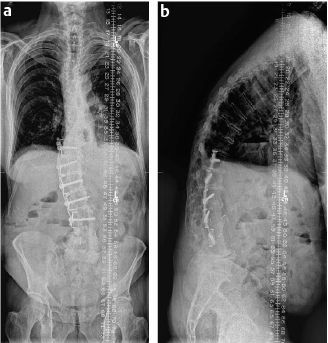
26 Both intraoperative hemostasis and coagulation management as well as postoperative venous thromboembolism (VTE) prophylaxis are crucial aspects of appropriate spine surgical care. Modern spine surgical care involves the treatment of a wide array of pathologies across a substantial breadth of surgical case complexity and, accordingly, the particular nuances of hemostasis and coagulation also vary widely in parallel with underlying etiology and degree of complexity of surgical intervention. Specific case examples are presented here to illustrate several aspects of hemostasis and anticoagulation as they relate to the care of the spine surgery patient. A 67-year-old man with a medical history of hypertension and diabetes presented with an 18-month history of progressive ambulatory dependent bilateral leg pain radiating to his lower legs. Severe pain was brought on by walking less than one city block and relieved completely with sitting or forward flexion. Physical examination identified a normal neurologic examination and normal pedal pulses. A recent magnetic resonance imaging (MRI) study showed evidence of severe central and lateral recess spinal stenosis at the L3/4 and L4/5 secondary to a combination of facet arthropathy and ligamentum flavum hypertrophy. Given the compelling clinical history and excellent radiographic correlation, a diagnosis of neurogenic claudication secondary to lumbar spinal stenosis was entertained, and the option of a minimally invasive lumbar decompression directed at the L3/4 and L4/5 spinal levels was discussed with the patient. An uneventful minimally invasive multilevel lumbar decompression was performed. The patient was positioned prone on a Jackson spinal table (OSI, Union City, CA). Intermittent pneumatic compression (IPC) was instituted preoperatively. Operative blood loss was 75 mL. Postoperatively, IPC was continued, and early ambulation was encouraged. No chemical prophylaxis was instituted. The patient tolerated the procedure well and was discharged the following morning. Simple spine surgical procedures such as diskectomies, laminectomies, and one- or two-level fusion operations do not routinely involve significant blood volume loss and, accordingly, perioperative hemostasis is often not a significant issue. However, regardless of the degree of anticipated spine surgical intervention, proper patient positioning remains important to the overall goal of minimizing operative blood and promoting effective hemostasis. The Jackson spinal table leaves the patient’s abdomen free in the prone position and therefore decreases inferior vena cava pressure and, as a result, decreases epidural venous plexus filling.1 Theoretically, this also decreases vertebral venous pressure and thus lowers intraoperative blood loss from decreased bone bleeding. Intermittent pneumatic compression is instituted perioperatively, as this method has been shown to be as effective as chemical prophylaxis for low-risk spine surgery patients. Patients undergoing simple spine surgery procedures typically ambulate in the early postoperative phase, and thus do not require chemical prophylaxis. Minimally invasive spine surgery techniques have further reduced the degree of postoperative pain typically experienced by patients, allowing for even earlier ambulation and the transition of many simple spine surgery operations to day-surgery procedures. Chemical prophylaxis is only recommended in this patient population if there are other factors that raise the risk of VTE (e.g., previous VTE, malignancy, prolonged recumbency due to perioperative medical complication). A 61-year-old man presented with a multi-month history of severe, progressive ambulatory leg pain radiating to his bilateral calves. This claudicant leg pain was occurring on the background of long-standing worsening chronic mechanical low back pain and a progressive inability to stand in an upright, erect fashion. His past medical history was significant for having undergone a T10–L3 anterolateral fusion (Dwyer procedure) for scoliosis 30 years previously and a myocardial infarction 1 year ago that was treated via percutaneous placement of a bare-metal coronary stent and dual antiplatelet therapy with clopidogrel (Plavix) and aspirin. Physical examination demonstrated a substantial thoracic kyphosis and lumbar hypolordosis. No focal deficits were identified on a neurologic examination. Standing scoliosis X-rays demonstrated his previous T10–L3 Dwyer fusion construct combined with a severe fixed sagittal imbalance measuring 17.5 cm (Fig. 26.1) as well as significant degenerative disk disease at the L4/5 and L5/S1 levels caudal to the previous fusion. Lumbar spine MRI (Fig. 26.2) revealed severe spinal stenosis both centrally and in the lateral recesses at the L4/5 and L5/S1 levels. Diagnoses of fixed sagittal imbalance and adjacent segment degeneration spinal stenosis were made. After a lengthy discussion with the patient about the pertinent risks and benefits of surgical intervention, a T3–ilium posterior instrumented fusion in combination with multiple thoracic Smith-Petersen osteotomies, a L2 pedicle subtraction osteotomy, as well as L4/5 and L5/S1 transforaminal lumbar interbody fusions was planned as a treatment for the patient’s fixed sagittal imbalance and spinal stenosis.
Intraoperative Spine Surgery–Specific Patient/Case Examples
Case 1: Spinal Stenosis
History
Procedure
Discussion
Case 2: Spinal Deformity (Fixed Sagittal Imbalance)
History
< div class='tao-gold-member'>
Intraoperative Spine Surgery–Specific Patient/Case Examples
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree