Chapter 6 Intradural Extramedullary Malignant Tumors
MALIGNANT PERIPHERAL NERVE SHEATH TUMOR
EPIDEMIOLOGY
• Neurogenic tumors may arise from peripheral nerves or nerve sheaths, or from sympathetic ganglions.
• The tumors that arise from peripheral nerves or nerve sheaths include neurofibroma, neurilemmoma (schwannoma), and malignant nerve sheath tumors. Tumors from sympathetic ganglions are ganglioneuroma, ganglioneuroblastoma, and neuroblastoma. Nearly 85% of tumors in children are ganglion in origin whereas, in adults, more than 75% are nerve sheath tumors.1
DISTRIBUTION
• The majority of MPNSTs are derived from neurofibroma or arise de novo in normal peripheral nerves.2,3
• There were only very rare cases arising in malignant transformation of benign schwannoma or sympathetic ganglion tumors.4 Large and medium-sized nerves are more often involved than small nerves. Common sites of origin include the sciatic nerve, brachial plexus, and upper arm. MPNSTs affect young to middle-aged adults, with a slight female predominance.
• Neurofibromatosis type 1 (NF-1) predisposes to the development of MPNSTs. About 50–60% of MPNSTs occur in patients with NF-1.2,3 In addition to hereditary factors, exposure to ionizing radiation also may play a role in the development of MPNSTs.
HISTOLOGY
• The malignant nerve sheath tumors are confined to the cells intrinsic to the peripheral nerve sheath, including the perineurium and endoneurium. These tumors are generally regarded as being of Schwann cell origin because most of them usually exhibit some evidence of Schwann cell differentiation and the small minority have the features of fibroblast or perineurial cells.
• Histologically, MPNSTs are usually more hypercellular with spindle cell proliferation. The tumor cells often show hyperchromatic nuclei and are mitotically active.4
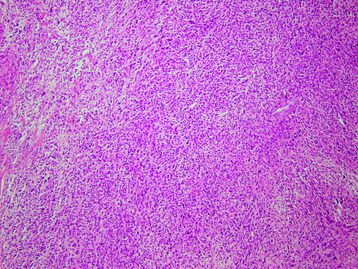
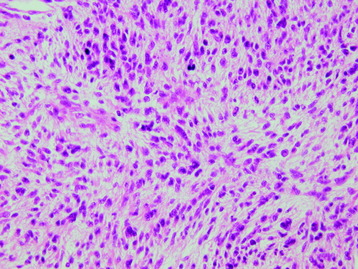
• Microscopically, the tumor shows fasciculated growth of tightly packed, hyperchromatic spindle cells (Fig. 6-1). The fibrosarcoma-like fascicles are focally alternating with hypocellular myxoid zones, creating a marbleized appearance. Focal, subtle nuclear palisading and waving nuclei are present. Moderate cellular atypism, high mitotic activity, and foci of necrosis are also noted (Fig. 6-2).
• In the immunohistochemical studies, the tumor cells are positive for S100 and negative for cytokeratin, desmin, and CD34. Positive p53 immunoreactivity is noted in 10% of tumor cells.
RADIOLOGY
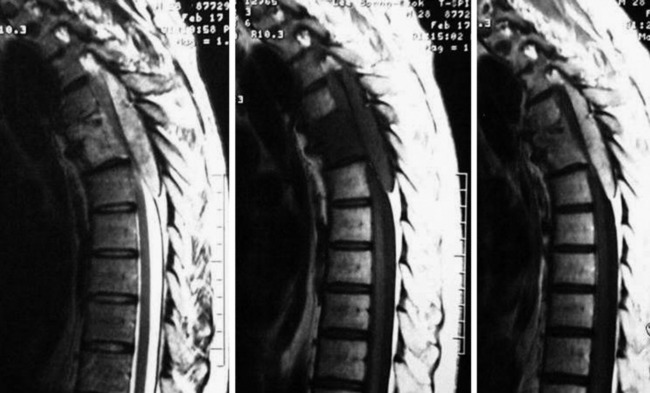
• On plain radiographs, nerve sheath tumors typically appear as sharply marginated, round, elliptical, or lobulated paraspinal masses. Intervertebral foramen widening is seen and erosion of the ribs and vertebral bodies sometimes is evident5 (Fig. 6-3).
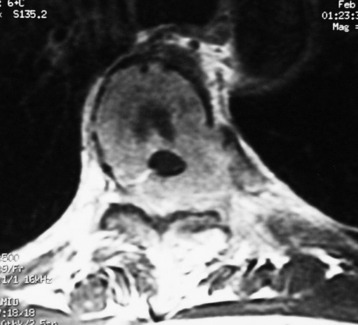
• On computed tomography (CT) scan, schwannoma has been shown to have a mixed attenuation, attributable to a confluent area of hypocellularity adjacent to dense cellularity, or xanthomatous change, or regions of cystic degeneration. Variable enhancement of the tumor may be seen after contrast infusion. Calcification (about 5–10%) may be present with either benign or malignant tumors but is not a reliable sign of benign character.
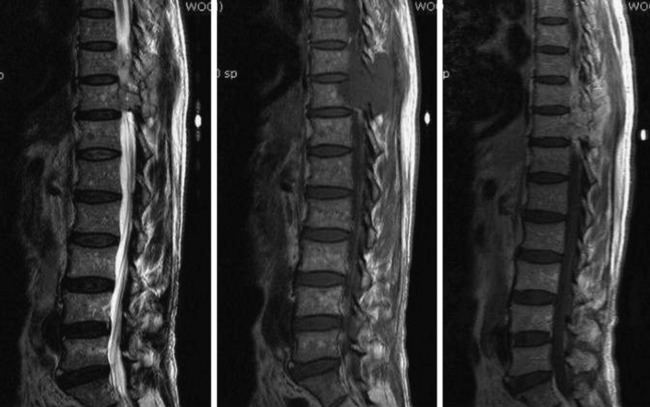
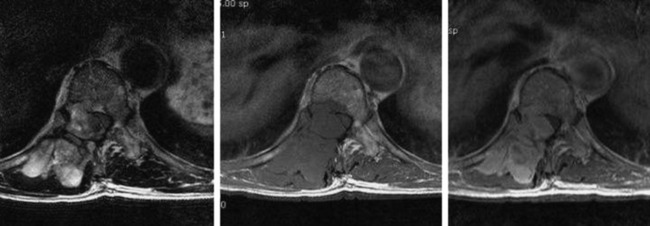
• On magnetic resonance imaging (MRI), MPNSTs typically have iso-signal intensity as muscle on T1-weighted images (T1WI) and markedly increased signal intensity on T2-weighted images (T2WI) or contrast-enhanced images, although often in an inhomogeneous fashion (Figs. 6-4 to 6-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree