Chapter 5 Intradural Extramedullary Cystic Lesions
INTRADURAL ARACHNOID CYST
EPIDEMIOLOGY
• They are divided into acquired cyst and congenital cyst. Acquired arachnoid cysts are more common and can be the result of spinal cord trauma, postsurgical arachnoiditis, meningeal infection, and other insults that cause inflammation and subarachnoid adhesions.1
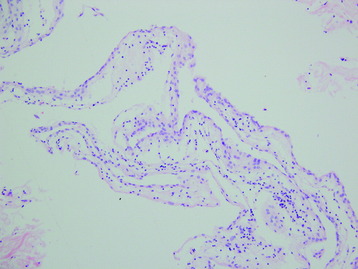
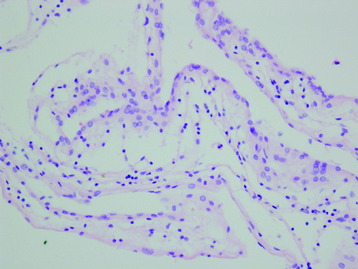
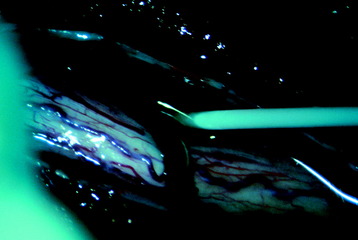
• Congenital or idiopathic spinal arachnoid cysts are diagnosed when there is no antecedent history of trauma or other etiologic factors and the intraoperative macroscopic and microscopic findings show a cyst wall composed of normal or slightly thickened arachnoid tissue.
• Various theories have been proposed to explain the formation of arachnoid cysts.2 Perret et al3 proposed that they arise from diverticula in the septum posticum. However, reports of cysts ventral to the spinal cord suggest that there must be another origin.4 Incarceration of arachnoid granulations may produce CSF that becomes entrapped in arachnoid diverticula. These sequestered pockets of fluid lead to further disruption of normal pulsatile CSF flow and thus are capable of expanding or producing associated syringomyelia.5,6
DISTRIBUTION
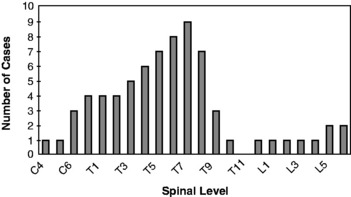
• The regional distribution of the spinal arachnoid cyst is presented in Fig. 5-1.2 Most of them are located in the thoracic region (80%), as compared with 15% in the cervical spine and 5% in the lumbar spine.
• Most of the arachnoid cyst is located dorsal to the spinal cord. In a review of the six published series that specified the arachnoid cysts’ location, 12 of 69 (17%) of the cysts were anterior to the spinal cord.5,7
• They may be single or multiple. Men and women are equally affected and usually in the third through fifth decades of life.
RADIOLOGY
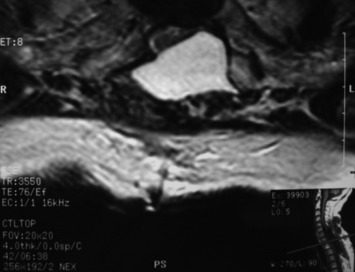
• The primary magnetic resonance imaging (MRI) finding is a spinal space–occupying mass, nonenhancing extramedullary loculated CSF collection.
• T1- and T2-weighted signals of arachnoid cyst are identical to those of CSF. There is no enhancement with gadolinium use.
• Intradural arachnoid cysts are poorly delineated on MRI because the signal intensities of both the cysts and the surrounding CSF space are more or less the same.
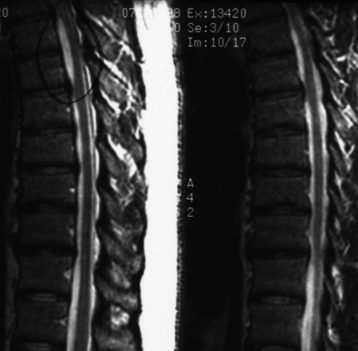
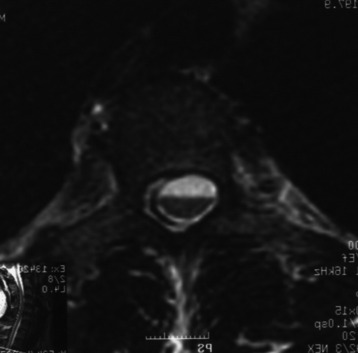
• Widening of the posterior CSF space on MRI, with anterior displacement and thinning of the spinal cord, may be the only sign of intradural arachnoid cyst (Figs. 5-4 and 5-5).8
• MRI results have been reported showing segmental clear-cut dilatation of the posterior CSF space, at one or two vertebral levels, with focal thinning of the neural structure, thus providing a definite diagnosis of intradural cysts.8
• However, because of the chronicity of this disorder, intradural arachnoid cysts may distend very slowly and elongate over multiple vertebral levels.
• Inhomogeneous areas of hypointense T2-weighted signal with respect to the surrounding CSF may be seen. This phenomenon is consistently interpreted as artifacts from aortic pulsations into CSF (see Figs. 5-4 and 5-5).9
• Anterior cysts are more likely to cause weakness and myelopathy, whereas dorsal cysts present more commonly with neuropathic pain and numbness (Figs. 5-6 and 5-7).