Introduction: What Is Epilepsy?
Jerome Engel Jr.
Timothy A. Pedley
Introduction
Epilepsy is one of the most common disorders of the brain.28 One of every ten people will have at least one epileptic seizure during a normal lifespan, and a third of these will develop epilepsy. Worldwide, epilepsy affects 50 million people. According to a World Health Organization (WHO) survey, epilepsy accounts for 1% of the global burden of disease, a figure equivalent to breast cancer in women and lung cancer in men.15
Epilepsy has been known since antiquity. An Assyrian-Babylonian textbook written over three millennia ago provides an accurate clinical description of the condition,12 and Indian and Chinese physicians of that time were also familiar with it. The word epilepsy is derived from the Greek verb ελαμβανειν (epilamvanein) (“to be seized,” “to be taken hold of,” or “to be attacked”). In ancient Greece, as now, people spoke of “having seized” and of having had an “attack.” This terminology derived from the very ancient notion that all diseases represented attacks by the gods or evil spirits, usually as punishment. Because seizures were the most vivid example of demonic possession, epilepsy was considered to be “the sacred disease,” and by the fifth century BC, the word had gradually acquired the specific and particular meaning associated with it today.25 Indeed, the battle between prejudice and acceptance, ignorance and knowledge, myth and science, and charlatanism and rational therapy has been long and difficult, and even today it has not yet been fully won. Even in comparison with all the advances made during the last century—more than at any other time in history—consider how enormous and fundamental was that first step attributed to Hippocrates in about 400 BC, that epilepsy is a disease of the brain that must be treated by diet and drugs, not religious incantations.9
Epilepsy is, of course, not a specific disease, or even a single syndrome, but rather a broad category of symptom complexes arising from any number of disordered brain functions that themselves may be secondary to a variety of pathologic processes. The terms convulsive disorder, seizure disorder, and cerebral seizures are used synonymously with epilepsy: They all refer to recurrent paroxysmal episodes of brain dysfunction manifested by stereotyped alterations in behavior. Modern concepts of epilepsy originate in the work of mid–19th-century physicians and scientists, the most important among them being John Hughlings Jackson.10 At a time when epilepsy denoted disorders manifested by generalized convulsions, which were believed to arise from disturbances in the medulla oblongata, Hughlings Jackson established the important concept that there were different categories of seizures, each with its own physiology and semiology. His explanation of “dreamy states” and “uncinate group of fits” as focal seizures originating from discrete areas within the cerebral cortex comes close to present-day views of limbic seizures. Similarly, his recognition of focal motor seizures (“jacksonian seizures”) not only identified the responsible locus within the brain, but also allowed him to draw inferences that have forever changed our concepts of cortical motor representation and cerebral control of voluntary movement. Hughlings Jackson, more than anyone, established a scientific approach to the study of epileptic phenomena.
Today, a large number of clinical phenomena are recognized as epileptic seizures, some of which (e.g., myoclonic and atonic seizures) are currently poorly understood and might, in fact, reflect neuronal mechanisms that are somewhat different from the pathophysiologic processes traditionally considered to be “epileptic.” A variety of conditions or epilepsies have been categorized and defined not only by the types of seizures they manifest, but also by other, associated clinical features. Specific epileptic syndromes have been identified by their characteristic seizure types, pattern of seizure recurrence, age of onset, associated neurologic and other clinical signs, electroencephalographic (EEG) findings, presence or absence of familial occurrence, and prognosis. Epilepsies and epileptic syndromes are broadly divided into idiopathic and symptomatic disorders. Idiopathic epilepsies are generally benign in the sense that they are not associated with brain lesions, neurologic abnormalities other than seizures, or mental impairment, and that they tend to be self-limited or respond readily to antiepileptic drugs. Genetic factors are important, and manifestations are typically age related. This is epilepsy sui generis (“by itself”), which conforms to the original Greek meaning of “idiopathic,” in contrast to the commonly used but incorrect meaning of “cause unknown.” Symptomatic epilepsies are those in which seizures are the consequence of an identifiable lesion or other demonstrable physical or metabolic etiology. When epilepsies are presumably symptomatic but currently of unknown specific etiology, they have been termed cryptogenic,2 a term also used in epidemiologic studies to mean unknown as to whether idiopathic or symptomatic.4 Because of its ambiguity, “cryptogenic” is a term that should be replaced by the more accurate “probably symptomatic.”5
The Role of Research
Advances in the understanding and treatment of epilepsy have occurred because of active and continuing research efforts. Indeed, it is not an exaggeration to say that many of the exciting developments in basic neuroscience in the middle and latter parts of the last century were related to epilepsy, either directly (e.g., in cellular studies of disease mechanisms) or indirectly (e.g., in investigations of cortical excitability and its control). Clinical investigation is an essential part of practice, and clinicians have played important roles in developing hypotheses that can be subjected to experimental investigation.
An important change that has occurred and accelerated in the last two decades has been the growing ability to carry out basic studies in humans. For example, intracranial monitoring
techniques used to evaluate patients with intractable seizures for surgery, and the removal of brain tissue during surgical procedures now offer investigators opportunities to investigate basic physiologic, biochemical, and molecular phenomena in patients that could previously be studied only in experimental animal models of epilepsy. Similarly, modern brain imaging methods, such as functional magnetic resonance imaging (fMRI), magnetic resonance spectroscopy (MRS), positron emission tomography (PET), and single-photon emission computed tomography (SPECT), allow noninvasive study of basic biologic questions in the living, intact brain. New insights derived from these studies make it possible to determine which abnormalities found in animal models of epilepsy have counterparts in humans, which experimental observations are valid for the human condition and which are not, and which experimental data fit within reasonable conceptual frameworks for developing further hypotheses that can be tested either in humans directly or in relevant animal models.
techniques used to evaluate patients with intractable seizures for surgery, and the removal of brain tissue during surgical procedures now offer investigators opportunities to investigate basic physiologic, biochemical, and molecular phenomena in patients that could previously be studied only in experimental animal models of epilepsy. Similarly, modern brain imaging methods, such as functional magnetic resonance imaging (fMRI), magnetic resonance spectroscopy (MRS), positron emission tomography (PET), and single-photon emission computed tomography (SPECT), allow noninvasive study of basic biologic questions in the living, intact brain. New insights derived from these studies make it possible to determine which abnormalities found in animal models of epilepsy have counterparts in humans, which experimental observations are valid for the human condition and which are not, and which experimental data fit within reasonable conceptual frameworks for developing further hypotheses that can be tested either in humans directly or in relevant animal models.
Epilepsy Is More Than Seizures
There have been many attempts to obtain a consensus on definitions of epileptic seizure and epilepsy. Recently, the International League against Epilepsy (ILAE) has proposed new definitions for both.7 In this proposal, an epileptic seizure is defined as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain.” This definition acknowledges that previous concepts of decreased inhibition and increased excitation were oversimplifications, because inhibition is actually increased in some forms of epilepsy where phasic inhibition is a central element in the primary epileptogenic abnormality. An epileptic seizure can also be a natural response of the normal brain to transient disturbance in function and, therefore, not necessarily an indication of an epileptic disorder. Such seizures are often referred to as provoked, acute symptomatic, or reactive. This accounts for a greater incidence of seizures (about 7% by age 80) than epilepsy (nearly 3%).
Epilepsy is a group of neurologic conditions, the fundamental characteristics of which are recurrent, usually unprovoked, epileptic seizures. A common operational definition of epilepsy is two or more unprovoked seizures occurring more than 24 hours apart.4 However, the new ILAE proposal7 offers a more fundamental definition of epilepsy: “A chronic condition of the brain characterized by an enduring propensity to generate epileptic seizures, and by the neurobiological, cognitive, psychological, and social consequences of this condition.” This definition emphasizes the existence of a persistent intrinsic epileptogenic abnormality that is a property of the brain itself and thus present even when seizures are not occurring. This contrasts with seizures that are dependent upon acute insults or other conditions that transiently affect an otherwise normal brain. An intrinsic epileptogenic abnormality of the brain necessary for a diagnosis of epilepsy, however, can resolve spontaneously, as in some age-related idiopathic epilepsies that typically remit.
The new ILAE definition also acknowledges importantly the psychological and social consequences of epilepsy. This change recognizes that to the affected patient, epilepsy is more than seizures, and that the condition in its entirety comprises many facets, different for each individual, that contribute to disability and impaired quality of life (Fig. 1). Treatment that focuses solely on seizures often does little to lessen disability. This is most dramatically illustrated by the patient who, having undergone successful surgical resection of epileptogenic brain tissue, becomes seizure free but remains socially isolated and unemployed, with little evidence of an improved life. Therapeutic intervention can be optimal only when the multiple medical, psychological, and environmental factors that constitute epilepsy are addressed. Thus, the physician’s role is properly defined, and sometimes circumscribed, by asking a series of questions: “What are the problems that are contributing to the patient’s predicament?” “Which of these can or need to be treated?” “What will be the consequences of treatment?” and “What outcome measures will appropriately gauge the treatment’s success?”
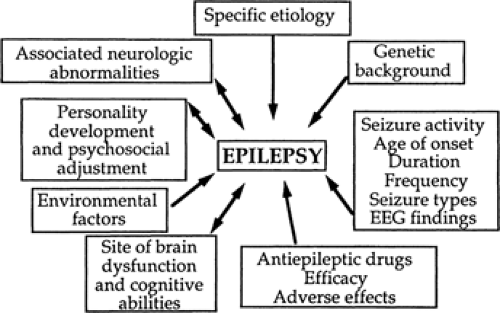 FIGURE 1. The multiple, interacting factors that contribute to the totality of epilepsy for an individual patient. |
The existing ILAE Classification of Epilepsies and Epileptic Syndromes2 and Classification of Epileptic Seizures3 are presently under review. An ILAE Task Force on Classification and Terminology has proposed a diagnostic scheme for use when describing individual patients5 (Table 1). Axis 1 consists of a detailed phenomenologic description of the ictal events, which is useful in certain situations, such as a presurgical evaluation, but otherwise can be abbreviated or omitted. Axis 2 is a new concept, recognizing seizure types as diagnostic entities based on distinct pathophysiologic and anatomic features that provide information useful for determining etiology, therapy, and prognosis. Diagnosis of a specific seizure type is especially important when diagnosis of an epilepsy syndrome is not possible. Axis 3 consists of accepted epilepsy syndromes and recognizes that a syndromic diagnosis is not always possible. An epilepsy syndrome as used here refers to “a complex of signs and symptoms that define a unique epileptic condition. This must involve more than just a seizure type: Thus, frontal lobe seizures per se, for instance, do not constitute a syndrome.” In contrast, an epileptic disease is defined as “a pathologic condition with a single, specific, well-defined etiology. Thus, progressive myoclonus epilepsy is a syndrome, but Unverricht-Lundberg myoclonic epilepsy is a disease.” Axis 4 is etiology, which includes a wide variety of genetic and nongenetic diseases associated with epilepsy, specific epilepsy genes, and acquired cerebral injuries such as trauma and infection. Axis 5, which assesses the degree of disability caused by the epilepsy, is taken from a WHO classification of impairment for neurologic disorders and is optional.
Physiologic Considerations
It is readily apparent from observing the diverse ictal phenomenology of patients with epilepsy that most seizures consist of evolving processes that depend on multiple pathophysiologic mechanisms and anatomic substrates. Two essential epileptogenic factors represent the net effect of many complex interrelated events. The first is an abnormality of cellular excitability that arises from mechanisms that affect membrane
depolarization and repolarization. The second is a “network defect” that derives from mechanisms underlying the development of aberrant neuronal integration, resulting in abnormal synchronization of neuronal populations and propagation of the epileptic discharge within neural pathways. Both sets of disturbances must be present before a seizure can occur.
depolarization and repolarization. The second is a “network defect” that derives from mechanisms underlying the development of aberrant neuronal integration, resulting in abnormal synchronization of neuronal populations and propagation of the epileptic discharge within neural pathways. Both sets of disturbances must be present before a seizure can occur.
Table 1 Proposed Diagnostic Scheme for People with Epileptic Seizures, and with Epilepsy | |||
|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





