PSG parameters
n = 85
M:F
61:24
Age
47.8 ± 6.7
BMI
26.9 ± 2.7
AHI
33.3 ± 16.0
Supine AHI
44.3 ± 22.4
Lateral AHI
21.3 ± 22.4
O2 saturation min
80.2 ± 13.8
O2 saturation < 90 %
7.5 ± 13.1
Drug-Induced Sleep Endoscopy
Drug-induced sleep endoscopy (DISE) was performed in the following manner. The patient lied down comfortably in the supine position. Heart rate and oxygen saturation were monitored throughout the examination. Examination started in the awake state after unilateral nasal topical anesthesia and decongestion using cotton pledges placed at the middle meatus. Thereafter, sleep was induced by intravenous administration of midazolam (initial dose of 3 mg for adult patients over 50 kg; 0.06 mg/kg). After the patient fell asleep, endoscopy was performed through the same nostril. Desaturation events (drop of basal saturation during sleep of more than 3 %) were analyzed for obstruction level, structure, pattern, and degree and representative findings recorded. If there was no desaturation, changes during snoring were analyzed. Additional bolus of 0.5 mg of midazolam was administered in the event of awakenings. Target level of sedation was upper muscle relaxation producing obstruction (i.e., snoring or apnea) without respiratory depression. Level of sedation was maintained to a modified Ramsay score of 5 (sluggish response to a light glabellar tap or loud auditory stimulus) or 70–80 in selected patients in which BIS monitoring was used.
After observing the airway in the supine position, the patients were positioned in the right lateral decubitus position. Body and head was moved simultaneously so that axis of the body and the Frankfort plane of the head were perpendicular to the bed.
At least three obstructive events were observed in each position, and the most severe event was determined as the obstruction site of the patient. After the conclusion of the examination, 2 mg of flumazenil was administered intravenously as an antidote. The average examination time was 40 min.
Midazolam-induced sleep endoscopy (MISE) findings were classified according to obstruction structures (soft palate (SP), lateral wall (LW) including palatine tonsils, tongue base (TB), and larynx (LX) including epiglottis). The degree of obstruction was determined as 0, no obstruction; 1, partial obstruction (vibration with desaturation); and 2, complete obstruction (total collapse of airway with desaturation). For obstruction in the tongue base more than >50 % displacement compared to the awake state was determined as grade 1, while grade 2 obstruction was attributed for more than 75 % obstruction.
DISE Findings According to Sleep Position
In the supine position, the most common structure contributing to obstruction was the soft palate which was observed in 87.6 % of patients (n = 74) followed by TB (n = 65, 76.5 %), LW (n = 60, 70.6 %), and LX (n = 18, 21.2 %) (Table 2). When the patients were positioned in the lateral decubitus position, the most frequent anatomical structure contributing to obstruction changed from the SP to the LW which was seen in 51 patients (60 %), followed by SP (n = 19, 22.3 %), TB (n = 6, 7.1 %), and LX (n = 1, 1.4 %). A patent airway with no discernible site of obstruction was found in 25.3 % of patients in the lateral position. The degree of obstruction of the six patients who showed TB obstruction in the lateral position was all grade 1, indicating partial obstruction (Table 2). The prevalence of obstruction in the SP, TB, and LX showed statistically significant decrease when sleep position was changed from supine to lateral position (p < 0.05), while overall prevalence of LW obstruction was not affected by position change (p > 0.05).
Table 2
Changes of obstruction site according to sleep position (n = 85)
Obstruction site | Supine position, patient number (%) | Lateral position, patient number (%) |
|---|---|---|
Soft palate | ||
Total (n = 85) | 74 (87.6) | 19 (22.3)* |
Mod OSA (n = 47) | 43 (91.5) | 9 (19.1)* |
Severe OSA (n = 38) | 31 (81.6) | 10 (26.3)* |
Lateral wall | ||
Total | 60 (70.6) | 51 (60.0) |
Mod OSA | 29 (61.7) | 17 (36.2)* |
Severe OSA | 31 (81.6) | 34 (89.5) |
Tongue base | ||
Total | 65 (76.5) | 6 (7.1)* |
Mod OSA | 38 (80.1) | 4 (8.5)* |
Severe OSA | 27 (71.1) | 2 (5.0)* |
Larynx | ||
Total | 18 (21.2) | 1 (1.2)* |
Mod OSA | 11 (23.4) | 0 (0)* |
Severe OSA | 7 (18.4) | 1 (2.6)* |
No obstruction | ||
Total | 0 (0) | 21 (24.7)* |
Mod OSA | 0 (0) | 14 (29.8)* |
Severe OSA | 0 (0) | 2 (5.3)* |
Changes in Obstruction Site According to Severity of OSA
Among the 85 patients, 47 patients had moderate OSA (AHI = 15–29) and 38 patients had severe OSA (AHI ≥ 30). In moderate OSA patients, the prevalence of all the anatomic structures contributing to obstruction (SP, LW, TB, LX) showed significant improvement (p < 0.05) when position was changed from supine to lateral, with no airway obstruction in 29.8 % of patients (Table 2).
In severe OSA patients, the prevalence of obstruction in the SP, TB, and LX showed significant improvement (SP changed from 81.6 % to 26.3 %, TB from 71.1 % to 5.0 %, LX from 18.4 % to 2.6 %) after position is changed to the lateral position (p < 0.05). However, there was no change in the prevalence of obstruction in the LW. The incidence of LW obstruction in the lateral position was significantly higher in the severe OSA patients (89.5 %) compared to the moderate OSA patients (36.2 %) (p < 0.05).
Representative DISE findings in the supine and lateral positions are shown in Figs. 1 and 2.
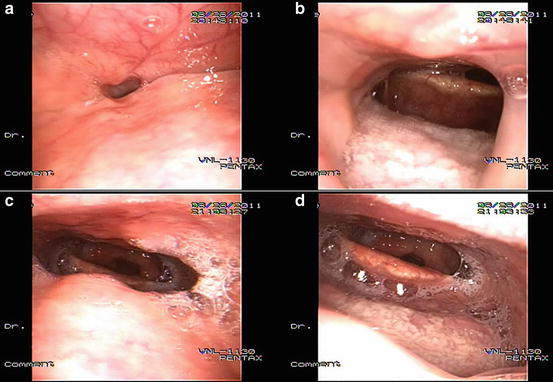
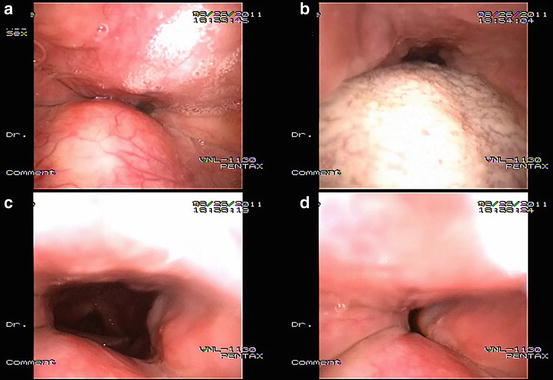
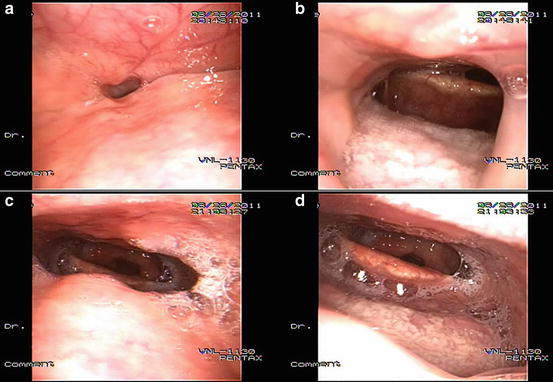
Fig. 1
Representative DISE findings from our series showing changes in site of obstruction according to sleep position. In the supine position (a, b), the patient shows obstruction at the soft palate (a) and tongue base resulting in secondary epiglottis obstruction (b). When the patient changed position to the lateral decubitus position (c, d) a patent airway was observed in the retropalatal and retroglossal airway. The AHI for this particular patient was 44.2 (total), 52.6 (supine), 7.4 (lateral). The patient was classified as lateral nonobstructor
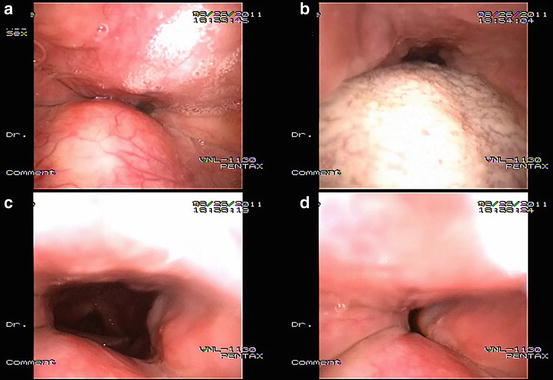
Fig. 2
Representative DISE findings from our series showing changes in site of obstruction according to sleep position. In the supine position (a, b), the patient shows obstruction at the soft palate (a), oropharyngeal lateral wall, and tongue base (b). When the patient changed position to the lateral decubitus position (c, d), there was no obstruction observed in the soft palate and tongue base (c); however, there was persistent obstruction in the lateral walls (b). The AHI for this particular patient was 63.8 (total), 89.7 (supine), and 32.2 (lateral). The patient was classified as lateral obstructor
Changes in Obstruction Site in Lateral Obstructors and Lateral Nonobstructors
Subgroup analysis was carried out in 78 patients whose sleep time spent in lateral position was greater than 30 min. Among them, 50 patients were position dependent (PD), while 28 were non-position dependent (NPD). Patients with a lateral AHI equal or below 10 were regarded as lateral nonobstructors (LNO), while those who had a lateral AHI equal or above 10 were regarded as lateral obstructors (LO). Characteristics of the two groups are summarized in Table 3.
Table 3
Demographic and polysomnographic findings of LO and LNO
LO (n = 42) | LNO (n = 36) | |
|---|---|---|
M:F | 34:8 | 25:11 |
Age | 46.7 ± 8.3 | 48.8 ± 5.7 |
BMI | 28.8 ± 3.2
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



