La Chapelle [9] in 1946 described a two-stage anterior opening wedge osteotomy for correction of thoracic–lumbar kyphosis in one case of AS [9]. He first removed the L2 lamina under local anesthesia and two weeks later by an anterior release and resection of the intervertebral L2/3 disc. The anterior osteotomy was then wedged open and grafted with a structured bone.
Many modifications of this opening wedge osteotomy have been described. Discectomy and transfacet intervertebral fusion can be combined SPO. Briggs et al. [10] and Wilson and Turkell [11] reported a posterior wedge osteotomy with bilateral intervertebral foraminotomy. This method modified SPO to a gradual correction without rupturing of the anterior longitudinal ligament. Posterior closing wedge osteotomy was also described in 1984 by Alberto Ponte for the treatment of flexible Scheuermann’s kyphosis in skeletally mature patients [12], which is lesser bone resection compared with SPO and more indicated in Scheuermann’s kyphosis and adolescent idiopathic scoliosis. So the main differences of SPO and posterior wedge osteotomy (Ponte osteotomy) are the degree of posterior element resection, corrective ability, and indicated pathology (Fig. 1.3).
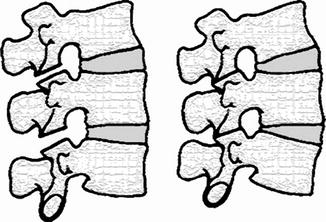
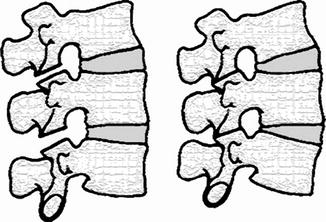
Fig. 1.3
Ponte osteotomy: partial fact resection and wedge osteotomy
Generally with each SPO, a 10–15° per segment can be expected by 10 mm resection through a mobile and adequate height disc. It is important to note the power of this osteotomy is limited by the degree of anterior ossification and it may be beneficial to choose a more cranial level.
Some surgeons consider the SPO can be modified as more radical posterior column resection and anterior osteoclasis to achieve approximately 30° of correction in one level, especially as in an ankylosing spondylitis patient. Logically this procedure seemed to acquire more corrective angles by only one segment, but which can cause dangerous spine kinking and ventral vessels complications.
Every spine osteotomy surgery needs to investigate the fusion and longstanding results. SPO osteotomy is primarily designed for kyphosis deformity of AS, especially as patient has a bony fusion ability. So in most of circumstances, anterior gap of SPO can be a satisfied spine fusion results. Anderson lesion or pseudarthrosis is also a common pathology for AS which caused pain, kyphosis, or even neurological symptoms due to fibro-osseous tissue proliferation around the site of the lesion. Standard procedure for pseudarthrosis seems to be an anterior fusion. Chang described his experiences of using SPO osteotomy and without anterior fusion tech in 30 cases of AS patients [13]. All patients had no evidence of nonunion on X-ray at the level of the pseudarthrosis at final follow-up (average 4.7 years, range 2.2–9.1 m). None had a notable loss of correction. For absence of anterior structured supporting, SPO has a potential loss of correction. In a compared study of SPO and PSO method for AS patients, Zhu Z [14] reported the mean loss of correction of >5° occurred in 4 cases (21.1 %) in SPOs group and 5 cases (16.1 %) in PSO group.
1.1.1.2 Indication
A long, rounded, smooth kyphosis, such as Scheuermann’s, idiopathic kyphosis, especially with a previous fusion and malunion, is often an ideal candidate for multiple SPOs. Minor kyphosis deformities <30° are also candidate for SPO. Typically SPO is performed in the thoracic spine. In addition, multiple Smith-Petersen osteotomies can be done throughout the thoracic and lumbar spine to achieve the desired correction [15]. Clinically, SP osteotomy offers unique advantages. In comparison to the historic standard of anterior and posterior combined approach and pedicle subtraction osteotomies, Smith-Petersen osteotomies offer stable fixation and deformity correction with less blood loss, less operative time, and fewer complications [16].
1.1.1.3 Complications
The length of anterior column by SPO has caused major complications, including paraplegia from spinal kinking and cauda equina compression and abdominal vessels injury from stretching of anterior column length. Although V-shape osteotomy provides rotation control, canal and nerve root compromise should be prevented while there is a scoliosis over 40°, for cantilever maneuver can push spine into concavity. It should be cautioned that although aggressive posterior decompression can acquire correction more than 10° in one SPO level, it is susceptible to occur a spine column sagittal translation which can cause cord compromise. Chang et al. indicated [17] that ST is a basic mechanism for correcting sagittal imbalance and is likely to occur when the level of OWO is near the apex of deformity.
1.1.2 Pedicle Subtraction Osteotomy
Scudese and Calabro in 1963 [20] and later by Ziwjan in 1982 [21] and Thomasen in 1985 [22] described the three-column posterior osteotomy for the management of fixed sagittal plane deformities in patients with ankylosing spondylitis. Typically, pedicle subtraction osteotomy is performed at either L2 or L3, as these vertebrae are the normal apex of lumbar lordosis and safer for that they are caudal to the conus medullaris (Fig. 1.4).
Fig. 1.4
Pedicle substraction osteotomy
1.1.2.1 Technical Details
The technique involves a transpedicular vertebral wedge resection extending from the posterior elements through the pedicles and into the anterior cortex of the vertebral body. When the middle and posterior column bone defects are closed, the length of the anterior vertebral cortex remains unchanged (Fig. 1.3).
As PSO is a three-column osteotomy, stability of spine column may be lost abruptly during the process of osteotomy. To obviate this complication, pedicle screws should be placed into the cephalad and caudad vertebral of the intended osteotomy site. The pedicle of osteotomy vertebral also can be prepared with pedicle awl for later location of pedicle. Osteotomy maneuver begin with removing all of the posterior elements (spinous process and lamina). When the pedicles are isolated, cancellous bone from the vertebral body can be removed or decancellation through the pedicles while protecting the dura and nerve roots. Bleeding from the vertebral body and canal can be reduced by hemostatic agent, such as Avitene, to help control blood loss. When performed in the thoracic spine, partial rib resection may be required to gain access to the vertebral body without retracting the spinal cord. Once adequate cancellous bone has been removed, an osteotomy is then done through the lateral walls of the vertebral body, inferior wall of pedicle adjacent to the exiting nerve root and finally the posterior cortex of the vertebral body, which means a 360° circumferentially osteotomy.
Careful attention is needed to ensure that the removal of bone is uniform, which will produce asymmetric closure of the osteotomy site. Asymmetric PSO also can be utilized as a method for sagittal combined coronal plane deformity [23]. Sagittal translation sometimes occurs for the asymmetric osteotomy or cantilever maneuvers, which can cause catastrophic dura impinging. Bridwell et al. suggested creating central enlargement in the lamina to inspect the thecal sac and nerve roots to make sure that nothing impinges on them (Fig. 1.4) [14]. The dura and nerve root above and below the pedicle resected should be freed. The osteotomy site can be closed with use of temporary rods cantilevering the spine and also by extension the chest and legs with the operating table. In some instances, hinge points are not located in the anterior column, thus a cage can be positioned or a second-staged anterior column grafting is reconstructed.
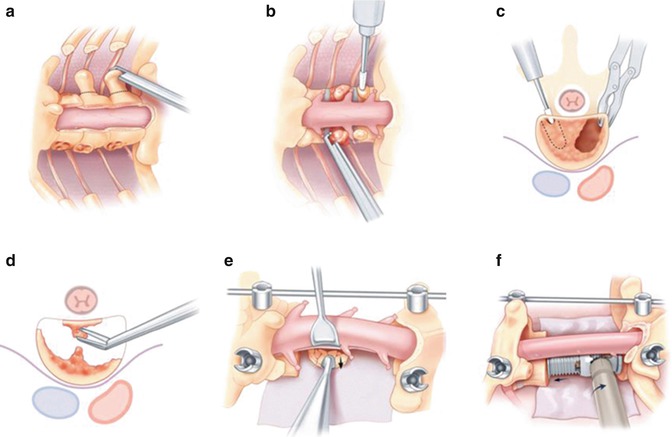
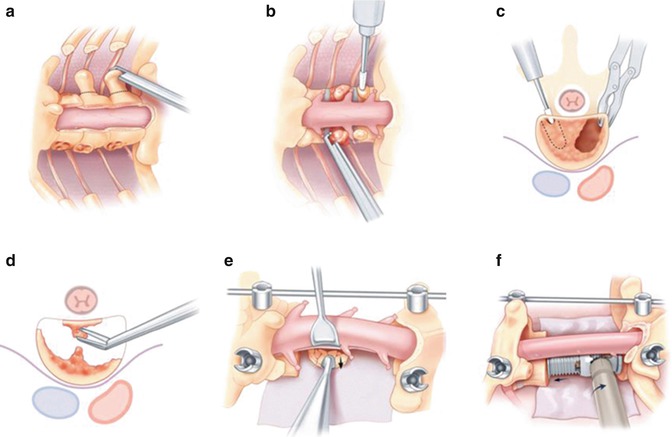
Fig. 1.5
Reprint with permission from Justin et al. [53]. (a) posterior element removed, (b) pedicle isolated, (c) transpedicle cancellous bone removed, (d) posterior wall bone removed, (e) packed posterior wall cortex, (f) vertebral column reconstructed
Compared with the SPO method, PSO technique is shortened posterior and middle column without lengthening of the anterior column, thus shortening the spinal canal. On the average, the pedicle subtraction osteotomy can achieve approximately 30–40 of lordosis at each level at which the osteotomy is performed [24, 25]. A 6–13.5 cm of SVA correction is also anticipated [26]. Bone quality is prerequisite for an effective segmental instrumentation.
1.1.2.2 Indications
Pedicle subtraction osteotomies are indicated for short angular deformities, severe global positive sagittal imbalance >6 cm, concomitant coronal deformity, or in cases with multilevel circumferential fusion precluding Smith-Petersen osteotomy. Examples include posttraumatic kyphotic collapse, degenerative scoliosis, postinfectious kyphosis, iatrogenic flatback syndrome, or ankylosing spondylitis.
1.1.2.3 Complications
Although PSO offers more corrective advantages than SPO in one segment, it is not a panacea for all spinal deformity. Extensive bleeding lost >2 l with this procedure can cause complications in frequently debilitated patients [27]. Pseudoarthrosis is another complication associated with long spinal fusions and osteotomies. Although none occurred at the osteotomy site, Bridwell reported a 24 % pseudoarthrosis rate in a long-term follow-up of pedicle subtraction osteotomies for fixed sagittal imbalance in a prospective study [28]. Many authors suggest augmenting fusions with anterior interbody fixation or staged anterior plating to prevent this complication [29].
Neurologic complications following a pedicle subtraction osteotomy are unfortunately common. In a similar retrospective review of 83 consecutive patients with fixed sagittal imbalance treated with a spinal osteotomy, Ahn et al. [30] found a 12.0 % incidence of neurologic deficits. Bridwell published a neurological complication rate of 15.2 % of a series of 33 consecutive patients treated by PSO osteotomy [28]. Buchowski et al. presented a long-term follow-up of 108 patients and noted deficits in 11.1 % of patients and 3 patients had permanent deficits [31]. All authors discuss dural buckling, dorsal impingement, and posterior subluxation or sagittal translation as potential causes of neurologic compromise. Ahn recommends a wide central decompression and the use of a Stagnara wake-up test or intraneuromonitor, especially Spontaneous EMG to detect any of these injuries. A recent report highlighted a 67 % sensitivity and 98 % specificity of using multimodal monitoring in these patients [32].
1.1.3 Vertebral Column Resection
Vertebral column resection was first described by MacLennan [33] in 1922 as a vertebrectomy from posterior only approach for treatment of severe scoliosis. In 1983, Luque reported another vertebrectomy method by anterior fenestration [34]. Later Boachie reported combined approach for vertebrectomy and Luque instrumentation for multiplanar deformity [35]. As the most powerful tool for the correction of spinal deformity, vertebral column resection is generally reserved for severe fixed sagittal and coronal imbalance. With the evolution of posterior approach, some author challenged the posterior—only approach for vertebrectomy. And due to its technical difficulty and potential for complications, Suk et al. [36] called this procedure a “formidable last resort technique for the most tenacious spinal deformities.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








