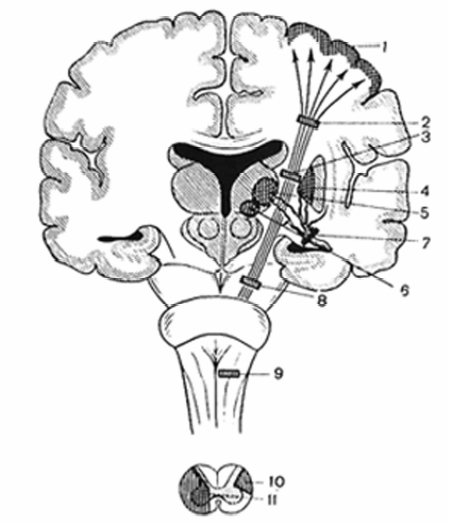
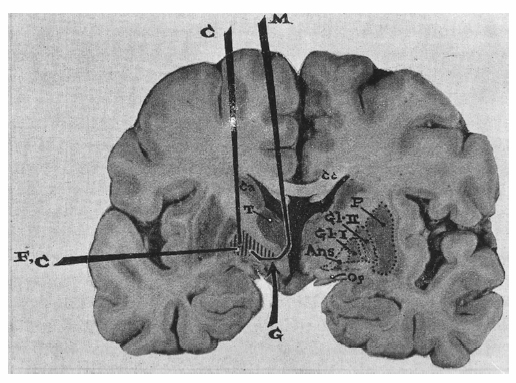
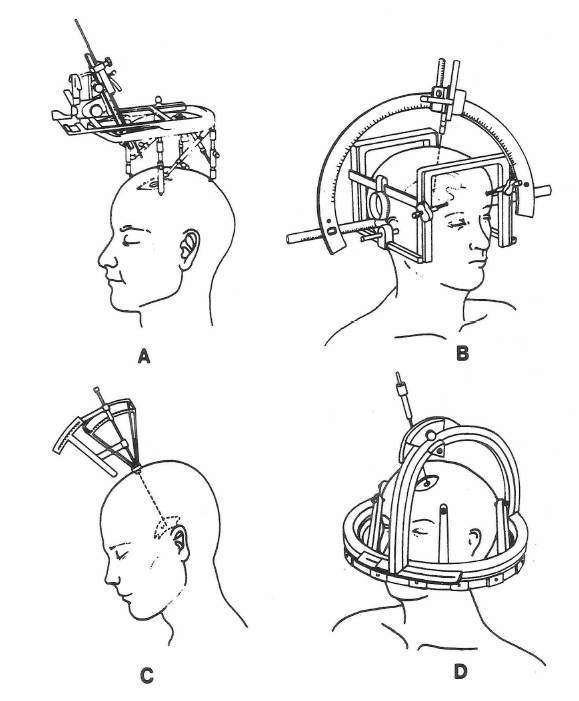
1 History of Surgery for Movement Disorders Philip L. Gildenberg The history of surgery for movement disorders can be divided into five stages: the prestereotactic era (1890–1954), the early stereotactic era prior to the introduction of L-dopa (1947–1968), the latent period (1968–1992), reintroduction of ablative stereotactic surgery (1992–1999), and the use of implanted stimulators (1997–present). There is overlap between the various periods, particularly between the first two, because open ablative, resection craniotomy, or laminectomy was performed for several years until stereotactic surgery had time to demonstrate its superiority, by both improved results and safety. Not much happened for several years after the introduction of L-dopa, around 1968, until it became well established that medication was not the ultimate answer for Parkinson disease (PD). Reports of success of pallidotomy were reintroduced. The patients, however, were different from those in the first stereotactic phase because they were much later in their disease and had the complications of the medication added to their parkinsonian symptoms. The use of implanted stimulators for movement disorders was introduced gradually. Original observations were made as early as 1980, but it was not until 1998 that deep brain stimulation for movement disorders became common in Europe. In 2001 it was approved for widespread use in the United States. Even so, ablation procedures are still performed for various reasons, not the least of which is economic. The groundwork for surgery for movement disorders began in the last part of the nineteenth century. The concept of localized activity of the cerebral cortex was based on electrical stimulation studies such as those of Fritsch and Hitzig1 and such clinical observations as Jackson’s2 observation of a loss of motor or sensory function associated with cerebral lesions and Broca’s3 similar observation of a loss of speech. The functions of the basal ganglia were not well appreciated because of the difficulty in experimental manipulation of such subcortical structures. The father of functional neurosurgery was also the father of the scientific approach to surgery for movement disorders, Sir Victor Horsley. As early as 1890, he performed extirpation of the motor cortex for treatment of athetosis.4 In 1909, he obtained relief of postscarlatina hemiathetosis in a 15-year-old boy by resecting the upper-extremity portion of the contralateral precentral gyrus, but paresis and dyspraxia ensued.5 In subsequent reports6 he acknowledged improvement in other types of movement disorders, but at the expense of paralysis or severe paresis, which usually improved gradually, often as the abnormality returned. In the absence of other treatment, however, it was considered to be a reasonable trade-off to exchange paresis for involuntary movements despite a mortality rate of up to 15%. One might speculate that it was his frustration at these imperfect results that led him to physiological experiments on subcortical structures. In 1908, he and Clarke reported on physiologic observations following production of lesions in the dentate nucleus of the monkey.7 This paper is a classic in every sense and should be read in the original by anyone interested in the history of stereotactic surgery. The literary quality of the writing is rarely seen in scientific publications today. After defining the need for more information about the connections between cerebellum and cortex, the authors state, “An essential preliminary, therefore, to further progress was to find some method which would satisfy these conditions, viz., a means of producing lesions [of the cerebellar nuclei] which should be accurate in position, limited to any desired degree in extent, and involving as little injury as possible to other structures.” This remains the goal of stereotactic surgery even today. The paper has four sections. “Rectilinear topography” describes how they created the first stereotactic atlas by sectioning the rhesus monkey brain in a fashion to provide anatomical slices that related to the skull anatomy. “Stereotaxic instrument,” the section most quoted, describes the original stereotaxic apparatus, based on a Cartesian coordinate system that was the basis for the development of a human stereotactic apparatus 40 years later. “Electrolysis” presents the description of a controlled lesion made with direct current that has yet to be matched. “Excitation” was perhaps the first report of mechanical and electrical stimulation of a subcortical structure. The authors determined that faradic stimulation was superior to direct current stimulation, unipolar was more practical than bipolar, and that the cerebellar nuclei appeared to be more excitable than cerebellar cortex, both of which were not as excitable as certain areas of the cerebral cortex. All of this information was new and all was important in the subsequent development of surgery for movement disorders. With this experimental breakthrough, the first part of the twentieth century provided the laboratory information regarding the extrapyramidal system that later became the basis for movement disorder surgery. Even so, in the absence of understanding about the cerebral extrapyramidal system, attempts at treating movement disorders, especially PD, involved a variety of other structures. Foerster8 performed posterior rhizotomy for the treatment of spasticity and rigidity as early as 1908. Sympathetic ramisection and ganglionectomies were reported from the 1920s9,10 to as late as 1949.11 Posterolateral cordotomy was employed during the 1930s,12 and even thyroidectomy was used.13 In the 1930s attention returned to ablation of the cerebral cortex and the pyramidal system (Fig. 1.1). In 1932, Bucy and Buchanan14 presented their first report on a series of ablation of Brodmann areas 4 and 6, the primary motor cortex and adjacent tissue, for the treatment of athetosis. The resection area was extended somewhat for the treatment of parkinsonian tremor.15 Even much later, after it was clearly demonstrated that PD symptoms could be controlled by extrapyramidal lesions, Bucy16 (as well as Gillingham et al17) insisted that, regardless of the primary target, it was necessary to include some of the pyramidal system for the procedure to be successful. In 1937, Polenov18 interrupted the pyramidal fibers in the internal capsule, as did Browder19 in 1948. Fig. 1.1 Evolution of surgical operations for movement disorders. 1, Extirpation of premotor and motor areas of cortex (Horsley,4 Bucy16); 2, Section of pyramidal tract in the semioval center (pyramidotomy) (Polenov18); 3, Section of pyramidal tract in the internal capsule (Browder19); 4, Surgical or stereotactic pallidotomy (Meyers,32 Spiegel and Wycis,58 Cooper47); 5, Ventrolateral thalamotomy (Hassler and Riechert,39 Cooper et al49); 6, Subthalamotomy (Spiegel and Wycis66); 7, Clipping of anterior choroidal artery (Cooper61); 8, Section of pyramidal tract in peduncle (pedunculotomy) (Walker25); 9, Section of rubrospinal and tegmental tracts in medulla oblongata (bulbotomy) (Burdenko and Klosovski24); 10, Section of pyramidal tract in dorsal part of spinal cord lateral column (Putnam21); 11, Section of lateral column of the spinal cord (Oliver22). (From Kandel EI Functional and Stereotactic Neurosurgery. New York, London: Plenum; 1989.) Reprinted by permission. As late as 1951, Takebayashi20 reported the undercutting of the precentral cortex for the treatment of PD. The pyramidal tract was also attacked at the level of the cervical spinal cord, when Putnam21 modified his extrapyramidal cervical cordotomy to section the posterolateral quadrant, and Oliver22 cut the lateral column to include the pyramidal tract to treat tremor. It was during the 1930s and 1940s that the extrapyramidal pathways became the target of choice for treatment of movement disorders. One of the first efforts was high cervical anterolateral cordotomy for management of choreoathetosis reported by Putnam23 in 1933. In 1937, Burdenko24 sectioned the rubrospinal and tegmental tracts in the medulla. Approaching the extrapyramidal tracts at intracranial levels, even prior to the acceptance of stereotactic localization, was more challenging, and the two dominant figures reporting these procedures were Walker and Meyers. Walker25 incised the lateral two thirds of the contralateral pedicle to a depth of 6 to 7 mm for the management of first hemiballismus and later PD,26 and in Europe Guiot and Pecker27 made a similar but shallower incision, also for PD. Meyers, on the other hand, selected mainly intracerebral targets. As early as 1939, he performed a transventricular craniotomy approach to extirpate the contralateral head of the caudate nucleus in hemiparkinsonism in a patient who had failed cortical undercutting28 (Fig. 1.2). This was particularly adventurous given that Dandy29 had, less than a decade before, decreed—erroneously30—that the basal ganglia should not be disturbed, assuming that a lesion there would cause unconsciousness. This was based on observations of stroke that involved the anterior cerebral artery. The patient did well for 4 years with no significant deficit, which opened the door to even more adventurous procedures on the basal ganglia for movement disorders. When extirpation of the head of the caudate proved to be insufficient in many patients, Meyers31 added section of the anterior internal capsule, section of the ansa lenticularis (ansotomy), and even encroachment on the putamen. Slightly over 60% of patients had some benefit, but although the operative mortality decreased from 16%, it was never reduced below 10%, even in the latter part of the series. Meyers eventually considered the risk:benefit ratio to be insufficient to justify such procedures, and indicated that it “became apparent that open surgery at the level of the basal ganglia had a very limited applicability to the problem of paralysis agitans.”31 He did, however, confirm that lesions in the basal ganglia would not cause unconsciousness, that tremor could be abolished without paralysis, and that rigidity could be significantly reduced without paresis or postoperative spasticity, hyperreflexia, dyspraxia, abnormal postures or circumduction. Consequently, he prepared the way for the use of stereotactic surgery to target the basal ganglia and associated pathways for the treatment of movement disorders. The stage had been set for the introduction of human stereotactic surgery. A concept of potential subcortical targets had been developed from laboratory research, particularly on the extrapyramidal system. A basic concept of the pathophysiology of movement disorders had been obtained from extrapyramidal surgery, which demonstrated that such surgery was possible without disruption of voluntary movements or consciousness.28,32 Intraoperative x-ray was introduced, with rapid (at that time 30 minute) film processing and sufficient resolution to demonstrate such structures as pineal calcification or the foramen of Monro on ventriculography. Surgical experience on the limbic system had derived from prefrontal lobotomy.33,34 Indeed, the motivation for the development of human stereotactic surgery was Spiegel’s desire to obtain the benefits of prefrontal lobotomy without the risk of devastating neurological deficit.35 Human stereotactic surgery was introduced when Spiegel et al36 published a brief account in Science describing a technique to produce accurate lesions in specific sub-cortical targets within the human brain. The frame was a modification of the Horsley-Clarke apparatus that had been described 40 years earlier.7 The electrode holder was mounted on a system to move translationally in each of three planes corresponding to the three Cartesian coordinates. The major technical advance was that it used internal landmarks within the brain for targeting, rather than skull derived landmarks, which would have proven too inaccurate to use in humans.37 Consequently, they called this new field “stereoencephalotomy.” Despite the original plan to treat psychiatric disorders, the first recorded case involved alcohol injection into the pallidum and dorsomedian nucleus in a patient with Huntington chorea, producing significant clinical benefit.36 Fig. 1.2 Diagram of open surgical approaches to extrapyramidal structures. Frontal section at level of foramen of Monro, showing ansa lenticularis (Ans) and other pallidofugal elements interrupted in ansotomy for the relief of contralateral hemiparkinsonian tremor. M, approach employed by Meyers via corpus callosum (Cc), lateral and third ventricles; C, approach used by Cooper 47 and Fenelon114 to globus pallidus; G, approach employed by Guiot and Brion115 via perforated substance in neighborhood of optic tract (Op); Ca, body of caudate nucleus; T, thalamus; P, putamen; GI I, globus pallidus, crus I (medial segment); GI II, globus pallidus, crus II (lateral segment). (From Meyers R. Historical background and personal experiences in the surgical relief of hyperkinesia and hypertonus. In: Fields W, ed. Pathogenesis and Treatment of Parkinsonism. Springfield, IL: Chas C Thomas; 1958:229–270.) Reprinted by permission. Originally, Spiegel and Wycis38 used as their landmarks the calcified pineal gland and the foramen of Monro. It was not long, however, before Hassler and Riechert39 and Talairach et al40 advocated using the intercommissural line, which immediately became the standard. During the first 2 decades, numerous surgeons visited Spiegel and Wycis and came away with plans to develop their own stereotactic programs. There was no commercially available apparatus, so each surgeon designed his own (Fig. 1.3). A great deal of innovation was demonstrated. Leksell41 produced the first arc-centered device in 1948. Hécaen et al42 in Paris designed an apparatus that involved insertion of electrodes through a grid system. Riechert and Wolff43 in Germany introduced a phantom base to adjust their offset arc-centered electrode. Bailey and Stein44 used a pointing device mounted at the burr hole. Relatedly, Uchimura and Narabayashi,45 who did not have access to the Western literature in Japan, independently invented a translational type of stereotactic apparatus. Originally, the lesion was made with the injection of alcohol in hopes of sparing the fibers en passage. Spiegel et al36 soon modified their technique to utilize the same direct current that Horsley and Clarke7 had described in their 1908 paper. Other techniques were soon developed. Narabayashi and Okuma46 developed an oil—procaine or oil—procaine—wax mixture. Cooper47 employed alcohol injection but soon realized that it diffused uncontrollably; he then combined the alcohol with a thickening agent. When that proved also to be poorly controlled,48 he and colleagues tried to produce a cavity that would contain the alcohol by temporarily inflating a balloon,49 which still failed to control the extent of the lesion.48 Obrador developed a mechanical device, a leukotome, with a wire that could be extended to the side to make a lesion by rotating the central shaft.50 Hassler and Riechert39 utilized a radio frequency current to heat the tissue adjacent to the electrode tip, and similar devices eventually became the standard means of making a lesion.51 An interesting side story concerns Cooper and Lee’s52 plan to use a cryoprobe, a closed cannula through which liquid nitrogen flowed in a controlled fashion to freeze the surrounding tissue. Cooper had coincidentally hired an engineer by the name of Arnold St. J. Lee who had previously worked in Spiegel’s laboratory and was the fourth author on the original stereotactic paper.36 Cooper persisted in use of the cryoprobe even after radio frequency heating became the standard for safe and reliable lesioning. Fig. 1.3 The four basic types of stereotactic apparatus. (A–C) developed within the first decade of stereotactic surgery, and (D) with the advent of image guided surgery in 1979. (A) translational system (Spiegel-Wycis Model V116); (B) arc centered system (Leksell41); (C) burr-hole mounted apparatus; (D) system of interlocking arcs. The first few decades of stereotactic surgery provided a cornucopia of innovation and human experimentation. There were no experimental models for most motor disorders, so it was necessary to develop hypotheses from the logic of what was known about motor control and then try the new procedures in patients. Despite the risks, these patients had few options. All were severely disabled. There were few if any effective medications. The morbidity and mortality rates of open surgery were unacceptable. Movement disorders continued to be the major indication for stereotactic surgery, and eventually most movement disorder surgery involved stereotaxis. The mortality rate decreased from 15% in the prestereotactic era53 to 2% within a year54 and less than 1% by the second year.55 It must be recognized that the progression of PD that existed then was not the same as we see today. Prior to the introduction of L-dopa, patients became disabled more rapidly and presented for surgery much earlier in their disease. There was no medication-induced dyskinesia to be treated. Because tremor was the most obvious symptom and could be quantitated (albeit subjectively) better than bradykinesia or dystonia, most reports of that era discuss only relief of tremor. There were still many patients with postencephalitic parkinsonism in the patient pool, so the average age of the patients tended to be younger than it is now. Consequently, one must be cautious in comparing results from those days with present-day figures. Although there were a variety of targets for movement disorders, most involved interruption of the extrapyramidal circuit at the globus pallidus, the thalamus, or the pathways in between, and occasionally the subthalamic nucleus (STN) for PD. The literature at the advent of stereotactic surgery used the Walker56 nomenclature for the thalamic nuclei, and that continued to be most frequently used in the United States. The