Imaging
In the early days, an invasive method had to be used even for the evaluation of ventricle size in idiopathic normal pressure hydrocephalus (iNPH). Now, we try to perform the complete diagnosis without having to resort to invasive methods. Although promising approaches have been found, completely noninvasive diagnostics for iNPH have not become a reality and the same difficulties remain in the follow-up of patients with iNPH, as well as during the treatment of complications.
The aim of this chapter is to describe the range of alternatives available so as to avoid invasive diagnostics when possible.
7.1 Computed Tomography
Native computed tomography (CT) remains the norm for diagnostic and follow-up examinations of iNPH. Even an old, one-slice CT scanner can provide all of the information needed about the configuration of the ventricular system. A CT scan requires only a few minutes and CT scanners are universally available.
The primary use of a CT scan in the diagnosis of iNPH is to detect an enlarged ventricular system, which is the key feature in iNPH. The secondary objective is to exclude the possibility that
Other features could produce the symptoms and not the suspected iNPH
Other features may have produced hydrocephalus (secondary hydrocephalus)
A contraindication for the surgical treatment of iNPH exists.
7.2 Subjective Assessment of Ventricular Size and Shape
A variety of assessment methods are widely available. Indeed, any experienced neurosurgeon could claim that he or she can identify a hydrocephalic constellation in a CT scan without the use of a measuring instrument. Although this approach is not objective, it does appear that the results of subjective assessment are not completely unreliable.1
In our experience, the typical CT scan of a patient with iNPH shows enlarged, cloddy ventricles. The frontal horns are more dilated than the occipital horns. The third ventricle is dilated, but it still retains an oval shape. Massive enlargements of the extracerebral arachnoid space and the sulci are not typical. Some of these criteria have been subjected to systematic examination, but they have failed to provide a reliable prediction for which patients would become responders or nonresponders.2,3
7.3 Indices
The radiologic assessment of patients with iNPH requires that different scans in the history of one patient are comparable when carried out by different examiners. Consequently, an index must be used to document ventricular size.
The indices used in the assessment of patients with iNPH have advantages, but they also have pitfalls. Consistency in the use of the same index by all examiners is essential.
7.3.1 Evans Index
The Evans index was introduced by Detroit (Michigan, United States) radiologist William A. Evans in 1942.4 At that time, the standard diagnostic method was encephalography. The present day definition of the index is an adaptation: in the cella media slice of a CT scan, the widest distance in the frontal horns is divided by the widest transverse distance between the tabulae internae. The index is widespread, easy to calculate, and does not require any special data acquisition. There is consensus that an Evans index > 0.3 is indicative of hydrocephalus. The Evans index directly indicates the width of the frontal horns, which, in our opinion, is the most specific change in the shape of the ventricles in patients with iNPH. The disadvantages of the index are that values vary significantly depending on the CT slice within the same CT scan and the lack of representation of ventricular volume.5 A pitfall of the Evans index is that CT scans with different gantry angles cannot be compared because the transverse distance between the tabulae internae changes according to the position of the slice. The same problem results from different standards in the angle of transverse CT and magnetic resonance imaging (MRI) scans.
7.3.2 Other Indices
Many indices have been published with regard to different forms of hydrocephalus. None of these alternative indices is widespread for the evaluation of patients with iNPH. All indices have advantages and disadvantages. Most important for communication within a clinic or a department is that all collaborators use the same index and are familiar with that index. For scientific publications, use of the Evans index is obligatory.
7.3.3 Third Ventricle Diameter
To differentiate between iNPH and some forms of functional aqueduct stenosis that are hardly detectable, it is important to pay attention to the width of the third ventricle and to the proportions of the third and fourth ventricles. Because these cases are rare, they must be examined individually. In our view, an index that includes the width of the third ventricle is not needed for patients with iNPH (Table 7.1).
