Fig. 4.1
(a, b) PSO grade 3: closing wedge within body. (c) PSO grade 4 closing/opening body and disc
Spinal osteotomy can be undertaken in pediatric and adult patients who present with spinal deformity in one or more planes and require release/destabilizing operations (osteotomies/resection) to achieve the desired correction. Most common indications include spinal decompensation or malalignment, progressive deformity, pseudarthrosis in a previously fused spine, and postoperative crankshaft in pediatric patients.
Spinal decompensation or malalignment occurs when there is a global or regional imbalance with resultant clinical deformity. It can be a single plane or in multiple planes. Single plane deformities can be in the coronal or sagittal plane. Rigid, severe scoliosis and postoperative coronal malalignment with or with adjacent segment degeneration are examples of coronal deformity. In the sagittal plane, Scheuermann’s kyphosis, ankylosing spondylitis, and proximal junctional kyphosis in a previously fused spine are common examples of sagittal plane deformities. Multiplanar deformities usually result from either complex kyphoscoliosis or previously fused spine with progressive deformity as a result of pseudarthrosis, adjacent segment degeneration, or of crankshaft phenomenon in a pediatric patient (Fig. 4.2).


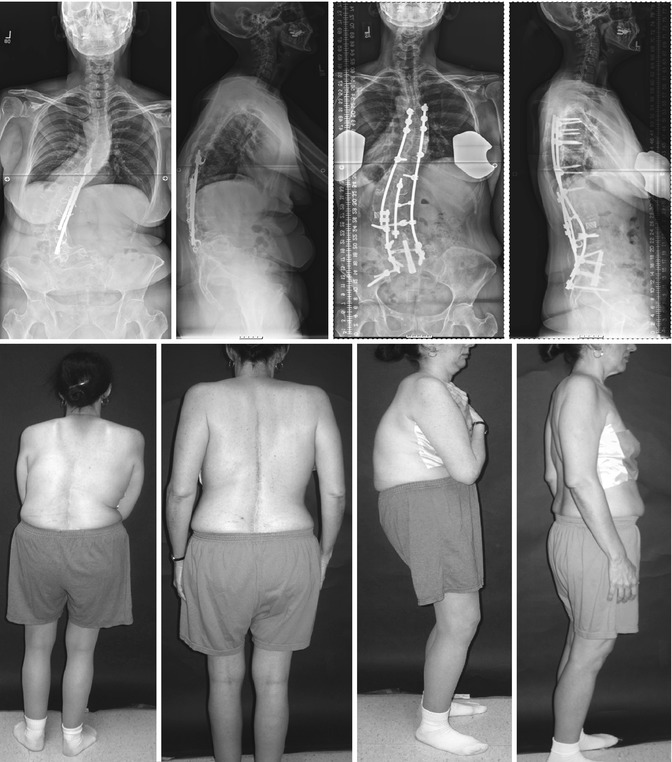
Fig. 4.2
Pre and post op AP and lateral radiographs of 20 year old female with congenital kyphoscoliosis treated with multiple level posterior Smith-Petersen osteotomies. PSF C6-L4, SPO T4-L1 thoracoplasty and concave rib osteotomies
4.2 Smith-Petersen Osteotomies
This type of osteotomy was originally described in 1945 for the treatment of ankylosing spondylitis. Smith-Petersen osteotomies are most commonly performed in the lumbar spine to produce correction of about 10–15° [13] per level with approximately 1° correction per 1-mm bone resected [14] in the sagittal plane. This technique can also be applied in coronal plane deformities such as severe scoliosis with primary ankylosis of the motion segments or in a previously fused thoracic or lumbar spine. Performing multiple Smith-Petersen osteotomies to achieve the desired correction requires a mobile anterior column as in a primary deformity in a pediatric or adult patient. In a pure sagittal plane deformity with anterior ankylosis as in ankylosing spondylitis, an extension of the anterior column with bony osteoclasis results. Such lengthening of the anterior column may also lead to vascular injuries [9, 15].
Other complications may include dural tear, cauda equina compression and postoperative ileus, pseudarthrosis, and inadequate correction. The void created by the extension of the anterior column may require a supplemental anterior augmentation with structural bone or metal cages and grafts [15, 16].
Bridwell KH. et al. [6, 11, 12] applied osteotomies for fixed deformities in the thoracic and lumbar spine and showed that 1° of sagittal correction can be achieved for each millimeter of bone resected using the Smith-Petersen osteotomy technique without bridging anterior osteophytes and usually allowed a 10–15 mm osteotomy. Other authors have stressed the importance of undercutting the osteotomies to avoid encroachment on neural structures during closure of the osteotomy site [5, 17]. Simmons focused on the Smith-Petersen osteotomy for ankylosing spondylitis and reported a mortality of 8–10 % and neurological deficit including paralysis of 30 % [15].
We reported a series of 27 adults who underwent either multiple anterior discectomies or anterior osteotomies combined with Smith-Petersen osteotomy and achieved a postoperative sagittal balance of approximately 6.5 cm [18].
A similar osteotomy has been described by Alberto Ponte to correct sagittal deformities by removal of the entire facet and closure of same in unfused spine such as in Scheuermann’s kyphosis or in a kyphoscoliosis patients. This osteotomy is not to be confused with the Smith-Petersen osteotomy where there is ankylosis or fusion of the facets that require their removal [19].
4.3 Pedicle Subtraction Osteotomy
PSO is a posterior based three-column osteotomy performed for a fixed sagittal or coronal plane deformity and is a posterior shortening operation deemed to be safer than the anterior column lengthening procedure in SPO. Main indications for PSO include patients for whom posterior osteotomies alone (i.e., Smith-Petersen osteotomies) are likely to provide inadequate correction, and cases in which at least 30° of corrective lordosis are required [6, 11, 12, 20, 21] (Fig. 4.3).


Fig. 4.3
Pre op and postoperative radiographs and clinical photographs of 36-year-old male ankylosing spondylitis and sagittal malalignment; surgical treatment consisted of PSO at L3 and multilevel segmental spinal instrumentation. Anterior column support with mesh cage was performed
The ideal candidates for PSO are patients with substantial sagittal malalignment (approximately 10–12 cm), sharp angular kyphosis and patients who have undergone a prior multilevel circumferential fusion that would preclude performing SPOs. Although the osteotomy may be performed in the thoracic spine, most often it is performed in the lumbar spine, typically at the L2 or L3 level. The size of the osteotomy is based on preoperative standing radiograph measurements. The goal of surgery is restoration of normal sagittal balance with the C7 plumb line falling at or within 4 cm of the posterior-superior corner of S1.
In patients with biplanar deformity, a unilateral or biplanar PSO can be performed with asymmetric removal of the pedicles and the three columns to achieve the desired correction. Typically, at least six fixation points (preferably pedicle screws) should be used both proximal and distal to the level of the osteotomy [22]. Continuous monitoring by somatosensory-evoked potentials (SSEPs) and neurogenic motor-evoked potentials (NMEPs) or transcranial motor-evoked potentials (tcMEP) is critical to avert a neural element injury [23].
4.4 Vertebral Column Resection (VCR)
Vertebral column resection is the most complicated of the three-column osteotomies that carry a substantial neurologic risk to the patients [10, 14]. Unlike in the lumbar spine where a PSO can provide 30–40° of lordosis, in the thoracic spine, a PSO does not provide the same degree of correction and, therefore, for sharp angular thoracic and thoracolumbar kyphosis, a posterior-based vertebral column resection (VCR) is preferred. A VCR is particularly useful when the kyphosis is associated with significant coronal malalignment [14, 24]. The approach can be very helpful when dealing with a hemivertebra or when the anterior column has to be reconstructed in the setting of tumor, infection, and trauma. Although most frequently the procedure is performed in the thoracic spine, it can be performed in the lumbar spine as well. Both pediatric and adult patients with complex spine deformities can benefit from the VCR operation, either as a posterior only approach or as combined anterior/posterior procedures [2, 5, 23] (Fig. 4.4).