Fig. 12.1
(a) Spinal hydatid cysts (arrows). (b) Spinal hydatid preoperative view (arrows). (c) Spinal hydatid resected specimen (arrows) (Courtesy of D. Chowdhury, MD)
Patients with hydatid disease usually present with symptoms caused by spinal cord or nerve root compression (Akhan et al. 1991; Pandey and Chaudhari 1997; Işlekel et al. 1998; Hilmani et al. 2004; Layadi et al. 2005; Adilay et al. 2007; Gopal et al. 2007; Kaen et al. 2009; Limaiem et al. 2010). Hydatid disease can be seen at any level of the spine (Bouras et al. 1984; Mathuriya et al. 1985; Göçer et al. 1994; von Sinner and Akhtar 1994; Pandey and Chaudhari 1997; Turgut 1997; Singh et al. 1998; Layadi et al. 2005; Adilay et al. 2007; Song et al. 2007; Arif and Zaheer 2009; Senoglu et al. 2009), but thoracic vertebrae are more commonly involved (Polat et al. 2003; Gopal et al. 2007), sometimes misleading to the diagnosis of Pott’s disease (Bouras et al. 1984; Turgut 1997; Song et al. 2007) and mimicking tuberculous spondylodiscitis (Tabak et al. 2007). Intradural hydatid at the foramen magnum was reported with all features of spinomedullary compression including respiratory distress, so hydatid disease should be considered in the differential diagnosis of compressive lesions at the foramen magnum (Mathuriya et al. 1985).
Hydatid cysts were classified according to their relationship with the dura mater, spinal canal, and spinal cord (Pamir et al. 1984; Fahl et al. 1994; von Sinner and Akhtar 1994; Berk et al. 1998; Turgut 2002; Polat et al. 2003; Adilay et al. 2007; Gopal et al. 2007; Arif and Zaheer 2009; Güneş et al. 2009) as intramedullary hydatid cysts, intradural extramedullary hydatid cysts, extradural-intraspinal hydatid cysts (Fig. 12.2), hydatid cysts of the vertebrae (Figs. 12.3, 12.4, 12.5, 12.6, and 12.7), and paravertebral hydatid cysts (Figs. 12.4, 12.8 and 12.9) (Polat et al. 2003). Intradural hydatid cysts are rare (Pamir et al. 1984; Kahilogullari et al. 2005; Arif and Zaheer 2009; Güneş et al. 2009).

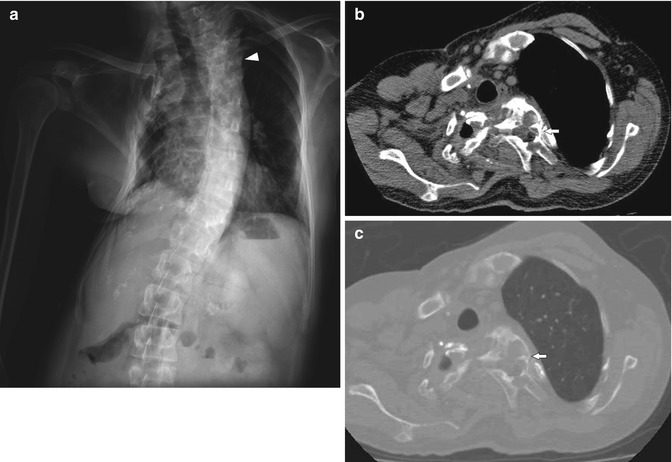

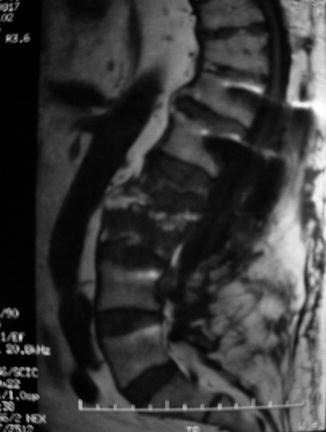
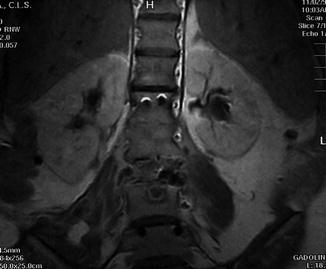
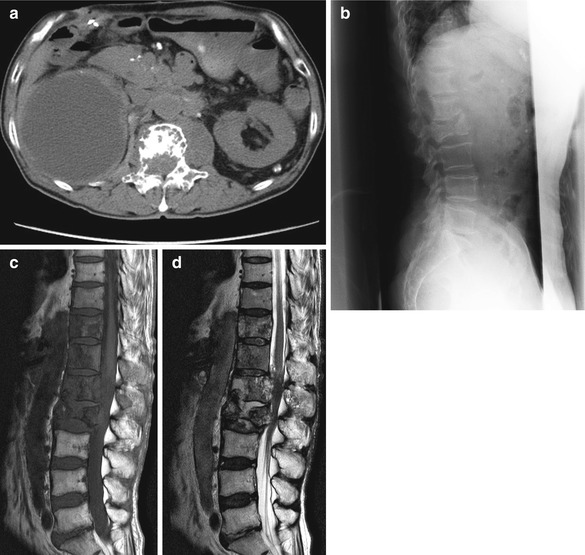

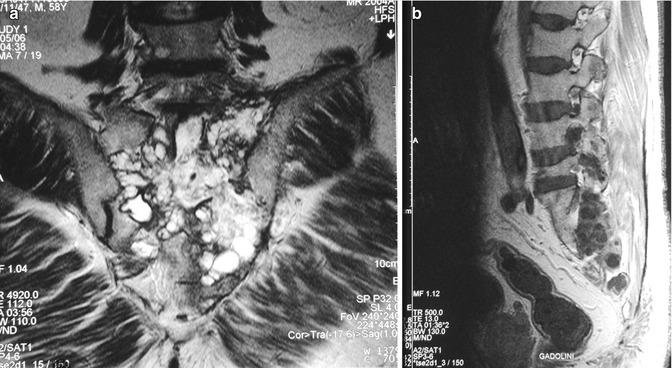

Fig. 12.2
(a, b) A 24-year-old male patient with extradural hydatid cyst at T4 vertebra corpus level (Courtesy of F. Limaiem, MD)
