Fig. 7.1
Right MCA thrombectomy. (a) Right MCA is occluded at its origin (arrow). (b) Super-selective microcatheter injection demonstrates placement of the microcatheter tip (arrow) distal to the clot burden. (c) The distal tines (arrow) of the stent retriever are seen at the level of the right MCA bifurcation. (d) The right MCA remains patent after retrieval of the stent retriever
Acute Vertebrobasilar Occlusion
Vertebrobasilar occlusions account for about 3 % of all acute intracranial large artery strokes [25] with high mortality rates ranging 40–80 % in some studies as well as a high likelihood of poor functional outcome among survivors [26, 27]. Achieving recanalization results in significant reduction in mortality [28]. In one study, the length of the occluded segment and extent of collaterals were independent predictors of survival. Even though the time window for achieving recanalization could be longer in the posterior circulation, one study reported higher recanalization rates if treatment was initiated within 6 h of onset [29].
Illustrative Case 2 (Basilar Occlusion)
A 67-year-old man with a history of hypertension, hyperlipidemia, and diabetes acutely developed dizziness with nausea and vomiting. His neurological exam progressively worsened, and the patient required intubation for altered mental status and respiratory compromise. He underwent a CT angiogram that demonstrated occlusion of the basilar and extracranial left vertebral arteries. The patient underwent a cerebral angiogram that confirmed basilar thrombosis. A 6-French guiding catheter was advanced into the right vertebral artery. With the aid of a microwire, a microcatheter was successfully navigated through the basilar thrombosis. Distal positioning of the microcatheter tip was confirmed with a super-selective injection. A Solitaire device was then successfully deployed across the basilar thrombus and immediately improved flow. After a 5-min deployment, the Solitaire device was removed. Subsequent imaging demonstrated patency of the basilar artery with an unintended branch occlusion of the right posterior inferior cerebellar artery (Fig. 7.2).
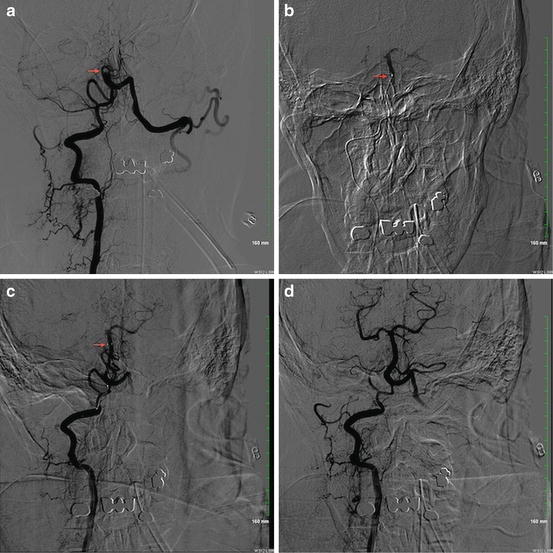
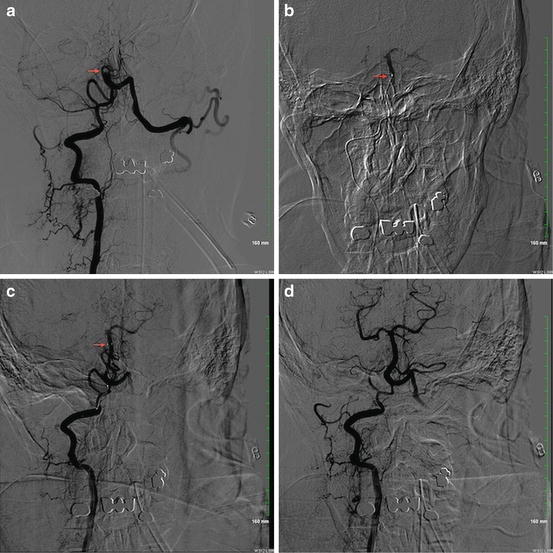
Fig. 7.2
Basilar artery thrombectomy. (a) Complete occlusion of the basilar artery is seen at the level of AICA (arrow). (b) Super-selective microcatheter injection demonstrates placement of the microcatheter tip (arrow) distal to the clot burden. (c) The distal tines (arrow) of the stent retriever are seen at the level of the distal basilar artery. (d) The basilar artery remains patent after retrieval of the stent retriever
Carotid-T Occlusions
Terminal internal carotid artery (ICA) occlusions with the thrombus extending into the origin of ipsilateral A1 and M1 segments are associated with high clot burden, poor collateral flow, and poor outcomes. Earlier studies investigating intra-arterial infusion of thrombolytic agents reported poor recanalization and unfavorable outcomes in carotid-T occlusions [30, 31]. A recent study reported significant improvement in recanalization rates with mechanical thrombectomy using Solitaire in patients with ICA-T occlusions without any additional increase in symptomatic intracranial hemorrhage [32].
Illustrative Case 3 (Carotid-T Occlusion)
A 42-year-old man with recently diagnosed renal infarct presented with the acute onset of aphasia and right-sided weakness. He was administered IV thrombolytics and his symptoms transiently improved but then returned. CT angiogram and perfusion studies were performed that demonstrated a left intracranial ICA occlusion with significant penumbra in the left hemisphere. A cerebral angiogram was then performed which demonstrated a left carotid-T occlusion with no flow beyond the posterior communicating artery segment. A Penumbra reperfusion catheter was advanced into the occluded intracranial carotid, and a thrombectomy was performed with continuous aspiration and a separator wire. After recanalization of the left ICA, the reperfusion catheter was advanced into the distal left MCA, and an additional thrombectomy was performed with continuous aspiration and a separator wire. Subsequent angiographic imaging from the guide sheath demonstrated recanalization of the left MCA. There was unintended branch occlusion of the ipsilateral anterior cerebral artery that resolved spontaneously. The stroke evaluation also included an echocardiogram that demonstrated severe stenosis of the aortic valve with left atrial enlargement secondary to childhood rheumatic heart disease (Fig. 7.3).
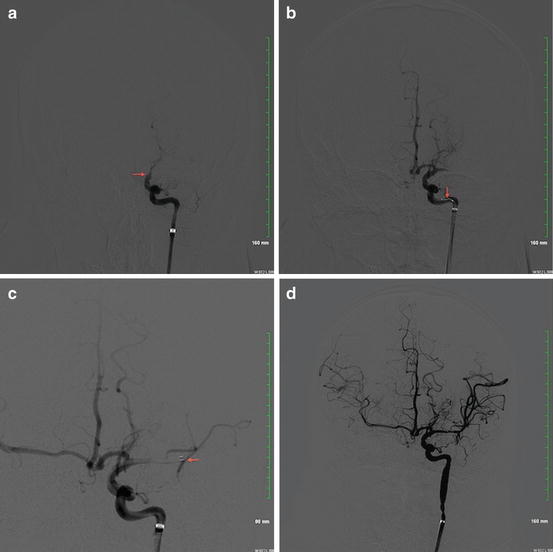
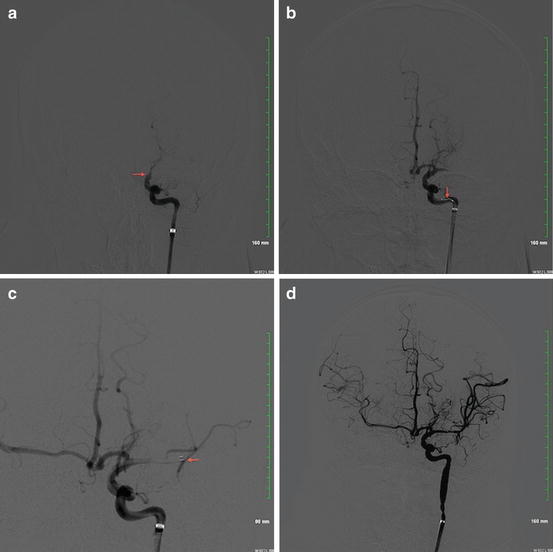
Fig. 7.3
Carotid-terminus thrombectomy. (a) Complete occlusion of the left ICA is seen at the level of the posterior communicating artery segment (arrow). (b) The left ICA is recanalized with the aid of the separator wire (arrow) and reperfusion catheter. (c) The reperfusion catheter (arrow) is advanced into the occluded left MCA and aspiration is performed. (d) The left MCA remains patent after removal of the reperfusion catheter
Tandem ICA/MCA Occlusions
Occlusions of cervical ICA and ipsilateral MCA comprise about 7 % of all acute intracranial large artery ischemic strokes [25]. Tandem ICA/MCA occlusions are associated with poor outcomes after intravenous thrombolysis [33]. Revascularization of the proximal ICA with stent placement and angioplasty followed by mechanical thrombectomy to achieve recanalization of the intracranial arterial occlusion has been demonstrated as safe and feasible with reported good recanalization rates and functional outcomes [34–36]. This technique has also been reported to be safe and feasible in tandem ICA/MCA occlusions in the setting of acute ICA dissection [37].
Illustrative Case 4 (Tandem ICA/MCA Occlusion)
A 52-year-old man without significant past medical history acutely developed vision loss in the right eye and left hemiparesis. He received intravenous thrombolytics in the emergency room, but his deficits persisted. A subsequent cerebral angiogram demonstrated a flame-shaped taper of the right ICA most consistent with a dissection. A Penumbra reperfusion catheter was successfully navigated distal to the carotid dissection. Subsequent super-selective angiographic imaging demonstrated complete occlusion of the right MCA at its origin. A carotid stent was deployed across the dissected segment of the cervical ICA. We did not administer heparin or antiplatelet agents since IV thrombolytics had been administered. A Penumbra reperfusion catheter was then advanced into the right MCA, and the thrombectomy was performed with continuous aspiration and a separator wire (Fig. 7.4).
