Imaging of Lumbar Spondylolisthesis
Jean-Louis Dietemann
Adriana Bogorin
Robertson Correia Bernardo
Georg Zöllner
Radiological investigations using plain films, multidetector row helical computed tomography (CT) with multiplanar reformations, magnetic resonance imaging (MRI), and lumbar myelography may recognize the type of spondylolisthesis, evaluate the degree and progression of the slip, explain the clinical presentation, and help the physician to choose the appropriate treatment.
SPONDYLOLISTHESIS
Diagnosis of spondylolisthesis is obtained on lateral plain films of the lumbar spine performed in upright position, CT with sagittal reformations, or sagittal MR imaging of the lumbar spine. Lumbar spondylolisthesis may decrease, even disappear in supine position.
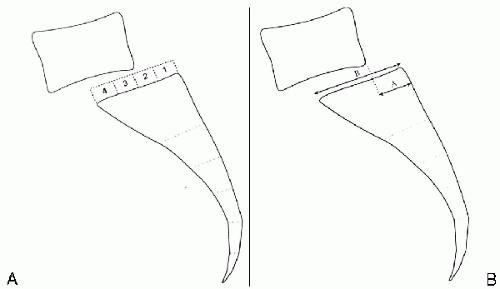
Measurement of the slip degree, using lateral plain radiographs obtained in upright position, is based on Meyerding’s classification, Taillard’s index, or Wiltse-Winter index. Meyerding’s classification describes five slip grades: grade 1 = 25%, grade 2 = 25% to 50%, grade 3 = 50% to 75%, grade 4 = 75% to 100%, and grade 5 = more than 100% corresponding to a complete dislocation, called spondyloptosis. Using Taillard’s index or Wiltse-Winter index, the degree of slip is expressed as a percentage (1,2,3) (Fig. 6.1).
CLASSIFICATION OF SPONDYLOLISTHESIS
Type 1: Dysplastic or Congenital Spondylolisthesis
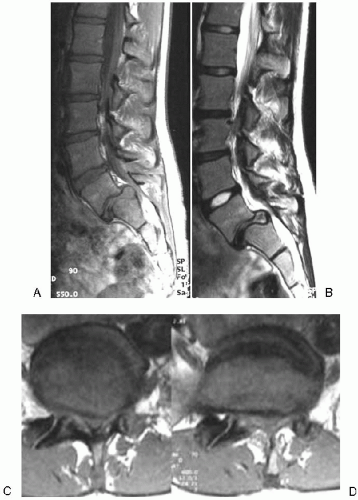
Dysplastic spondylolisthesis occurs at birth or early in life and is related to dysplasia of the upper sacrum (absence or dysplasia of the superior articular facets of S1 or elongated pars of L5). The slip is marked (grade 5 or spondyloptosis); the L5 vertebra may be displaced in front of S1 (Fig. 6.2). Hypoplasia and wedging of the L5 vertebral body is noted. Sacral rounding involving the upper aspect of S1 is usually observed. CT confirms absence or dysplasia of articular facets or bilateral elongated pars interarticularis; CT with sagittal reformations and MR imaging evaluate the degree of slip and foraminal and central canal stenosis (Fig. 6.3). There is usually an important central canal stenosis with compression of the dural sac and nerve roots between the neural arch of L5 and the posterior part of the S1 body (4).
Type 2: Isthmic Spondylolisthesis
Three subtypes are described: subtype A is related to a stress fracture of the pars interarticularis. In subtype B there is no defect but the pars interarticularis appears elongated; repeated healed microfractures are probably the cause of pars elongation. Subtype C corresponds to an acute fracture related to severe trauma.
Isthmic spondylolisthesis (subtype A) related to a stress or fatigue fracture (spondylolysis) involves the pars interarticularis of L5 in 90% of cases and usually occurs between the ages of 5 and 7. The spondylolisthesis appears between the ages of 10 and 15 and rarely increases after age 20 (2).
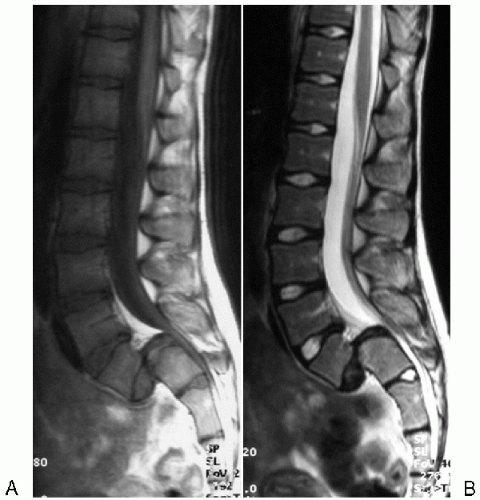 FIG. 6.2. Dysplastic L5-S1 spondylolisthesis. A: Sagittal MR imaging with T1 and (B) T2 weighted imaging. Grade 5 spondylolisthesis severe stenosis of the dural sac at the level of the listhesis. |
Plain films and CT demonstrate the defect involving the pars interarticularis. Spondylolysis associated with spondylolisthesis is best identified on coned lateral, anteroposterior with 30 degrees cranial angulation, and oblique plain radiographic projections (5) (Fig. 6.4). Visualization of the spondylolysis may be difficult on plain radiographs in the earliest stages before spondylolisthesis occurs. Multidetector helical CT with multiplanar reformations using thin section and reverse plane axial angulation allows precise analysis of the neural arch and appears superior to MR imaging for confirmation of the spondylolysis (5). However, improved visualization of the pars interarticularis is possible by using thin (3 mm) reverse-angle oblique axial T1W images (6,7). Axial CT may recognize recent and old stress fractures. However, CT may appear normal in the earliest stage of spondylolysis, before the fracture appears. At this stage, bone scan may reveal unilateral or bilateral increased activity involving the neural arch. MR imaging may demonstrate at the earliest stage of the stress fracture, low signal on T1 weighted imaging (WI), high signal on T2 WI, particularly on T2-STIR WI, and enhancement involving the pars interarticularis
but also the adjacent pedicles and the soft tissues surrounding the neural arch; these abnormalities are related to edema and increased vascularization (8,9) (Fig. 6.5).
but also the adjacent pedicles and the soft tissues surrounding the neural arch; these abnormalities are related to edema and increased vascularization (8,9) (Fig. 6.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree