Fig. 1
Example of swelling and infarct growth in a stroke patient. Baseline DWI (left panel) was compared with the co-registered follow-up DWI (middle panel) to assess the presence of swelling or infarct growth. Region of interest (ROI) defining the stroke at baseline and the stroke at follow-up were co-registered and merged to assign volumes for edema, infarct growth, and, as appropriate, hemorrhage (right panel) (From Battey et al. [13])
Brain Edema Portends Worse Outcome
First, using the categorical designations we found that patients with ICE had a greater likelihood of poor outcome (defined as modified Rankin Scale (mRS) 3-6; univariate p < 0.002; Fig. 2). In this cohort, infarct growth did not have an impact on outcome until a change in ASPECTS of >1 was used. Volumetric analysis of ICE showed that patients with poor outcome had higher ICE volume than those who did not (Fig. 3). Multivariate adjustment confirmed that swelling volume was an independent predictor of poor outcome (p = 0.02) [13]. Receiver operating characteristic (ROC) curve analysis showed that 11 mL of swelling volume had the highest sensitivity and specificity for distinguishing good versus poor outcome [13]. Together, these data suggest that ICE not only predicts worse outcome, but that an edema volume of >11 mL is sufficient to impair recovery.
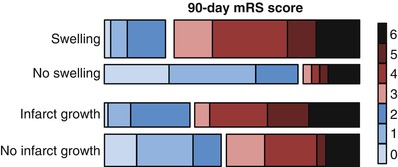
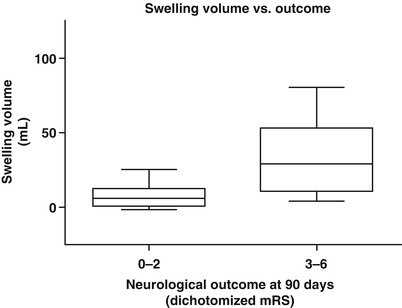
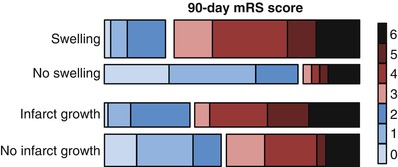
Fig. 2
The distribution of 90-day modified Rankin Scale (mRS) scores for subjects with and without swelling or infarct growth. The distribution for swelling and infarct growth are shown, with the right-hand color key representing each category of mRS as labeled. The height of each bar graph is representative of the percentage of the cohort with each characteristic (From Battey et al. [13])
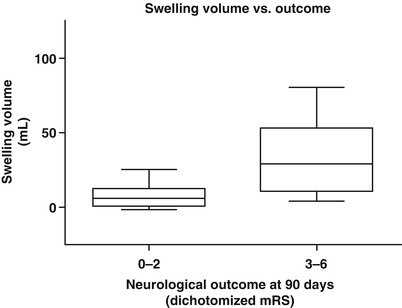
Fig. 3
Increased swelling volume is associated with poor neurological outcome at 90 days. The volume of swelling in subjects with mRS of 3–6 was significantly higher than those with mRS of 0–2 (p < 0.001) (From Battey et al. [13])
Predictors of Brain Edema
To understand the underlying mechanisms that contribute to ICE, our group has also studied the lesional properties of the stroke and assessed the association with subsequent ICE. Little is known about the biological factors underlying ICE that lead to poor outcome in stroke patients. Prior studies have demonstrated that high admission National Institutes of Health Stroke Scale (NIHSS) score and the initial stroke volume are key factors that determine the development of ICE [17, 18]. Indeed, our own studies confirm that stroke volume predicts ICE across a broader range of stroke volumes [13].
In addition, the severity of the initial cytotoxic injury can influence subsequent brain swelling [19–21], which is dependent on blood flow [22, 23]. Previously published data from our group provides further support that the severity of cytotoxic injury is predictive of ICE and is measurable using clinically available apparent diffusion coefficient (ADC) imaging [13]. Taken together, these data suggest that the degree of the cytotoxic injury plays a central role in determining the severity of ICE.
Significance for Clinical Trial Design
The development of imaging biomarkers of ICE has relevance for prognosis after stroke and also for clinical trial design and interpretation. As stroke size and cytotoxic injury (measured on apparent diffusion coefficient (ADC)) both predict ICE severity, these factors can be used to identify stroke patients at elevated risk for developing clinically significant edema. These patients may warrant closer observation for secondary neurological decline and also avoidance of factors that may worsen edema such as hypotonic solutions.
Our imaging biomarkers can also be used for selection of patients for inclusion in clinical trials targeting novel anti-edema therapies or as treatment response biomarkers. Accordingly, our ongoing evaluation of intravenous glyburide for the prevention of malignant edema see chap. 3 represents the ideal setting to test and validate these intermediate surrogate endpoints in the clinical development of anti-edema therapies.
Conclusions
Brain edema after stroke is a significant clinical problem with few current treatment options. The development and validation of neuroimaging biomarkers represents an important step in the further study of ICE. These surrogate endpoints can be used to assess prognosis and for treatment response in ongoing clinical trials.
References
1.
Go AS, Mozaffarian D, Roger VL et al (2014) Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 129(3):e28–e292CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








