Fig. 13.1
Incidental finding on MRI (a FLAIR sequence) of numerous focal white matter hyperintensities in a 54-year-old female patient with no particular history investigated for nonspecific chronic headache. The patient was otherwise asymptomatic. Note the absence of any abnormality suggestive of recent ischaemic or haemorrhagic lesion on the other sequences (b diffusion-weighted images, c T2*-weighted images)
Ubiquitous topography but preferentially located at the cortical-subcortical junction. Lesions become stable with time. No associated spinal cord abnormalities on MRI.
Management
No specific monitoring in the absence of symptoms.
Unruptured Aneurysm (Fig. 13.2)
Prevalence of 2–5 % in the general population.
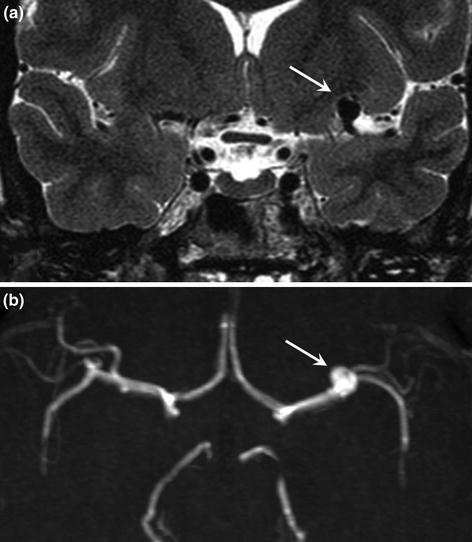
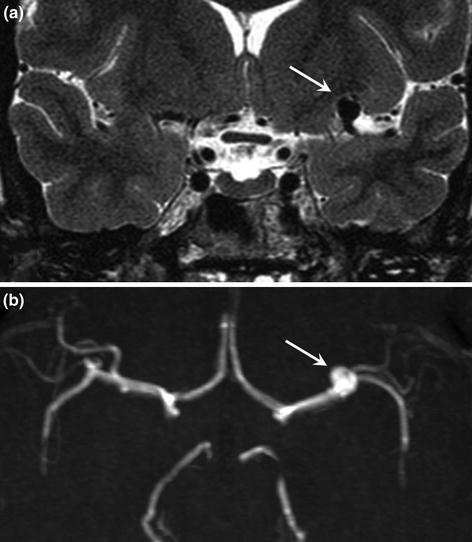
Fig. 13.2
Incidental finding of unruptured intracranial aneurysm on brain MRI in a young female patient. The aneurysm is hypointense on the T2-weighted SE image (a arrow, coronal section). The TOF sequence (b arrow, axial reconstruction) confirms the presence of the saccular aneurysm at the left middle cerebral artery bifurcation
An intracranial aneurysm is a frequent incidental finding on imaging (MRI, CT angiography) and is the second most common incidental finding after silent infarcts on brain MRI procedure, detected on 0.23–1.8 % of MRI examinations.
Size at the time of discovery often <7 mm and often in the carotid territory.
Imaging
CT
Spontaneously isodense. Sometimes fine mural calcifications. Intensive contrast enhancement.
MRI
Additional image on TOF sequence, clearly visible as hypointensity on T2-weighted SE images.
Pulse artifact around the aneurysm. Early intensive gadolinium enhancement.
A large aneurysm can cause a mass effect on adjacent structures with hyperintense perianeurysmal oedema on T2-weighted and FLAIR images.
Management
No randomized study has been conducted.
Consultation with an interventional neuroradiologist or neurosurgeon to determine the management strategy: simple surveillance or endovascular or surgical treatment according to criteria associated with an increased risk of spontaneous rupture of the aneurysm.
The two main factors associated with an increased risk of rupture are the size of the aneurysm >7 mm and smoking. Other factors are also known to increase the risk of rupture: alcoholism, hypertension, family history of ruptured intracranial aneurysm and vertebrobasilar or posterior communicating artery aneurysms.
Developmental Venous Anomaly (Fig. 13.3)
Developmental venous anomalies are also called venous angiomas.


Fig. 13.3
Gadolinium-enhanced MRI T1-weighted sequence showing a superficial developmental venous anomaly draining the deep part of the brain (hollow arrow). The transcortical vein drains into an enlarged normal cortical vein related to a larger draining territory compared with other cortical veins
The superficial cerebral venous drainage is ensured by superficial cortical veins. The deep venous drainage is ensured by deep cerebral veins. The superficial and deep venous networks communicate via transcortical veins that are not visible or only barely visible on imaging.
Developmental venous anomaly: superficial venous drainage of a deep territory or deep venous drainage of a superficial territory via a dilated transcortical vein located in a cerebral hemisphere or the cerebellum, but never in the brainstem or spinal cord.
Frequently associated with cerebral cavernous malformation, or more rarely with arteriovenous malformation, sinus pericranii, anomaly of cortical gyri (pachygyria, schizo-encephalopathy), venous or sinus ectasia, capillary telangiectasia.
Clinical Features
Asymptomatic when the anomaly is isolated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