Europeans, however, adopted Hassler’s57 system when it became available, which identified smaller subnuclei on the basis of subtle differences in cytoarchitecture. The original target for all movement disorders was in the globus pallidus. In addition, the original intention was to interrupt as many of the emerging fibers as possible, to obtain the greatest extrapyramidal denervation as possible. Lesions involved the emerging fibers of the ansa lenticularis, and the procedure was named pallidoansotomy or pallidothalamotomy.58 Spiegel,35 however, was reluctant to interrupt this system in parkinsonian patients. In experimental animals, such lesions may cause hypokinesis, and he feared that the akinesia of PD would be made worse by surgery. It was only after Hassler and Riechert39 and Talairach et al59 treated parkinsonism by lesions in the ventrolateral thalamic nucleus in 1951 that stereotactic surgery was considered as a treatment of PD. Spiegel and Wycis60 began to treat PD, but they primarily targeted the pallidum, however, as did Narabayashi and Okuma46 and most others. In 1953, Cooper61 attempted a nonstereotactic craniotomy to perform Walker’s section of the cerebral peduncle in a patient with PD but encountered an interesting “surgical accident.” He inadvertently cut a vessel as he exposed the midbrain, and he stopped the procedure as soon as he had controlled the bleeding. The patient awoke with no neurological deficit, and the tremor and rigidity were abolished. In retrospect, Cooper determined that it had been the anterior choroidal artery that had been damaged, so he thereafter advocated purposefully ligating that vessel as a form of treatment. Although there was significant improvement reported in 16% of 55 patients thus treated, the operative mortality rate was 13.3%, and there was a significant morbidity rate as well. Cooper47 assumed that the benefit was from infarction of the globus pallidus and later advocated injecting that target with alcohol, although by that time the pallidum was already a favorite target of stereotacticians. When Cooper switched to injecting alcohol into the pallidum in ~1955, he did not use a stereotactic apparatus, but only a needle guide that directed the needle through the temporal lobe somewhat upward toward the globus pallidus.47 Around 1957, after a patient on whom he had an excellent result died of other causes, the autopsy revealed the lesion not to be in the pallidum but in the ventrolateral thalamus, which then became his target of choice.49 By that time, however, Hassler and Hess62 had already defined that thalamic target. In addition Cooper et al63 advocated pulvinotomy for treatment of spasticity, which was never documented by others. Athetosis, dyskinesia, and rigidity responded well to pallidotomy. Intention tremor and essential tremor were treated with lesions in the ventrolateral nucleus,64 according to the Walker nomenclature. This target included Hassler’s ventrointermedius (Vim) nucleus, the area eventually identified as the best target for tremor of any etiology.65 Although poststroke hemiballismus was produced by a small infarction in the STN, it might be treated by making larger STN66 or thalamic lesions.67 When Hassler began to divide the thalamic ventrolateral region into subnuclei in 1954,57 he and Riechert refined their ventrolateral target to conform to the new nomenclature; they advocated making the lesion for PD in the ventralis oralis posterior for tremor and another in the ventralis oralis anterior for rigidity.39 However, as time went on, the ideal target for tremor was defined more narrowly within the ventrolateral region, leading to the identification of the Vim subnucleus as the generally accepted target for tremor. Many surgeons followed Riechert and Hassler when they moved their lesion to the thalamus for all parkinsonian manifestations. Some surgeons, however, continued to advocate pallidotomy. Both studies of Spiegel and Wycis35 and Leksell and colleagues68 noted that a lesion placed somewhat more ventral and posterior than the usual pallidoansotomy target might produce increased improvement in rigidity and bradykinesia. In the late 1950s, Spiegel and Wycis and colleagues69,70 moved their lesion to H Forel field, to interrupt the most pallidofugal fibers with the smallest lesion, and they observed further improvement in rigidity and bradykinesia, as well as significant improvement in tremor.
The Prestereotactic Era (1890–1954)
The Early Stereotactic Era (1947–1968)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