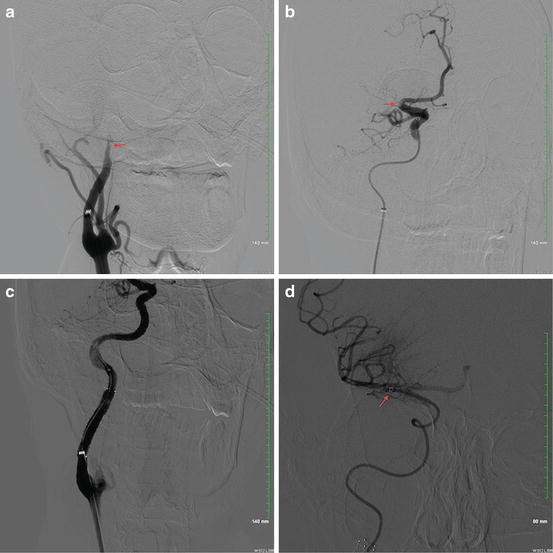
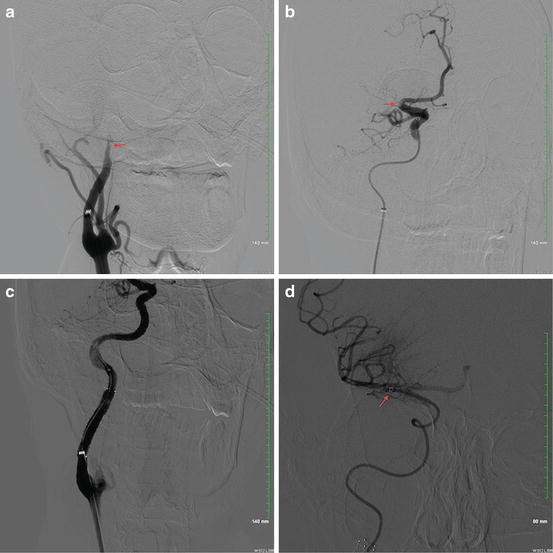
Fig. 7.4
Endovascular treatment for tandem occlusion—carotid artery stenting followed by MCA thrombectomy. (a) The cervical right ICA demonstrates a flame-shaped taper (arrow) consistent with a dissection. (b) Super-selective angiogram distal to the carotid dissection demonstrates occlusion of the right MCA (arrow). (c) Successful deployment of a carotid stent across the dissection results in recanalization of the right ICA. (d) The reperfusion catheter (arrow) is successfully advanced into the right MCA for thrombectomy
Acute Large Artery Occlusion in Anticoagulated Patients
Patients with acute ischemic stroke receiving coumadin (with INR > 1.7) or newer anticoagulants are considered ineligible for IV thrombolysis due to perceived risks of ICH. Case series have reported safety and feasibility of IAT in patients receiving therapeutic doses of anticoagulants [38, 39]. The American Heart Association/American Stroke Association (AHA/ASA) guidelines also recently suggested endovascular therapies as a reasonable approach to treat patients with acute large artery occlusions in whom IV thrombolysis is contraindicated [40].
Complications Associated with IAT in Ischemic Stroke (See Chap. 3)
Certain complications such as arterial dissections/perforations, contrast-induced renal dysfunction, and groin hematomas can occur in any endovascular procedure. However intracranial hemorrhage occurring post-procedure is specifically associated with IA thrombolysis for ischemic stroke. Earlier studies reported an incidence of ICH on follow-up CT scans in almost 50 % patients following IA thrombolysis [41]. However majority of these patients (43 %) had an asymptomatic ICH that was considered a marker of reperfusion and did not adversely affect outcomes. The recently concluded IMS-III and MR RESCUE trials [42, 43] reported rates of symptomatic ICH in the range of 4–6.2 % indicating that IA thrombolysis can be performed safely. Reducing the number of microcatheter contrast injections during the procedure has been suggested as a way to reduce the risk of hemorrhagic conversion [44].
Periprocedural Management (See Chap. 3)
The role of general anesthesia (GA) and intubation pre-procedure is controversial. In one retrospective study, poorer neurologic outcomes and higher mortality were noted in patients receiving GA when compared to conscious sedation [45]. It has been postulated that treatment delays associated with intubation and blood pressure changes associated with induction of GA could be factors affecting overall prognosis. Many centers therefore prefer conscious sedation whenever possible to minimize delays in therapy. Patients should be observed closely in an intensive care unit with close attention to the neurologic as well as hemodynamic monitoring following protocols similar to post-IVT.
Conclusions
References
1.
2.
Brückmann H, Ferbert A, del Zoppo GJ, Hacke W, Zeumer H. Acute vertebral-basilar thrombosis. Angiologic-clinical comparison and therapeutic implications. Acta Radiol Suppl. 1986;369:38–42.PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