Index | Image | Calculation | Advantages | Disadvantages/pitfalls |
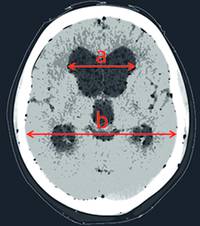
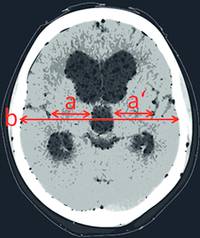
Evans index4 |
| Evans index = a/b |
|
|
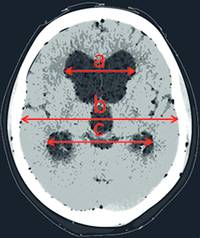
Fronto-occipital horn ratio syn. frontal and occipital horn ratio6,7,8 (FOR syn. FOHR) |
| FOHR = a + c/2b |
|
|
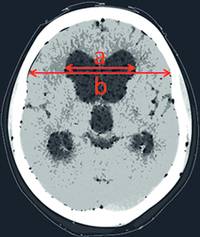
| FHR = a/b |
|
| |
| BCR = a/b |
|
| |
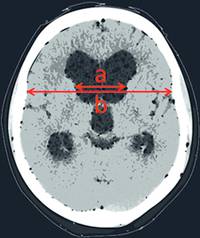
Third ventricular sylvian fissure ratio (3VSFR)9 |
| 3VSFR = (a+a′)/b |
|
|
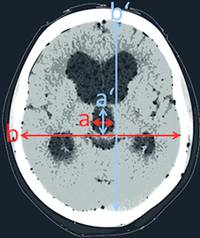
Third ventricular brain ratio (VBR3)9 |
| VBR3=A*A′/B*B′ |
|
|
Abbreviations: CT, computed tomography; iNPH, idiopathic normal pressure hydrocephalus; MRI, magnetic resonance imaging; syn., synonym. | ||||
7.4 MRI/Phase-Contrast MRI
MRI has advantages compared with CT in relation to the following possibilities:
The detection of special conditions (e.g., membranes) in the region of the aqueduct that could explain a functional stenosis
The measurement of aqueduct cerebrospinal fluid (CSF) flow
Generally, a CT scan is sufficient as preoperative imaging and has the advantage that postoperative CT scans are comparable in relation to ventricular width.
A preoperative MRI should be performed if the CT scan shows a mismatch between the size of the lateral ventricles and the third ventricle or between the third and fourth ventricles. In those cases, it may be of interest to detect structures causing functional stenosis and to open up the possibility of performing endoscopic procedures. As it is not a mistake to shunt a patient with obstructive hydrocephalus, MRI is not obligatory in patients showing enlarged lateral and third ventricles but a normal fourth ventricle. An MRI is, of course, essential if there is a suspicion of a “trapped” fourth ventricle that could worsen with postshunt surgery.
Aqueduct CSF flow seems to have a strong relationship with the pathophysiology of the iNPH; therefore, several attempts have been made to develop a reliable diagnostic tool based on this relationship. The rationale of increased aqueduct CSF flow is that, as a result of rigid basal arteries, cerebral blood flow is not transformed into a laminar streaming before entering the capillaries in patients with iNPH. Accordingly, the periventricular parenchyma pulsates with the frequency of the blood. Balancing this parenchyma pulsation, the CSF is forced out through the aqueduct with every heartbeat. This CSF movement can be measured by functional MRI (fMRI) either in milliliters per heartbeat or in milliliters per second.6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21 Through clinical studies performed by our own research group,22 we generated a threshold value of 24.5 mL/s to identify patients with iNPH, but we also found that this parameter is not appropriate for all patients. Currently, the measurement of aqueduct CSF flow is not a reliable method to establish an indication for shunt surgery (▶ Fig. 7.1).
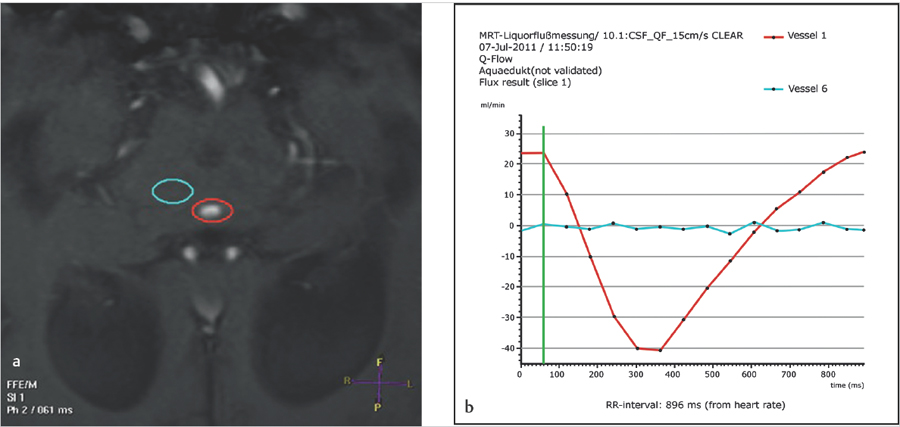
Fig. 7.1 (a and b) Measurement of the aqueductal cerebrospinal fluid flow by phase-contrast magnetic resonance imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree