Fig. 18.1
Drawing of cross-section at C5 level. Deep cervical fascia is marked in green, pretrachreal fascia with carotid sheath in orange (neurovascular bundle is contained in it) and prevertebral fascia in violet
Fig. 18.2
Drawing of the antero-lateral cervical anatomy . Inferior constrictor and esophagus are retracted medially. The cranial carotid sheath and surrounding pretracheal fascia are removed. The prevertebral fascia overrides the scalenus muscles and the longus colli. The nervus vagus is sectioned. The dashed and dotted line shows the vagus nerve which runs in the thoracic cavity and gives the recurrent laryngeal nerve
The superior laryngeal nerve divides itself near the Ganglion inferius of the vagus nerve, at the level of the hyoid bone, in an internal and external branch. The external branch innervates the thyreopharyngeal and cricopharyngeal part of the inferior pharyngeal constrictor muscles and the cricothyroideal muscle. Some of its fibers breaks through the Membrana cricothyroidea and innervate the mucosa of the anterior commissure of the larynx. The internal branch runs with the superior laryngeal artery through the Membrana thyroidea and runs under the mucosa of the Recessus piriformis (Plica nervi laryngei). It innervates the mucosa of the inlet of the larynx, the atrium of the larynx and the posterior part of the Plica vocalis. In the Recessus piriformis the internal branch of the superior laryngeal nerve forms an anastomose with the inferior laryngeal nerve (Galen-Anastomose).
Inferior laryngeal nerves are end-branches of the N. laryngei recurrenti. They are asymmetric, with the left one which descends the carotid sheath into the thorax.
The inferior laryngeal nerve is located in a trough between Trachea and Esophagus cranially and reaches the larynx between the inferior horn of the thyroid cartilage and the posterior cricoarythenoid muscle. Here the nerve gives a posterior and an anterior branch. The posterior branch innervates the posterior cricothyroideal muscles as the transversal and the oblique arytenoideal muscles. The anterior branch innervates the thyreoarytenoideal and lateral cricoarytenoideal muscles. The inferior laryngeal nerve is responsible of sensitivity of the infraglotteal cavity of the upper trachea, esophagus and hypopharynx.
It curves around the aortic arch and return up between esophagus and trachea. The right one turns around the subclavian artery.
Lesions of the nervus laryngeus superior leads to a paralysis of the cricothyroid muscles and hypoestesy of major part of the internal laryngeal space. The tension of the vocal folds is decreased and the protection reflex (cough reflex, and close of the glottis) are impaired.
Lesions of the inferior laryngeal nerve (n. laryngeus recurrens) are called recurrent paralysis . Symptoms of the paralysis of the muscles innervated from the nerve are individually different. In general the main symptom is “whispering”. In case of monolateral lesion, is the vocal fold in a paramedian position. In case of bilateral lesion the patient will become dyspnoic [10].
Classification
Main purposes of a classification system of traumatic cervical spine lesions are giving a scale related to the gravity of the injury which is easy to communicate, offering treatment options and providing outcome. Unfortunately any classification meets all the expectation and doesn’t exist till now a widely accepted system [11].
In our opinion three main criteria have to be considered:
Biomechanics of the accident (compression, distraction, translation/rotation)
Neurological status (radicular, medullary, mieloradicular)
Stability of the lesion (White and Panjabi, columns theory, MRI)
Biomechanics
Compression Lesions
They represent the most common injuries. The mechanism is flexion and axial loading or a combination of both. Pure compression fractures involve only the anterior column. The involved part can be the vertebral body or the endplate. Occasionally fractures of the posterior elements are possible such as displaced or undisplaced facet fractures and/or lateral mass fracture. These lesions can be associated to osteopenia and osteoporosis, pathologic fracture and loss of normal cervical lordosis.
Particular morphologies of such fractures are represented from:
Burst fractures: the predominant component is the axial compression and only in a less measure flexion. In this fracture the anterior and middle columns are involved and fragments are often present in the canal. Concomitant spinal cord injuries are quite frequent [4, 12].
Teardrop fractures: the anterior inferior vertebral body is interrupted with the presence of a free fragment. The predominant mechanism is hyperflexion. The concomitant presence and the degree of an axial loading can contribute to transform this lesion in a burst fracture. Neurological lesions are possible [4, 12].
Distraction Lesions
The main aspect of these lesions is the disruption of the anatomical vertical axis. During an extension the anterior longitudinal ligament, the vertebral bodies and the intervertebral discs counteract the forces while during the flexion the solely bony and capsuloligamentous constraints of the facet articulation counteract the forces. The fact that these strong constraints are knocked informs us of the great degree of injury as well the higher instability represented from these injuries than a mere compression injury [12]. Common dynamic of the injury are falls or vehicular injuries [4]. Ligamentous disruption is quite common in this kind of injury. They can affect the facet joints (subluxation or luxation) and the disc space (widening; “fish mouth” anterior deformity). If concomitant axial load is present, posterior elements can be broken or spinal cord injury can occur [12]. The standard radiology after the accident can show only paravertebral soft tissue abnormalities because at the injury force arrest the column can be spontaneously returned to an “anatomical” rest situation [4]. MRI can be decisive to evaluate the injury pattern of distraction [12]. Among the posterior elements, the facet complex seems to be the most important for the stability [13]. At the MRI, signal of abnormality of the spinal cord after distraction lesion are quite common [4].
Translation/Rotation Lesions
The main characteristic is the horizontal displacement of a vertebral body on plain AP X-Rays . The usual degree of translation and rotation defined as pathologic are respectively 3.5 mm and ≥11° [14]. These pattern of injury are characterized from: bilateral pedicle fractures, bilateral facet fractures/dislocations, fracture separation of the lateral mass (“floating fractures”) [15]. Anterior and posterior complex can be both injured. An MRI study is usually indicated [12].
Two specific cases deserve a more accurate description because are combinations of the previous three mechanism of injury:
Unilateral facet dislocation
The dynamic is a combined flexion and rotation. The facet on the opposite side of the rotation is displaced anteriorly with locking in front of the facet below. Two adjacent segments show a different projection, with one that is projected laterally and the other on an oblique plane. On the anteroposterior view a brisk misalignment of the spinous processes can be observed. CT or MRI can give more informations (Fig. 18.3). Spinal cord injuries can be associated. In these injuries a radicular symptoms can present in the clinical pattern [4].
Fig. 18.3
Radiologic assessment of an unilateral facet joint fracture/luxation with anterior and rotatory shift on the preoperative CT (a, b) and MRI (c). On the right (d) the postoperative lateral X-Ray control after anterior microdiscectomy, open reduction using axial traction and plating
Bilateral facet dislocation
The dynamic is an abrupt hyperflexion and anterior translation with posterior longitudinal ligament insufficiency, which permit a forward dislocation of the facets. In this case a spinal cord injury is more frequent than in the unilateral. Usually the dislocation of the vertebral body is higher than 25 %. They are always highly instable lesions and traction weight must be monitored with radiographically for the risk of over distraction [4].
Neurological Status
Radicular, medullary or mielo-radicular syndromes can be objectivated.
There are different types of incomplete injury syndromes.
Anterior cord syndrome : usually due to traumatic anterior flexion of the cervical spine with direct injury of the spinal cord or indirectly with impairment of the blood supply from the anterior spinal artery. There is motor function impairment and a temperature and pain sensation deficit below the lesion, while proprioception and touch as well vibration sensation are intact.
Posterior cord syndrome : is a very rare condition and is caused from the direct trauma or loss of blood supply from the posterior spinal artery in a hyperextension of the spine. It results in loss of proprioception and epicritic sensation below the injured level.
