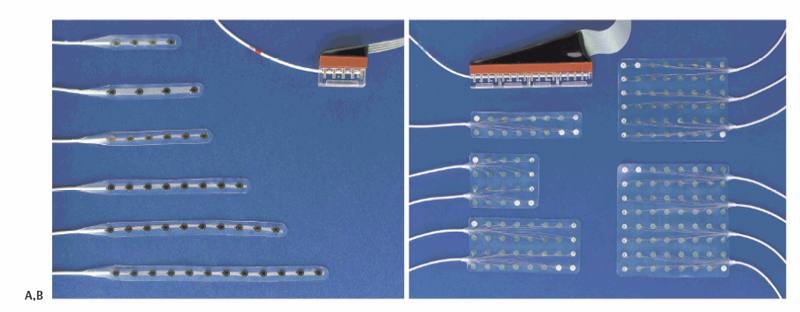
2 Invasive EEG Studies: Peg, Strip, and Grid Implantation Epilepsy is a very common neurological disorder with a prevalence of 5 to 10 per 1000 in the population in North America.1, 2 About 20 to 30% of patients are not adequately controlled by medical treatment alone.3,4 At least 12% of patients are candidates for surgical treatment, although this number may be larger with the development of new imaging and diagnostic technologies.5 A randomized, controlled trial demonstrated that surgery is superior to medical therapy.6 The goal of surgery is to remove the portion of brain that is responsible for the generation of seizure activity, a region known as the epileptogenic zone. Prior to consideration for surgery, patients require a comprehensive evaluation. The purpose of presurgical evaluation of epilepsy patients is to localize the epileptogenic zone responsible for the patient’s intractable seizures and determine if it is amenable to resection. Surgical treatment of epilepsy requires the precise location of the seizure focus to maximize the potential for surgical cure and minimize disruption of normal cortical function. The most common cause for failure in the surgical treatment of intractable epilepsy is incomplete surgical resection of the epileptogenic zone.7 Initial methods for localization of the epileptogenic zone involve noninvasive techniques such as external scalp electroencephalogram (EEG) monitoring, magnetoencephalography (MEG), interictal or ictal single-photon emission tomography (SPECT), positron emission tomography (PET), and various other neuroimaging techniques such as magnetic resonance imaging (MRI). Although helpful, these methods do not always provide sufficient information to guide resection. Some criteria used by the surgeon to consider the use of invasive techniques instead of relying on noninvasive technologies are lack of lateralization or localization of the epileptogenic zone, discordant information on noninvasive studies, presence of the epileptogenic zone near eloquent cortex, and the need to define the relationship of the zone to a lesion present on neuroimaging.8 When noninvasive techniques are insufficient, there are several options for detection of the epileptogenic zone using invasive methods, or electrocorticography (ECoG), including epidural electrodes, subdural grids, strip electrodes, and depth electrodes. Unlike scalp EEG that has a significant amount of tissue between the recorded cells and the electrode, electrodes placed by invasive methods localize the electrode on or near the cell that is being recorded. This results in less attenuation of the signal. The amplitude of the potentials recorded from the cortex is typically 2 to 58 times greater than scalp recordings.9 Additionally, invasive monitoring can be used for intraoperative recordings only. Indications for intra-operative mapping include mapping of eloquent cortex such as motor or speech. Also, intra-operative monitoring is used in tailored resections of the epileptogenic zone, localizing epileptic spikes. The first reported case of intracranial EEG monitoring to guide surgical resection was performed by Wilder Penfield and Herbert Jasper at the Montreal Neurological Institute in 1939.10,11 The patient had recurrent refractory seizure activity since a head injury in 1937. Scalp EEG performed on the patient demonstrated bilateral temporal epileptiform discharges. The patient underwent invasive EEG monitoring in an attempt to lateralize the focus. Epidural electrodes were placed via bur holes bilaterally, and the patient was monitored for 3 days revealing abnormal activity on the left side. The patient was taken to the operating room where an awake left temporal craniotomy reveled a posterior temporal meningocerebral scar that was then resected. There are several types of surface electrodes that differ in their location in the cranial space, as well as their configuration. The choice of invasive monitoring depends on patient characteristics including the site of disease, the age of the patient, and results of preoperative testing. Peg electrodes are mushroom-shaped electrodes consisting of a steel or platinum disk with a Silastic cover. These electrodes are normally placed via twist drill into the epidural space. The main clinical indication for peg electrodes is lateralization of seizure focus. These electrodes are used in patients for which scalp EEG is not possible because of anatomical reasons (e.g., bone defects) or in patients in which scalp EEG failed to lateralize the seizure activity.12,13 Peg electrodes do not record directly on the cortical surface; therefore, they have limited ability to spatially definethe epileptogenic zone. Also, because of their shape and configuration, they cannot be used to monitor subfrontal or subtemporal regions. However, modified peg electrodes with cylindrical forms have been used successfully in these regions.14 Because the dura is left intact, these electrodes are believed to have a reduced rate of complications such as hematoma and infection. Strip electrodes consist of a linear array of platinum or stainless steel contacts embedded into a silicon strip (Fig. 2.1A). These constructs normally consist of four to eight contacts spaced 10 mm apart. These electrodes are placed into the subdural space either through a bur hole or under the edge of a bone flap. This type of electrode is used both for intraoperative monitoring during tumor resections and for postoperative monitoring in seizure cases. These electrodes have some advantage over larger grid electrodes. Because of their narrow size they can be passed under bone edges considerable distances to monitor more distance sites. For example, this type of electrode is often passed around the temporal lobe to monitor mesial temporal structures. Subdural grids consist of a square array of contacts embedded in silicon (Fig. 2.1B). These constructs normally consist of four to 64 contacts; however, custom-designed grid patterns are available. These grids are placed on the cortical surface after a large craniotomy. An additional advantage to strip and grid electrodes is that these electrodes, unlike peg or other epidural electrodes, can be used for stimulation studies. Strip electrodes are used over the cortical surface for recordings. These electrodes are passed in the subdural space through a bur hole or under the edge of a craniotomy. A Penfield dissector is used to create room to pass the strip in the subdural space and to direct the strip in the appropriate direction. Constant irrigation is used to reduce any friction as the strip is passed and to monitor for any subdural bleeding. Due to the risk of damaging cortical veins, extreme care must be taken if they are passed into the interhemispheric fissure, near large cortical veins such as the vein of Labbé, or near venous sinuses. Placement of strip electrodes can be aided by frameless stereotaxy. Strip electrode placement is often used in suspected cases of temporal lobe epilepsy (TLE). The electrodes are placed in such a fashion as to cover the temporal lobe.15,16 In standard placement, a temporal bur hole is placed 2 cm anterior to tragus and superior to zygoma. Through this bur hole, two four-contact strip electrodes are passed and directed medially toward the parahippocampus and posterior to middle and inferior temporal gyrus. Next, through a frontal bur hole 4 cm anterior to the coronal suture and 2 cm lateral to midline, two electrodes are passed. A four-contact strip is passed along the interhemispheric fissure to cover the cingulate gyrus and one eight-contact strip is passed toward the ipsilateral globe. An alternative to the classic method is placement of an anteromedial strip electrode. This strip is passed around the temporal pole and underneath the lesser wing of the sphenoid electrode to monitor the medial temporal lobe.17 The end of the electrode is then passed through the dural defect and bur hole, and tunneled under the skin with a trocar. A nylon purse-string suture is placed around electrode, and a drain stitch is applied to secure the electrode. Each electrode has a unique color combination, and this color should be recorded along with the location of the electrode. Subdural grids are placed over the lesion or region of interest with care taken to overlap any eloquent cortex that is near. The placement of electrodes is affected by preoperative noninvasive studies. In patients with a suspected lesion present on preoperative imaging, grid placement is straightforward and can be aided by identification of the lesion with neuronavigation. In nonlesional cases, the electrodes are placed over the suspected epileptogenic focus based on scalp EEG recordings, MEG, ictal SPECT studies, or by semiology. Often a larger grid is used for nonlesional cases in an attempt to map the entire area.
History
Electrode Types
Operative Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








