OVERVIEW OF SLEEP STAGES AND CYCLES
The monitoring of sleep is complex and requires a distinct skill set including a detailed knowledge of electroencephalography (EEG), respiratory monitoring, and electrocardiogram (EKG). Expertise in only one of these areas does not confer the ability to accurately interpret the polysomnogram.
Sleep is not homogeneous and is characterized by sleep stages based on EEG or electrical brain wave activity, electrooculographic (EOG) or eye movements, and electromyographic (EMG) or muscle electrical activity (
1,
2 and
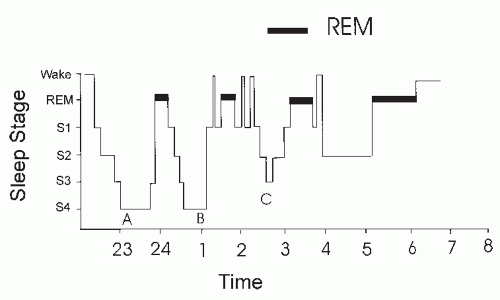
3). The basic terminology and methods involved with monitoring each of these types of activity will be discussed below. Sleep is composed of nonrapid eye movement (NREM) and rapid eye movement (REM) sleep. NREM sleep is further divided into stages N1, N2, and N3. Stages 3 and 4 sleep were recently combined into stage N3 sleep. Stages N1 and N2 are called light sleep and stage N3 is called deep or slow-wave sleep. There are usually four or five cycles of sleep, each composed of a segment of NREM sleep followed by REM sleep. Periods of wake may also interrupt sleep during the night. As the night progresses, the length of REM sleep in each cycle usually increases. The hypnogram (
Fig. 1-1) is a convenient method of graphically displaying the organization of sleep during the night. Each stage of sleep is characterized by a level on the vertical axis of the graph with time of night on the horizontal axis. REM sleep is often highlighted by a dark bar.
Sleep monitoring was traditionally by polygraph recording using ink-writing pens that produced tracings on paper. It was convenient to divide the night into epochs of time that correspond to the length of each paper page. The usual paper speed for sleep recording is 10 mm/s; a 30-cm page corresponds to 30 seconds. Each segment of time represented by one page is called an epoch; sleep is staged in epochs. Today most sleep recording is performed digitally, but the convention of scoring sleep in 30-second epochs or windows is still the standard. If there is a shift in sleep stage during a given epoch, the stage present for the majority of the time names the epoch. When the tracings used to stage sleep are obscured by artifact for more than one-half of an epoch, it is scored as movement time (MT). When an epoch of what would otherwise be considered MT is surrounded by epochs of wake, the epoch is also scored as wake. Some sleep centers consider MT to be wake and do not tabulate it separately.
SLEEP ARCHITECTURE DEFINITIONS
The term sleep architecture describes the structure of sleep. Common terms used in sleep monitoring are listed in
Table 1-1. The total monitoring time or total recording time (TRT) is also called total bedtime (TBT). This is the time duration from lights out (start of recording) to lights on (termination of recording). The total amount of sleep stages N1, N2, N3, REM, and MT is termed the
total sleep time (TST). The time from the first sleep until the final awakening is called the
sleep period time (SPT). SPT encompasses all sleep as well as periods of wake after sleep onset and before the final awakening. This wake time is termed the WASO (wake after sleep onset). Therefore, SPT = TST + WASO. The time from the start of sleep monitoring (or lights out) until the first epoch of sleep is called the
sleep latency. The time from the first epoch of sleep until the first REM sleep is called the
REM latency. It is useful to determine not only the total minutes of each sleep stage, but also to characterize the relative proportion of time spent in each sleep stage. One can characterize stages N1 to N3 and REM as a percentage of total sleep
time (%TST). Another method is to characterize the sleep stages and WASO as a percentage of the sleep period time (%SPT). Sleep efficiency (in percent) is usually defined as either the TST × 100/SPT or TST × 100/TBT.
The normal range of the percentage of sleep spent in each sleep stage varies with age (
2,
3) and is impacted by sleep disorders (
Table 1-2). In adults, there is a decrease in stage N3 sleep with increasing age, while the amount of REM sleep remains fairly constant. The amounts of stage N1 sleep and WASO also increases with age. In patients with severe obstructive sleep apnea, there is often no stage N3 sleep and a reduced amount of REM sleep. Chronic insomnia (difficulty initiating or maintaining sleep) is characterized by a long sleep latency and increased WASO. The amount of stages N3 and REM sleep is commonly decreased as well. The REM latency is also affected by sleep disorders and medications. A short REM latency (usually <70 minutes) is noted in some cases of sleep apnea, depression, narcolepsy, prior REM sleep deprivation, and the withdrawal of REM suppressant medications. An increased REM latency can be seen with REM suppressants (ethanol and many antidepressants), an unfamiliar or uncomfortable sleep environment, sleep apnea, and any process that disturbs sleep quality.
DIFFERENTIAL AMPLIFIERS, DIGITAL POLYSOMNOGRAPHY, SENSITIVITY, AND FILTERS
EEG, EOG, and EMG activities are recorded by differential AC amplifiers that amplify the difference in voltage between two inputs. Signals common to both inputs are not amplified (common mode rejection). This permits the recording of very small signals that are superimposed upon larger scalp-voltage changes and 60-cycle interference from nearby AC power lines. Common mode rejection depends on the impedance at input 1 and input 2, being relatively equal. A poorly conducting electrode (high impedance) will result in a large amount of 60-Hz artifact being present. By convention, in EEG recording, if input 1 is negative relative to input 2, the deflection is upward (up polarity). For each tracing, one must specify the electrode to be used at inputs 1 and 2 (also called a derivation). In bipolar recording, each amplifier records the difference between two electrodes of interest (A-B and C-D). Using selector panels, it is possible to change the electrodes recorded from a given amplifier during monitoring. In modern digital sleep monitoring, one may record the activity of numerous electrodes against a common electric reference (referential recording). Any combination of various tracings of interest can be obtained by digital subtraction (electrode A-reference) — (electrode B-reference) = electrode A — electrode B either during recording or during review (see
Table 1-3). For example,
if the sleep technologist failed to observe that EMG2 went bad during the recording, the reviewer can change the chin EMG display from EMG1-EMG2 to EMG1-EMG3. In modern digital recording, it is common to have a mixture of referential (EEG, eye electrodes, EMG electrodes), true bipolar (chest, abdominal movement, airflow), and DC (oxygen saturation) recording.
Many digital recording systems still use analog amplifiers that produce a continuous signal output. An analog-to-digital conversion board converts the signal to a digital form that can be stored and manipulated by a computer. The sampling rate must be more than twice the frequencies being recorded to avoid signal distortion. In addition, signals with a frequency higher than one-half the sampling rate must be filtered out, as they can cause aliasing distortion. The usual paper speed for sleep recording is 10 mm/s, which produces 30-second pages (30-cm wide paper). When reviewing digital recording, one can choose various time windows. A 30-second window (equivalent to 10 mm/s) is used for sleep staging. Time windows of 60 to 240 seconds may be used to view and score respiratory events. Alternatively, viewing data in 10-second window (equivalent to 30 mm/s) is the usual window for viewing clinical EEG and displaying interictal or epileptic activity. It also can be useful for measuring the frequency of a complex of oscillations or viewing the EKG. The traditional EKG speed is 25 mm/s, which is quite close to 30 mm/s. Some systems allow split screens with different time windows in each. A summary view is often provided with all-night condensed graphs of the hypnogram, Sao2 tracing, continuous positive airway pressure (CPAP) levels, respiratory events, and body position. This allows a useful overview of the entire recording. One can usually click on a given area of the summary and be taken to that point in the tracings.
In paper monitoring of sleep, the EEG is usually recorded at a sensitivity of 50 µV/cm in adults. In children, a lower sensitivity (100 µV/cm) is used because of the very high-amplitude EEG activity. Digital recording often uses 100 µV per channel width. For simplicity, many systems amplify signals at a set gain before they are digitally recorded. The signals can be amplified or diminished by changing the digital gain to produce a satisfactory display without changing the actual recorded voltage. One
can set default gains and filters so that a minimal amount of manipulation is needed to obtain a satisfactory display view of the signals.
Any signal of interest can be contaminated by unwanted low- or high-frequency signals of 50 to 60 Hz (from nearby AC power lines). Filters allow these components to be diminished. For example, a low filter (high-pass filter) attenuates the amplitude of low-frequency signals. A high filter (lowpass filter) attenuates the amplitude of high-frequency signals. A range of possible low-filter settings (off, 0.01, 0.03, 0.1, 0.3, 1, 3, 10, 30) is provided with each designation, meaning that at a setting of X, the amplitude of a signal at X Hz will be attenuated by a set amount (usually 30% or 50%) depending on the amplifier manufacturer. Lower frequencies will be attenuated even more. It is important to realize that frequencies slightly above the low-filter setting X also will be attenuated, although to a much lesser degree. Sometimes the strength of filters is given in decibels, which is defined as 20 log (voltage-out/voltage-in), where voltage-out and voltage-in are the amplitude of the signal entering and leaving the filter, respectively. A signal reduction of 30% and 50% (voltage-out/voltagein ratios of 0.7 and 0.5, respectively) correspond to -3 and -6 db reductions. Another terminology used for filters setting uses “1/2 amplitude.” A low filter with a 1/2 amplitude low setting of 1 Hz means that a signal with a frequency of 1 Hz will be attenuated by 50%. Similarly, a high filter with a setting of 1/2 amplitude high-filter setting of 30 Hz will attenuate a 30-Hz signal by 50%. Higher-frequency signals will be attenuated even more. A range of high-filter settings is typically provided (off, 1, 3, 15, 35, 70, 100).
Most amplifiers also provide optional notch filers to attenuate a narrow range of frequency (i.e., 50—60 Hz). Some recommend that notch filters not be used routinely, as the sudden appearance of increased 60-Hz activity is a clue that one or more electrodes may have gone bad. Traditional electronic filters use resistance—capacitance circuits (RC filters). Standard filter settings for different variables monitored during sleep studies are shown in
Table 1-4. Many digital polysomnography units actually record the signal over a wide frequency range (e.g., DC to 100 Hz). Although signals are acquired over a wide frequency range, they are viewed after application of desired digital low and high filters. These alter the display, but not the recorded data. This allows multiple choices of filters, if desired by the technologist or reviewer.
INTRODUCTION TO ELECTROENCEPHALOGRAPHIC TERMINOLOGY AND MONITORING
EEG activity is characterized by the frequency in cycles per second or hertz (Hz), amplitude (voltage), and the direction of major deflection (polarity). The classically described frequency ranges are delta (<4 Hz), theta (4—7 Hz), alpha (8-13Hz), and beta (>13Hz). Alpha waves (8-13Hz) are commonly noted when the patient is in an awake, but relaxed, state with the eyes closed (
Fig. 1-2). They are best recorded over the occiput and are attenuated when the eyes are open. Bursts of alpha waves also are seen during brief awakenings from sleep—called arousals. Alpha activity can also be seen during REM sleep. Alpha activity is prominent during drowsy eyes-closed wakefulness. This activity decreases with the onset of stage N1 sleep. Near the transition from stage N1 to stage N2 sleep, vertex
sharp waves—high-amplitude negative waves (upward deflection on EEG tracings) with a short duration—occur. They are more prominent in central than in occipital EEG tracings. A sharp wave is defined as deflection of 70 to 200 milliseconds in duration.
Sleep spindles are oscillations of 12 to 14 Hz with a duration of 0.5 to 1.5 seconds. They are characteristic of stage N2 sleep. They may persist into stage N3 but usually do not occur in stage REM. The K complex is a high-amplitude, biphasic wave of at least 0.5-second duration. As classically defined, a K complex consists of an initial sharp, negative voltage (by convention an upward deflection) followed by a positive-deflection (down) slow wave. Spindles frequently are superimposed on K complexes.
Sharp waves differ from K complexes in that they are narrower, not biphasic, and usually of lower amplitude.
As sleep deepens, slow (delta) waves appear. These are high-amplitude, broad waves. In contrast to the EEG definition of delta activity as <4 Hz, delta slow-wave activity is defined for sleep staging purposes as waves slower than 2 Hz (longer than 0.5-second duration) with a peak-to-peak amplitude of >75µV. The amount of slow-wave activity
as measured in the central EEG derivations is used to determine if stage N3 is present (
1) (see below). Because a K complex resembles slow-wave activity, differentiating the two is sometimes difficult. However, by definition, a K complex should stand out (be distinct) from the lower-amplitude, background EEG activity. Therefore, a continuous series of high-voltage slow waves would not be considered to be a series of K complexes.
Sawtooth waves (
Fig. 1-2) are notched-jagged waves of frequency in the theta range (3-7 Hz) that may be present during REM sleep. Although they are not part of the criteria for scoring REM sleep, their presence is a clue that REM sleep is present.
Electroencephalographic Monitoring Techniques
The traditional Rechtschaffen and Kales (R&K) guidelines for human sleep staging were based on central EEG monitoring (
1). However, most sleep recording today also includes occipital electrodes. Alpha activity is more prominent in occipital tracings. The terminology for the electrodes adheres to the International 10 to 20 nomenclature. In this nomenclature, electrodes are placed at 10% or 20% of the distance between structural landmarks on the head. Even subscripts refer to electrodes on the right and odd to electrodes on the left side of the head. The positions of the right and left central electrodes (C4 and C3), occipital electrodes (O2 and O1), and mastoid electrodes (A2 and Al) are shown in
Figure 1-5. The usual derivations use the central or occipital electrodes referenced to the opposite mastoid electrode (C4-A1, O1-A2). The greater distance between electrodes increases the voltage difference. A minimum of one central EEG derivation must be recorded for sleep staging. In modern digital recording, typically all of the electrodes (C4, C3, O2, O1, A1, A2) are recorded. Of note, additional electrodes may be added if one suspects seizure activity. This will be discussed in detail in later chapters.
EYE MOVEMENT RECORDING
The main purpose of recording eye movements is to identify REM sleep. EOG (eye movement) electrodes typically are placed at the outer corners of the eyes—at the right outer canthus (ROC) and the left outer canthus (LOC). In a common approach, two eye channels are recorded and the eye electrodes are referenced to the opposite mastoid (ROC-A1 and LOC-A2). However, some sleep centers use the same mastoid electrode as a reference (ROC-A1 and LOC-A1). To detect vertical as well as horizontal eye movements, one electrode is placed slightly above and one slightly below the eyes (
4,
5).
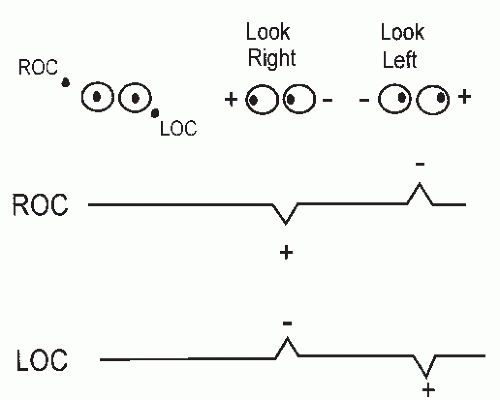
Recording of eye movements is possible because a potential difference exists across the eyeball—front positive (+) and back negative (-). Eye movements are detected by EOG recording of voltage changes. When the eyes move toward an electrode, a positive voltage is recorded (see
Fig. 1-2). By standard convention, polygraphs are calibrated so that a negative voltage causes an upward pen deflection (negative polarity up). Thus, eye movement toward an electrode results in a downward deflection (
4,
6). Note that movement of the eyes is usually conjugate, with both eyes moving toward one eye electrode and away from the other. If the eye channels are calibrated with the same polarity settings, eye movements produce
out-of-phase deflections in the two eye tracings (e.g., one up and one down).
Figure 1-2 shows the recorded results of eye movements to the right and left (assuming both amplifier channels have negative polarity up). The same approach can be used to understand the tracings resulting from vertical eye movements. Because ROC is positioned above the eyes (and LOC below), upward eye movements are toward ROC and away from LOC. Thus, upward eye movement results in a downward deflection in the ROC tracing and an upward deflection in the LOC tracing.
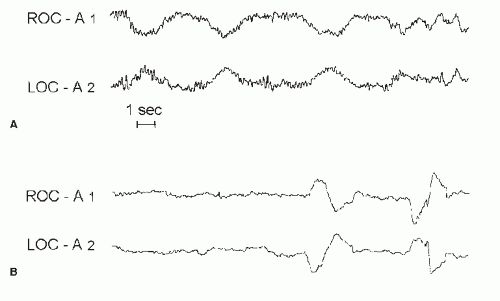
There are two common patterns of eye movements (
Fig. 1-3). Slow eye movements (SEMs), also called slow-rolling eye movements, are pendular oscillating movements that are seen in drowsy (eyes closed) wakefulness and stage N1 sleep. By stage N2 sleep, SEMs usually have disappeared. REMs are sharper (more narrow deflections), which are typical of eyes-open wake and REM sleep.
In the two-tracing method of eye movement recording, large-amplitude EEG activity or artifact reflected in the EOG tracings usually causes in-phase defections.
ELECTROMYOGRAPHIC RECORDING
Usually, three EMG leads are placed in the mental and submental areas. The voltage between two of these three is monitored (e.g., EMG1-EMG3). If either of these leads fails, the third lead can be substituted. The gain of the chin EMG is adjusted so that some activity is noted during wakefulness. The chin EMG is an essential element only for identifying stage REM sleep. In stage REM, the chin EMG is relatively reduced— the amplitude is equal to or lower than the lowest EMG amplitude in NREM sleep. If the chin EMG gain is adjusted high enough to show some activity in NREM sleep, a drop in activity is often seen on transition to REM sleep. The chin EMG may also reach the REM level long before the onset of REMS or an EEG meeting criteria for stage REM. Depending on the gain, a reduction in the chin EMG amplitude from wakefulness to sleep and often a further reduction on transition from stage N1 to N3 may be seen. However, a reduction in the chin EMG is not required for stages N2 to N3. The reduction in the EMG amplitude during REM sleep is a reflection of the generalized skeletal muscle hypotonia present in this sleep stage. Phasic brief EMG bursts still may be seen during REM sleep. The combination of REMs, a relatively reduced chin EMG, and a low-voltage mixed-frequency EEG is consistent with stage REM.