Stacie Segebart
Falls are the leading cause of injury death among persons aged 65 years and older. Between 30% and 40% of community-dwelling adults fall each year (4). Fall-related death rates and hip fracture hospitalizations have been increasing over the years (13).
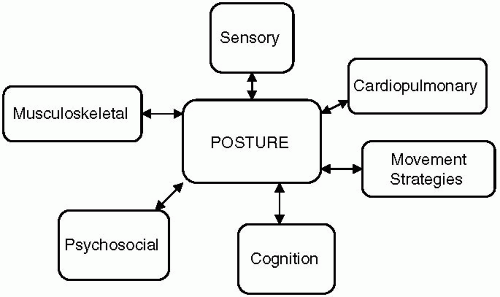
This chapter covers a generalized approach of physical therapy evaluation and intervention for prevention and management of falls. Therapeutic intervention is based on various components of a comprehensive evaluation. A systems model will be discussed in a broad spectrum that will help to drive treatment focus and intervention with each individual’s presentation. Common clinical tests of impairments and function will be overviewed along with computerized dynamic posturography.
EVALUATION
Effective patient management requires a multidisciplinary approach that focuses on pathology, impairments, and resultant functional limitations. The therapy evaluation is pertinent in driving the choice of therapy intervention.
As seen in Figure 9-1, there are multiple variables that have an effect on a person’s balance. Problems within any of these components can result in a loss of balance and falls. Therefore, a comprehensive evaluation that considers all of these systems is critical when setting up a treatment regimen to establish optimal balance rehabilitation and fall prevention (6).
The muscular contractile component, along with joint mobility, refers to sequencing, scaling, and timing of muscular contractions and plays a role in body position and movement, as well as posture and alignment during standing and sitting.
Balance involves the interaction between three sensory systems: visual, vestibular, and somatosensory. Visual input relays information about our environment and our body location. It measures head and eye position relative to the surroundings. Information relating to movement of our body and joints is provided by the somatosensory system. It associates our body location in relationship with our support surface and gravity. The vestibular system measures the head position relative to our self and gravity.
Age-related changes affect the sensory systems and motor components, which coincide with issues involving balance (2). In order to maintain postural stability, the sensory system needs to effectively detect movement, while the motor systems strategize to move the center of mass. Attention to the organization and processing of these senses is also compromised by age-associated changes. Our environment constantly challenges us as individuals. Although hearing plays a minor role in fall prevention, it should also be considered during treatment intervention because an individual may react to a loud noise by turning their head and causing them to react to a weight shift and vestibulo-ocular response requirements.
Various movement strategies, such as the ankle strategy, hip strategy, and stepping response, are used for postural control during an external perturbation. These strategies are based on the size of the perturbation and the size of the support surface. For example, the ankle strategy is used in situations of small perturbation, whereas the hip strategy is used during larger perturbations. The stepping response occurs when the movement of the center of mass moves outside the base of support. Due to the importance of each response in preventing falls, therapy intervention should focus on developing the ability to use the appropriate strategy at the right time in both static and dynamic situations.
The cognitive status of a patient will also determine the success of balance management for several reasons. First, one must determine whether the patient is able to learn and adapt to various environmental situations. Second, the patient will also need to be capable of integrating the various strategies in an environmental challenge. Therefore, greater understanding of the cognitive capacity and attention span of the patient will help to strategize your therapy intervention.
The patient’s overall health status will make a difference in treatment approach as well. Cardiovascular changes as a result of aging or pathology could result in lowered aerobic capacity, decreased exercise tolerance, or orthostatic hypotension. Questioning the individual about their activity levels can help to drive the treatment and length of intervention. The 6-minute walk test, which measures the distance an
individual walks in 6 minutes, is a tool used in therapy to help document a patient’s overall functional endurance during ambulation.
individual walks in 6 minutes, is a tool used in therapy to help document a patient’s overall functional endurance during ambulation.
The psychological status of a patient is another critical variable in determining outcome of therapy. Depression can have a direct and indirect impact. It can affect postural control. Abnormal extensor muscle tone may limit the patient’s ability for good postural control and alignment. The patient’s motivation can also limit the treatment avenues and functional outcomes.
Patients are not always ready to accept certain safety measures, or they can become resistant to using an assistive device. If a patient has a positively skewed sense of self-efficacy, he or she may feel that a device is not necessary. In contrast, a patient’s fear of falling can be great enough to result in avoidance of situations considered to be risky.
The treatment of these challenging patients is approached in numerous ways depending upon the individual. At times, the objectivity of a functional test may be proof enough to the patient that they are at risk of falling. To help objectively measure a person’s fear of falling, several scales have been developed. The Falls Efficacy Scale (FES) has been developed for measuring fear of falling (14). Also correlated with the FES test is the Activities-Specific Balance Confidence (ABC) scale, which is administered to the patient addressing any fears of falling that impact life’s activities. The ABC test has a wider continuum of activity difficulty in regard to activities of daily living (8). The Dizziness Handicap Inventory (DHI) is a multidimensional self-assessment tool that addresses the emotional, functional, and physical aspects that quantify the level of disability and handicap of a patient. The test measures the self-perceived impact that imbalance or dizziness has on the quality of life and psychosocial well-being of the patient (3). In the evaluation process, detection of individuals at risk for falls is an important concept that should be used in any health care setting.
Having a simplified systematic tool for detection of fall prevention should be integrated into the therapy evaluation process. At the beginning of therapy, the patient should be asked to complete a generalized form, and then the questions can be discussed in the subjective format of the therapy evaluation. Questions should be concise and include the various risk factors of falling so that treatment intervention can be targeted specifically for home safety and modifications can be made to prevent falls (9).
FUNCTIONAL TESTS
Functional testing helps to summarize the nature of a balance problem and provides objectivity in an evaluation. The results help physical therapists to direct treatment and focus on objective goal setting. Table 9-6 lists the most commonly used functional balance tests.
The Balance Evaluation Systems Test (BESTest) is a comprehensive tool that is divided into six sections: Biomechanical Constraints, Stability Limits/Verticality, Transitions/Anticipatory, Reactive, Sensory Orientation, and Stability in Gait. The test was designed by Fay Horak to identify principal issues of a patient’s balance problem.
The Timed Up and Go (TUG) is a quick testing tool to implement in the clinic. For this measure, the subject stands up from a standard chair and walks 3 m, turns around, and then returns to sitting while being timed. This test has been shown to be a sensitive and specific measure for identifying community-dwelling
adults who are at risk for falls (11). Scoring is represented in Table 9-7.
adults who are at risk for falls (11). Scoring is represented in Table 9-7.
Table 9-6. Common Functional Balance Tests | ||||||
|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree