1 Introduction and History
Acoustic neurinomas are well-known benign tumors that have fascinated generations of surgeons. They represent about 8–10% of all intracranial tumors, with an incidence of around one case per 100.000 people. More than 95 % of these tumors are unilateral. The remaining patients with bilateral tumors have the pathognomonic signs of type 2 neurofibromatosis, a disease with autosomal-dominant inheritance. The three most common initial symptoms are hearing loss (about 95 %), tinnitus (about 70 %), and dysequilibrium (about 65 %). The growth rate of the tumors is unpredictable; some show no change over many years. It has been reported that as many as 6 % actually decrease in size without any treatment. On the other hand, some tumors can increase in diameter by up to 20 mm per year. The “typical” growth rate has been observed to be between 1–2 mm per year.
The clinical manifestations are so typical that this type of tumor was recognized quite early in medical history. One of the first descriptions appears to have been made in 1776 by Sandifort, in Leiden (Netherlands). He had no idea that this tumor was an acoustic neurinoma; he described a “little body hiding in the recess of the brain,” and declared it to be the reason for the clinical symptoms. The first description of the clinical symptoms attributable to an acoustic neurinoma was made almost 50 years later by Levèque-Lasourie. Perhaps the most remarkable case was reported in 1835 by Cruveilhier (Fig. 1.1), who presented the clinical case of a 26-year-old woman in remarkable detail. Henneberg and Koch first introduced the term “cerebellopontine angle tumor” in 1902. Credit should be given to Monakow for being one of the first to conclude that surgical excision of acoustic nerve tumors should be possible. However, operations at that period where usually disasters, followed by postmortem descriptions. Finger dissection was the state-of-the-art technique at that time, and only three out of eight patients survived the operation. These techniques were both bloody and traumatic to all the structures around, especially the brain stem.
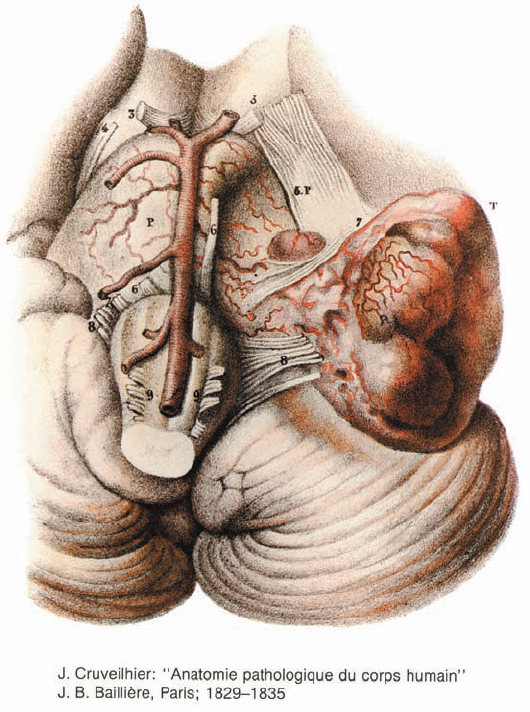
Fig. 1.1 From J. Cruveilhier, Anatomie pathologique du corps humain (Paris: Baillière, 1829–35).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