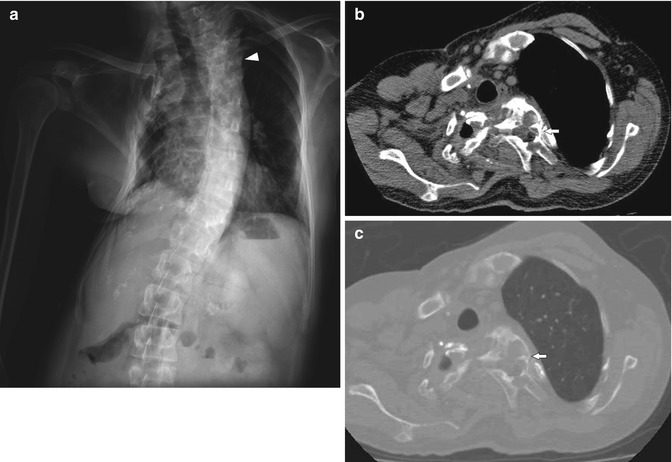
Fig. 12.3
Anteroposterior plain X-ray (a) of a 54-year-old male patient with thoracic spinal hydatid disease. There is marked kyphoscoliosis (arrowhead). Subtle radiolucent areas can be seen in the upper thoracic vertebrae. Unenhanced axial chest CT images with soft tissue window (b) and bone window (c) settings demonstrate hypodense cystic lesion in the vertebral corpus, which is isodense to cerebrospinal fluid, causing bone destruction and extending into the upper thoracic spinal canal (arrow). Chest deformities and subsequent tracheal deviation are prominent

Fig. 12.4
Anteroposterior plain X-ray (a) of a 43-year-old male patient with lumbar spinal hydatid disease. Decreased vertebral height and diffuse sclerosis is noticed at L4 vertebra (arrowheads). Sagittal reformatted CT image with bone window settings (b) demonstrates expansion and destruction at L4 vertebra with both sclerotic and lytic areas (arrows). Anterior paravertebral lesions with soft tissue density can also be seen. Sagittal spinal MRI demonstrates loss of height and destructive appearance with associating cystic lesions, hyperintense on T2-weighted image (c) and hypointense on T1-weighted image (d) (arrows), some of which extend into anterior paravertebral areas
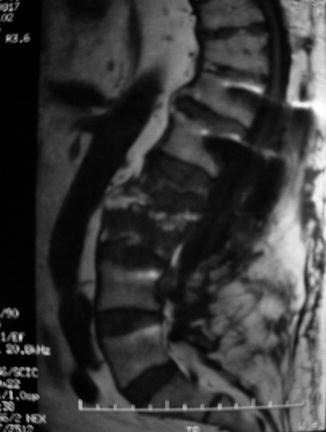
Fig. 12.5
A 59-year-old male patient who was operated 2 years ago had anterior debridement with partial corpectomy and grafting, posterior fusion. Despite the recurrence of disease, chemotherapy was not followed by the patient (Courtesy of A. Herrera, MD, PhD)
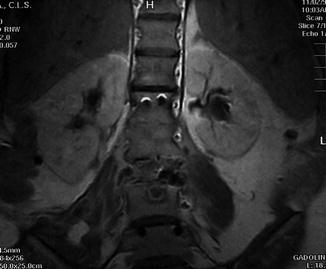
Fig. 12.6
A 46-year-old female patient. MRI lumbar spine hydatid lesions in L3 (Courtesy of A. Herrera, MD, PhD)
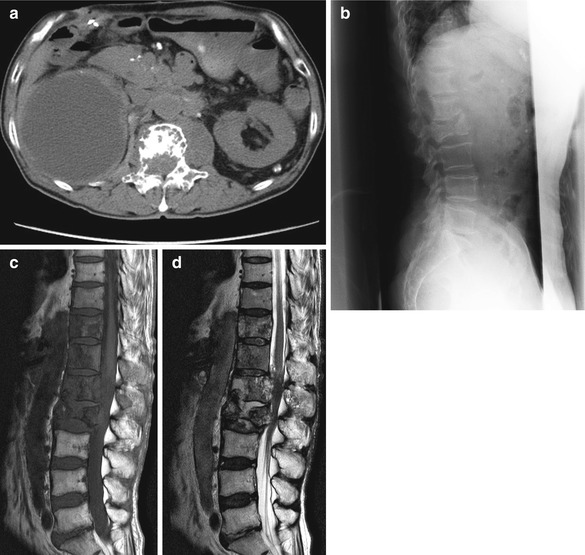
Fig. 12.7
(a–d) A 73-year-old male patient. He underwent palliative posterior decompression and instrumentation but died 2 years postoperatively (Courtesy of H. Sudo, MD)

Fig. 12.8
In a 46-year-old female with multiple sacral paraspinal hydatid cysts on the left side, unenhanced axial pelvic CT image (a) demonstrates a hypodense hydatid cyst (white arrow) in the left psoas muscle which shows a close relation with left sacral neural foramina and nerves. Posterior to the sacrum, another hydatid lesion (white arrowhead) is located in the erector spinae muscle. MRI reveals multicystic-multiloculated sacral paraspinal hydatid lesions (black arrows: lesion anterior to the sacrum, black arrowheads: lesions posterior to the sacrum) as sharply demarcated hyperintense lesions on sagittal T2-weighted (b) and axial T2-weighted (c) images, which are hypointense on sagittal T1-weighted image (d). One of the posteriorly located cysts protrudes into subcutaneous fat (black arrowhead). On sagittal (b) and axial T2-weighted images (c), collapsed germinative membranes inside the cyst in the left psoas muscle were clearly demonstrated (black arrows). All the cysts are isointense to cerebrospinal fluid
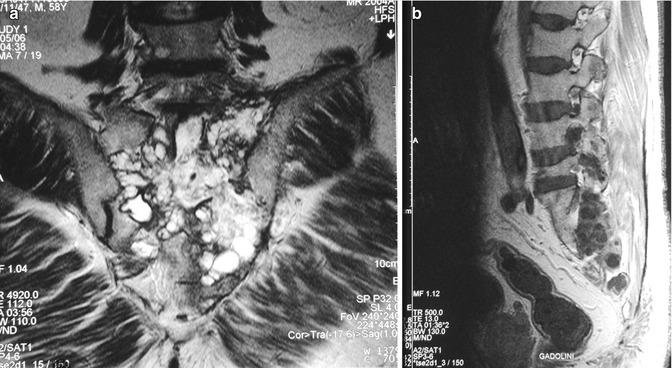
Fig. 12.9
(a, b) Sacral hydatidosis without accompanying neurological injury in a 61-year-old male patient. The patient with lung and liver hydatid cysts was not treated and transferred to his country of origin, Morocco (Courtesy of A. Herrera, MD, PhD)
Lack of osteoporosis and sclerosis in involved bone, absence of damage to intervertebral disk spaces and vertebral bodies, paraspinal extension, and (in the thoracic spine) involvement of contiguous rib are the most common features of spinal hydatid disease (Polat et al. 2003). Hydatid disease of the spine usually begins in the vertebral body. The cysts show slow growth in the direction of least resistance (Polat et al. 2003; Phatak 2006). With time, the parasite replaces the osseous tissue and destroys the cortex. It then spreads from bone to surrounding tissue such as muscle and the spinal cord (Polat et al. 2003). Extension into the spinal canal results in spinal cord and neural compression (Gopal et al. 2007). Hydatid cysts that lack the typical radiographic appearance may be mistaken for arachnoid cysts (Secer et al. 2008).
Plain X-rays are routinely obtained as a part of initial imaging but radiographic findings of spinal hydatid disease are nonspecific (Fig. 12.3). Plain X-rays may show bone destruction (Fig. 12.4) and sometimes abnormal soft tissue masses in the paravertebral region (Phatak 2006). However, they may show no bony abnormalities (Gopal et al. 2007; Arif and Zaheer 2009). It should be remembered that, radiographically, no sclerosis or periosteal reaction is evident in the early stages of the disease (Farzan et al. 2006).
Computed tomography (CT) and magnetic resonance imaging (MRI) demonstrate cystic cerebral hydatid disease effectively (Bükte et al. 2004) and they also serve for imaging of spinal hydatid disease (Figs. 12.1, 12.2, 12.3, 12.4, 12.5, 12.6, 12.7, and 12.9). After obtaining plain X-rays, CT and MRI should be used for further imaging as diagnostic tools of choice (Göçer et al. 1994; Turgut 1997; Gopal et al. 2007). CT and/or MRI techniques were found to be extremely useful, both for reaching the correct diagnosis and for proper surgical management of hydatid disease (Turgut 2002). CT and MRI have revolutionized neurosurgical practice for the diagnosis of hydatid cysts and allowed early diagnosis of the disease and provided localization of the lesions more accurately than we could do with plain X-ray, and also they could show multiple lesions (Turgut 1997); therefore, they are of value in preoperative planning of the surgical approach to hydatid lesions of the skeleton.
On CT and MRI, the appearance of the cystic fluid resembles that of cerebrospinal fluid (CSF) (Figs. 12.2, 12.3, 12.8, and 12.9) (Polat et al. 2003; Layadi et al. 2005; Gopal et al. 2007; Senoglu et al. 2009). In the past, myelography and CT myelography were used in the diagnosis of spinal hydatid disease (Işlekel et al. 1998), but now MRI has replaced the need for invasive myelography procedures.
Computed Tomography Scan
CT scan is effective in demonstrating the destructive hydatid lesions in vertebrae (Figs. 12.3, 12.4, 12.5, and 12.7), in determining their spread, and in establishing the presence of other hydatid cysts in adjacent soft tissues (Bouras et al. 1984; von Sinner and Akhtar 1994). CT could show multiple hydatid cysts in the ipsilateral psoas (Figs. 12.8) and quadratus lumborum muscles, widening of the neural foramen, and extension of cyst into the neural canal compressing the spinal cord (Phatak 2006).
In a 73-year-old man with sacral/retroperitoneal hydatid disease, CT could demonstrate a large, multiloculated, lytic lesion that expanded anteriorly causing extensive destruction of the sacrum and extending into the sacral canal. CT shows the cystic nature of the lesions which are isodense to CSF (Senoglu et al. 2009), but it is not possible to differentiate an extramedullary hydatid cyst from an arachnoid cyst by using only the CT views (Tuncel 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








