Fig. 1
Typical pattern of AP dynamics measured invasively in aorta: (1) peak systolic pressure; (2) dicrotic notch; (3) diastolic pressure; (4) anacrotic notch [5]
Dicrotic notch occurs at the instant of the closing of the aortic valve, when the pressure in aorta becomes higher than in the left ventricle. This moment signifies the end of systole and the beginning of diastole. An anacrotic notch occurs at the beginning of systole, before the instant of the opening of the aortic valve, and is only observed during monitoring of the pressure in the aorta, or during certain pathologic conditions [5]. To summarize, existing methods to study cerebral perfusion exhibit a series of limitations: invasiveness, insufficient accuracy, and high probability of diagnostic errors. Thus, improvement is needed.
Materials and Methods
This study of the procedure for invasive measurement of AP was conducted during endovascular operations on 19 patients. Operations were performed on patients with ruptures of anterior circulation arterial aneurysms. Real-time comparative recordings of AP were performed in the internal carotid artery (ICA) inside and outside of the skull cavity, and also inside the aneurysm lumen; AP was also measured noninvasively on the humeral artery with a blood pressure cuff.
The invasive monitoring of AP was executed under fluoroscopic control during different stages of operation; in the magisterial artery, with standard guiding catheters (length, 100 cm; internal diameter, 1.63 mm) and, in the cavity of the aneurysm, with a standard microcatheter (length, 150 cm; internal diameter, 0.4 mm). Measurements of AP in the magisterial artery both inside and outside of the skull cavity were conducted through a standard microcatheter. Invasive measurement of AP inside the skull cavity was conducted in the proximal (vertical) part of the C4 segment of the ICA. Outside the skull cavity, the measurement was carried out in the distal part of the C1 segment of the ICA (Fig. 2). Results were recorded by the monitor “Utas” UM 300 with the help of a transducer that was calibrated, then attached through a liquid line to the cannula of the catheter. Before every measurement, the sensor was calibrated. Data was processed for statistics on a personal computer with the program “Statistic 6.0”.
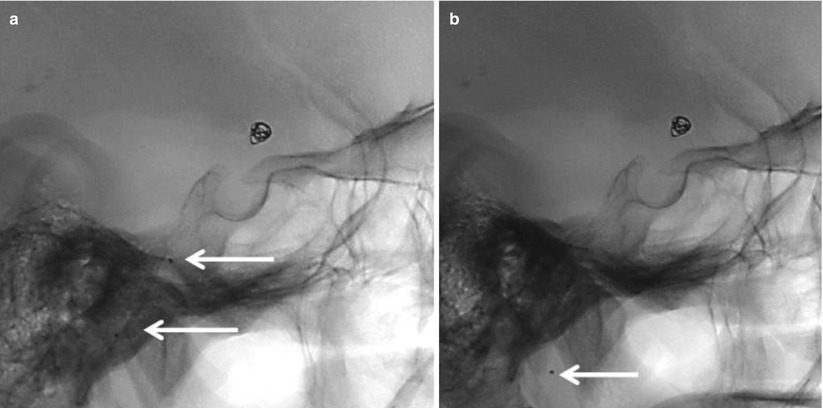
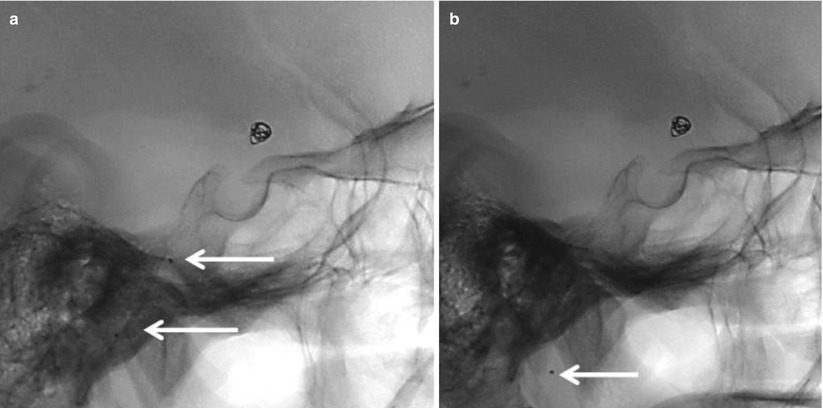
Fig. 2
Position of marks of microcatheter (arrows) during measurement of pressure in the segment C4 of ICA (a) and in the distal part of C1 segment of ICA (b)
Results and Discussion
Principles of Invasive AP Monitoring During Endovascular Neurointerventional Procedures
We conducted a series of simultaneous measurements of AP through catheters of different diameters (a guiding catheter and microcatheter) in the extracranial section of the ICA (segment C1). We observed that the amplitudes of fluctuations during measurements through the microcatheter were decreased, which was reflected in smaller values of systolic and pulse pressures and also in the growth of the diastolic pressure. These differences can be explained by the peculiarities of the functioning of the system with a high dumping coefficient, where elastic and very long tubes (the microcatheters) were used. The length of the catheter should not exceed 3–4 ft (91–122 cm) [2], and the length of the microcatheter, 150 cm. The patterns are shown on a curve recorded from the monitor (Fig. 3).
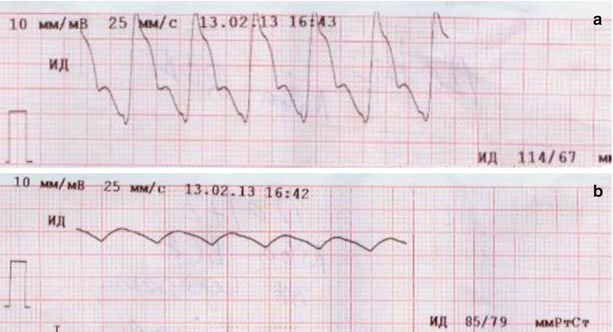
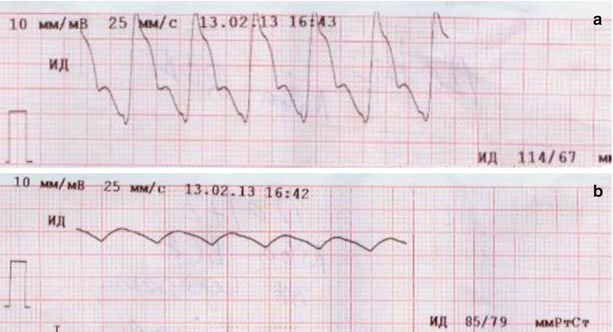
Fig. 3
A record of the direct measurements of AP in ICA: (a) through a guiding catheter; (b) through a microcatheter
According to our data, measured values of MAP (a basic characteristic of the perfusion pressure) are practically independent of the catheter diameters. They are 98.3 ± 5.6 mmHg on average, if measured through a guiding catheter; and 102.4 ± 6.3 mmHg, if measured through a microcatheter; p > 0.5. When measured by a noninvasive method on the humeral artery, MAP was recorded to be 103.8 ± 4.9 mmHg. Thus, MAP appears a precise parameter independent of the method of AP measurement (see Table 1). This explains why we will use this index for establishing the main characteristics of cerebral hemodynamics and brain perfusion in the future.
Table 1




AP parameters measured by cuff and directly, through catheters of various inner diameter
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