Hemicord syndrome (Brown–Séquard syndrome) : is a hemisection of the spinal cord. Precise hemisection are rare and the most of these kind of lesions are caused by penetrating wound (knife or gunshots). The ipsliateral side of the injury presents a loss of motor function, light touch, vibration and proprioception. The controlateral side has a loss of pain, temperature and gross touch below the lesion level. Usually the controlateral deficit starts few dermatomes below the section (spinotalamic tract doesn’t cross immediately but ascend between two and four levels before to decussate).
Central cord syndrome : represents a form of spinal cord injury with impairment of the arms and hands function and only to a lesser extent in the legs. Some clinicians refer to that like a reversed plegia. Cervical and thoracic segments can be affected. The condition is caused mainly by hemorrhage, ischemia or necrosis. Trauma can cause prolonged ischemia of the spinal cord tissue. The corticospinal fibers committed to the leg are spared because of the external anatomical location. The condition can also emerge in a second time after spinal shock because of prolonged swelling around the vertebrae. The syndrome may be permanent or transient (Fig. 18.4).
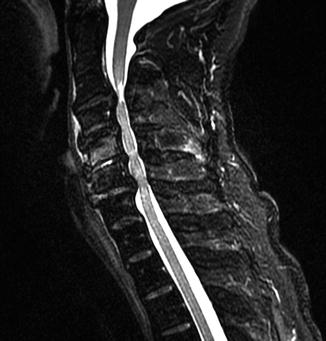
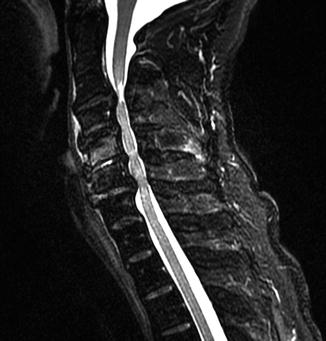
Fig. 18.4
Sagittal T2 MRI image of a cervical injury associated to spinal cord lesion with preexistent spinal canal stenosis
Neurological Impairment Scales
The first popular clinical scale to segregate the posttraumatic neurological status was introduced internationally by Frankel in the seventies.
It was organized in five categories were i.e. no function (A), sensory only (B), some sensory and motor preservation (C), useful motor function (D), and normal (E) [16].
Acute spinal cord injury – Frankel Classification grading system
Grade A | Complete neurological injury – no motor or sensory function clinically detected below the level of the injury. |
Grade B | Preserved sensation only – no motor function clinically detected below the level of the injury; sensory function remains below the level of the injury but may include only partial function (sacral sparing qualifies as preserved sensation). |
Grade C | Preserved motor non-functional – some motor function observed below the level of the injury, but is of no practical use to the patient. |
Grade D | Preserved motor function – useful motor function below the level of the injury; patient can move lower limbs and walk with or without aid, but does not have a normal gait or strength in all motor groups. |
Grade E | Normal motor – no clinically detected abnormality in motor or sensory function with normal sphincter function; abnormal reflexes and subjective sensory abnormalities may be present. |
The successor of the Frankel scale was the American Spinal Injury Association impairment scale introduced the first time in the 1982 [17]. The ASIA impairment scale categorizes motor and sensory impairment in individuals with SCI.
ASIA impairment scale
A = Complete | No sensory or motor function is preserved in the sacral segments S4-5 |
B = Sensory Incomplete. | Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-5 (light touch or pin prick at S4-5 or deep anal pressure) AND no motor function is preserved more than three levels below the motor level on either side of the body. |
C = Motor Incomplete | Motor function is preserved below the neurological levela, and more than half of key muscle functions below the neurological level of injury (NLI) have a muscle grade less than 3 (Grades 0–2). |
D = Motor Incomplete. | Motor function is preserved below the neurological levela, and at least half (half or more) of key muscle functions below the NLI have a muscle grade > 3. |
E = Normal | If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments, and the patient had prior deficits, then the AIS grade is E. Someone without an initial SCI does not receive an AIS grade. |
Stability
Columns Theory
Holdsworth introduced the new concept of two columns [18]. The anterior column is composed of the anterior longitudinal ligament, vertebral body, intervertebral disk and posterior longitudinal ligament. The posterior column is made up of all the ligamentous and bony structures behind the posterior longitudinal ligament. This concept has been decisively to understand injury pattern mainly in flexion and extension mechanism. The improvement offered from the Denis’ concept of three columns represented a breakthrough to define the condition of vertebral column stability [19]. The concept was initially applied to the thoracolumbar column but can be helpfully extended to the cervical spine for the understanding of its biomechanics.
To the middle column take part the posterior third of the vertebral body, the annulus fibrosus and the posterior longitudinal ligament. The posterior column consists of posterior neural arch, spinous process, articular processes and their capsules .
Radiographic Instability Criteria
Normal kinematics is facilitated from two fundamental structures: discoligamentous complex and the articulating facet joints.
Most of the criteria of spinal instability were studied and introduced from White and Panjabi and it is not purpose of this book chapter to analyse them.
Beside the kinking image in lateral acquisition the presence of a sagittal displacement of two vertebral bodies gets a clear meaning of instability. The dislocation occurs in flexion and disappears in reclination. A step of more than 3.5 mm is referred from White and Panjabi as a severe instability where the neurological structures are put at risk [20, 14]. Daffner proposed as rule of thumb 2 mm to define a normal finding [21].
According to White and Panjabi a segmental kyphosis of more than 11° is defined as pathologic [20, 14]. The pathological substrate of a segmental kyphosis is fragmentation of vertebral body or discoligamentary disruption.
Concerning subluxation of the facetary joint, White and Panjabi give 50 % of overlapping as limit between stable and unstable lesion.
Increased intervertebral disc space, increased shadow of the connective prevertabtral tissue (normal values: 10 mm C1; 4 mm C3-C4; 15 mm C6) and interspinous widening are others signs of radiologic instability [7].
Diagnosis
Physical exam of the patient has a central role for the evaluation of the patient before the radiogram. The sensitivity of the spontaneous pain and palpatory pain was reported to be respectively of 86 and 79 % [22]. Clinical exams and neurological exams with indicative signs for cervical column lesion was found have a sensitivity of 93 %.
A standardized process to reach the correct diagnosis is not defined. We recommend:
Direct or third person history outline
Thoroughly patients examination.
Acquiring of three standard radiographs: anteroposterior, lateral and transoral.
Swimming acquisition if the cervicothoracal passage is not well visualized.
Oblique acquisition to clarify different questions about articular processes or small vertebral joints as the foramina intervertabralia
Computer tomography is necessary if a bone injury is already visualized or just suspected
The magnetic resonance in every case of neurological lesion, or incongruence between the clinical findings and radiological finding.
Conventional radiography is the basis for the diagnostic of lesion of vertebral column.
Daffner proposed a systematic evaluation of plain radiogram with the ABCD rule. “A” for alignment and anatomy abnormalities; “B” for bony integrity abnormalities; “C” for cartilage (joint) space abnormalities and “S” for soft tissue abnormalities [23].
Most of these signs are combined or associated and are not to be found as isolated finding.
Is not always possible to do immediately the dens view because the patient has to be compliant .
The proper AP view is made with rays inclined 20° cranially and with centered cricoid.
The proper lateral view shows always the 7th cervical vertebral body, the intervertebral disc between C7 and T1 and the endplate of T1 [24, 25]. If necessary is necessary to pull on the patient’s arms to avoid overlap of the images.
The anteroposterior and lateral views play a main role in the diagnoses, which help us to understand the stability and not to prove instability. The instability is clarified individually for each patient with all necessary and available diagnostical studies (see chapter “Radiologic assessment”).
Patients presenting consciousness impairment, intoxications, neck pain or midline tenderness or severe associated injuries should undergo a complete radiologic assessment of the cervical spine.
The role of functional radiological studies is debated and with the wide spreading of CT and MR techniques the importance of such study is very limited.
In case of symptomatic patient with suspect radiography the indication for a CT to clarify the possible skeletal lesion should be posed. In presence of radiographic instability criteria or neurological deficit an MR investigation is justified.
CT is the tomographic methods of choice in acute spinal injury [26] and should precede supplemental studies (MRI, functional radiograms and digital subtraction angiography).
The sensitivity of the CT study is considerably higher than radiographs (e.g., 98 % versus 52 %) [27].
MRI is always more popular for the study also in acute setting thanks to the reduction in the time of scanning and processing and the availability of devices for traction compatible with magnetic field.
The MRI study can discover ligamentous disruptions not visualized with other imaging techniques.
In some cases also vascular dysfunction can be visualized with MRI, albeit DSA and angio-CT remain investigations of choice to clarify these situations. Indications and timing of the MRI study remain anyway a topic of debate [28]. Commonly, MRI is administered sub acutely as help to surgical planning.
With the MRI we can achieve adjunctive information which are not recognized with other imaging systems. For example many hyperintense signals which are defined as “indeterminant” can be signs for instable injuries. When MR sequences detect changes of signal in the facet capsules, interspinous ligament and disc space a pathologic process is objectivized but the clinical meaning remains not unknown [12]. Also injuries of the neck muscles or perivertebral hematoma are detected with high sensibility with the MRT.
Of all the severe injuries of the vertebral column 80–90 % has no neurological deficit. Anyway exists an absolute indication for use of MRI in acute neurological imparment [29].
Treatment
The optimal management of cervical spine injuries is still a matter of debate and the choice of treatment has to consider multiple variables such as clinical patient conditions, stability of the lesion and presence of deformity [30].
Conservative Treatment
A conservative management is the treatment of choice in case of stable, non-displaced cervical injuries without neurological deficit. The Philadelphia collar is the most used rigid system of external stabilization for the intermediate and lower cervical spine (Fig. 18.5). It allows a good stiffness in flexo-extension maneuvers even if it limits only partially the axial rotation. In case of association of a lesion on the craniocervical junction between C0 and C2 a more rigid rotation stabilization device such as a halovest has to be considered while in case of lesion on the cervico-thoracic junction the stability may be assured by a rigid collar with thoracic prolongation. The duration of the cervical external immobilization can vary according to the severity of the lesion but in general doesn’t last before 8 weeks of treatment.


Fig. 18.5
Image of a rigid cervical collar type Philadelphia
Surgical Treatment
The main goals of the surgical treatment of traumatic cervical injuries are to decompress the neurological structures, to restore the vertebral alignment and to guarantee the stability of the injured spine. In case of lesions provoking an anterior or posterior displacement of vertebral structures with consequent neurological impairment, the surgical treatment is for sure to be preferred. In case of incomplete spinal cord lesion, the surgical stabilization should take place in the first 8 h while in case of complete spinal cord lesion the surgical treatment window is 72 h [30]. When distinguishing between complete or incomplete lesion is not possible, an early stabilization is to be preferred to avoid secondary dislocations. It is worldwide accepted that a prompt operative treatment provide less complication and reduce the time of intensive care [31].
In case of acute spinal cord injury Methylprednisolone sodium succinate has been shown to improve neurologic outcome up to 1 year post-injury if administered within 8 h of injury and in dose regimen of: 30 mg/kg over 15 min, with maintenance infusion of 5,4 mg/kg per hour infused for 23 h [32].
Nevertheless quite often the initial radiologic assessment shows minimal dislocation without neurological symptoms. In these situations the severity of the injury can be assessed with complementary diagnostic exams such as MRI which can provide further informations concerning the integrity of the discoligamentary structures. The superiority of surgical over the conservative treatment in these situations is still not proved [33, 34]. Anyway the operative treatment allows a reduction of hospitalization and rehabilitation time [35–37]. Moreover the diffusion and standardization of surgical procedure have contributed to the tendency to privilege the surgical option.
The treatment decision has to be tailored on the patient case by case.
Cervical Axial Traction
In case of vertebral disallignment the restoration of the physiologic cervical lordosis is an independent parameter of good clinical result in term of axial pain. It is well known that the reduction of post-traumatic cervical misalignment can be very challenging and the utilization of cervical axial traction is still very useful either in non-operative close reduction of facet luxation and fractures or in preoperative and intraoperative open reduction maneuvers. The weight that has to be applied for axial traction through a head holder (such as Garden-Wells) depends on the level of the lesion and on the entity of the displacement [7].
Surgical Approaches
Two main surgical approach can be used to treat a lesion of the intermediate and lower cervical spine: the anterior approach has the advantage to allow good restoration of the cervical lordosis and it is in general preferred when a high comminution of the vertebral body imply a vertebrectomy, the posterior approach allows instead a good surgical decompression but can exitate in a kyphotic cervical disbalance. Familiarity of the surgeon with the technique and available equipment plays a role in the choice. On the patient’s side the anterior approach presents the risk of temporary dysphagia or hoarse voice, neck scar, and injury to visceral structures (esophagus) on the contrary the posterior approaches expose to local wound infection and paraspinal muscle damage. Indeed the anterior approach can be preferred to avoid the prone position in traumatized patient; disc herniations can be directly removed and restore of segmental lordosis is possible [38–41]. The criticism of the anterior approach for cervical subaxial trauma is its biomechanical inferiority when compared with posterior fixation [42, 43].
Generally burst and compression fracture with dorsal herniation or dorsal fragments dislocation of vertebral body are treated by an anterior fixation [44] while unstable translation and rotation lesions are usually treated from posterior or from combined anterior and posterior approaches [45]. In chronic dislocations posterior approach is generally preferred.
Anterior Approach to the Cervical Spine
In 1950 three independent authorships developed this access: Bailey and Badgley [46], Robinson and Smith [47] and Cloward [48] which allowed a good exposition of discs, vertebral bodies and uncovertebral joints from C3 to Th1, representing an elegant solution to treat cervical pathologies.
The split of the stilohyoid muscle and of the posterior belly of the digastric muscle allows to reach C2. Distally the Th2 and Th3 vertebral bodies can be reached with sternotomic prolongation approach.
(i)
Position of the patient
Supine on radiolucent operating table with neutral position of the head.
Extension of the neck is improved with a small sandbag between the shoulder
If motor evoked potential (MEP) and somatosensory evoked potential (SSEP) monitoring is available the head can be extended and distraction applied (after halter traction or taping of the chin) and turned away of the operative side to enlarge the operative field. Inhaling narcotics should be adapted to the neuromonitoring devices.
(ii)
Reference points
Several reference points are available in the anterior approach, making easier to determine the incision level:
Lower border of the mandible: C2-3
Hyoid bone: C3
Thyroid cartilage: C4-5
Cricoid cartilage: C6
Carotid tubercle (large tubercle adjacent to the carotid pulse on the anterior part of the transverse process of C6): C6
Sternocleidomastoid muscle origins from the mastoid process and attach to the sternum and clavicle. Turning the head controlaterally makes its relief more prominent.
Carotid artery pulse can be touched on the medial edge of the sternocleidomastoid muscle with gently pressure posterior and laterally.
(iii)




Incision
Once chose the level a transverse skin crease incision is performed. The incision is usually oblique mediolaterally to the posterior border of the sternocleidomastoid muscle.
The platysma can be incised without innervation problems (supplied by facial nerve, VII cranial nerve).
In the deeper layer there is a internervous plane between the medial strap muscles of the neck (segmental innervation from C1, C2 and C3) and the sternocleidomastoid muscle (spinal accessory nerve, XI cranial nerve).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








