Front Neurol Neurosci. Basel, Karger, 2014, vol 33, pp 19-29 (DOI: 10.1159/000351889)
______________________
Transient Ischemic Attack as a Medical Emergency
Yasushi Okada
Department of Cerebrovascular Medicine and Neurology and Clinical Research Institute, National Hospital Organization Kyushu Medical Center, Fukuoka, Japan
______________________
Abstract
Since transient ischemic attack (TIA) is regarded as a medical emergency with high risk for early stroke recurrence, the underlying mechanisms should be immediately clarified to conclude a definitive diagnosis and provide early treatment. Early risk stratification using ABCD2 scores can predict the risk of ischemic stroke occurring after TIA. Carotid ultrasonography (US) can evaluate the degree of stenosis, plaque properties and flow velocity of ICA lesions. High-risk mobile plaques can be classified by carotid US, and aortogenic sources of emboli can be detected by transesophageal echocardiography. Cardiac monitoring and blood findings are thought to play a key role in a diagnosis of cardioembolic TIA. Diffusion-weighted imaging (DWI)-MRI and MR angiography are also indispensable to understand the mechanism of TIA and cerebral circulation. To prevent subsequent stroke arising from TIA, antiplatelet and anticoagulant therapies should be started immediately along with comprehensive management of life-style, hypertension, diabetes mellitus, dyslipidemia and other atherosclerotic diseases. Carotid endarterectomy and endovascular intervention are critical for treating symptomatic patients with significant stenosis of ICA. A novel concept of acute cerebrovascular syndrome (ACVS) has recently been advocated to increase awareness of TIA among citizens, patients and medical professionals. TIA should be recognized as the last opportunity to avoid irreversible ischemic stroke and its sequelae. The clinical relevance of the new concept of ACVS is advocated by early recurrence after TIA, analysis of high-risk TIA, treatment strategies and the optimal management of TIA. Raising TIA awareness should also proceed across many population sectors.
Copyright © 2014 S. Karger AG, Basel
Urgency: Short-Term Risk of Transient Ischemic Attack
Patients with transient ischemic attacks (TIAs) are at high risk of early stroke. Large cohort and population-based studies over the past decade have demonstrated a higher risk of early stroke after TIA than had been suspected. In general, 15-20% of patients have a stroke within 3 months of a TIA [1], with half of those occurring within 48 h [2]. Several recent guidelines recommend that patients with TIA should be thoroughly assessed within 24 h. In a prospective, population-based observation with complete follow-up (Oxford Vascular Study) of 1,247 patients with a first TIA or stroke, 35 had recurrent stroke in the same arterial territory within 24 h. The 6-, 12-, and 24-hour stroke risks after 488 first TIAs are 1.2, 2.1 and 5.1%, respectively, and 42% of all recurrent strokes during the 30 days after a first TIA occur within the first 24 h [3]. The 12- and 24-hour risk area is closely associated with ABCD2 scores. Recurrent strokes within the first 24 h of a TIA highlight the need for emergency assessment. The ABCD2 score is a reliable clinical indicator during the acute phase to assess appropriate triage, emergency management and feasible treatment. However, most patients with TIA do not receive optimal treatment even today; statins are not administered, and blood pressure is not controlled. Many patients are prescribed with aspirin and sent home directly from an emergency room without additional evaluation. Yet risk is particularly high during the first few days after TIA. Studies in northern California (USA) and Oxfordshire (UK) found an approximate 4% risk of stroke within the first 24 h of a TIA, which is about twice the risk of myocardial infarction or death in patients presenting with acute coronary syndrome (about 2% at 24 h). The northern California study followed up 1,707 patients for 3 months after a first visit to an emergency room where they were diagnosed with TIA. The results showed an unexpectedly high (10.5%) overall incidence of stroke during the 3-month period, and half of these developed within 48 h after the onset of TIA [4]. Recurrent ischemic stroke occurred in 8 (5%) of 160 consecutive patients with DWI-negative TIA during hospitalization at Kyushu Medical Center [5]. All of these occurred within 7 days with a median of 2.5 days. Unlike the German Stroke Bank study [6], a lacunar etiology was the most frequent, and modified Rankin Scale outcomes were mostly good at discharge (fig. 1a). The incidence of recurrent stroke closely correlates with ABCD2 score. The prevalence of both atrial fibrillation (AF) and occlusive arterial disease is also significantly higher in patients with, than without recurrent stroke. An atherothrombotic etiology is more likely in the unclassified type (AF and/or middle cerebral artery), since PT-INR in these types remains within the optimal range (fig. 1b). These results are particularly characteristic in Japan, compared with USA-European findings. Even under immediate best medical management, patients with high ABCD2 scores tended to develop recurrent stroke. A combination of AF and occlusive arterial disease might indicate high risk for early recurrence of ischemic stroke in patients with TIA.
Effect of Emergency Care
The EXPRESS (Early use of EXisting PREventive Strategies for Stroke) study [7] in Oxford (UK) was designed to compare the outcomes of treatment before and after switching to emergency care in which each patient is evaluated more actively and urgently at a TIA clinic and treatment with proven methods is started within 24 h when possible. The findings showed that early treatment positively affected socioeconomic outcomes, length of hospital stay and reduced the incidence of ischemic stroke and improved activities of daily living (ADL) at 90 days [7, 8]. Although these were observational studies and the influence from confounding factors could not be ruled out, the stroke risk after onset of TIA or minor ischemic stroke decreased by 80% compared with risk recorded before starting emergency care. Lavallée et al. [9] also evaluated the effects of rapidly assessing patients with TIA at a TIA clinic on clinical decision-making, the length of hospital stay and subsequent stroke rates. Patients were assessed within 4 h of admission by means that included neurological, arterial and cardiac imaging. Among 1,085 patients admitted with suspected TIA, 574 (53%) attended the TIA clinic within 24 h of symptom onset, 701 (65%) had confirmed TIA or minor stroke, and 144 (13%) had possible TIA. Of the patients with confirmed or possible TIA, all started a stroke prevention program, 43 (5%) had urgent carotid revascularization, and 44 (5%) were treated for AF with anticoagulants. After assessment, 808 (74%) of the patients seen were sent home on the same day. The 90-day stroke rate was 1.24% (95% CI: 0.72-2.12), whereas the rate predicted from ABCD2 scores was 5.96%. This 80% stroke reduction was exactly the same as the EXPRESS results, that is, risk predicted based on ABCD2 scores. Use of TIA clinics with 24-hour access and the immediate initiation of preventive treatment might greatly reduce length of hospital stay and risk of stroke compared with predicted risk. Thus, this type of emergency TIA clinic is very effective in preventing stroke. The results of the EXPRESS and SOS-TIA registry referred to the 2009 Japanese Guidelines for the Management of Stroke [10], which state, ‘If TIA is suspected, the onset mechanism should be identified as soon as possible, and treatment to prevent subsequent cerebral infarction must be started immediately (Grade A)’. Since the early intensive management of TIA is rather important and awareness of TIA as a medical emergency needs to be heightened, a new concept of acute cerebrovascular syndrome (ACVS) that requires emergency examinations and treatment has been advocated along the lines of acute coronary syndrome [11] (fig. 2).
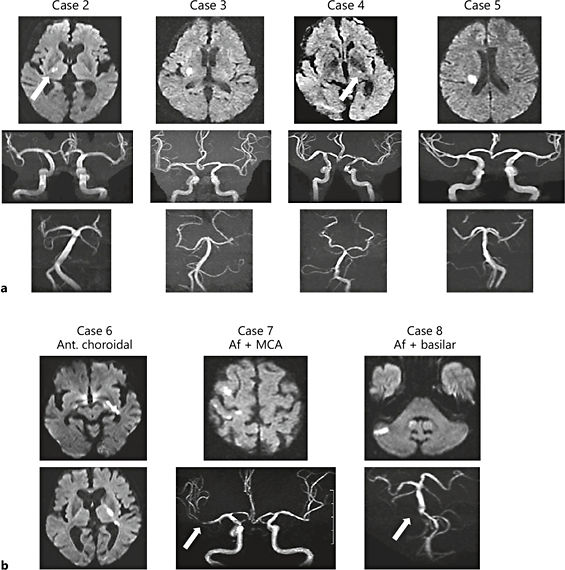
Fig. 1. Recurrent brain infarction in patients with DWI-negative TIA of unclassified and lacunar etiology. Four patients with lacunar TIA (a) and 3 with unclassified TIA accompanied by AF and intracranial artery disease (b). Modified from Mori et al. [27].
Fig. 2. Treatment on same spectrum as acute ischemic attack. Awareness of TIA as ACVS that requires emergency examination and treatment, like acute coronary syndrome.
Acute cardioembolic brain infarction without prior TIA is not rare, and often results in severe and irreversible neurological deficits that are referred to as devastating or knockout brain infarction, implying a bedridden state brought about by one straight punch delivered by a cardiac embolus. About 1.6-20% of patients with cardioembolic stroke reportedly experience recurrent stroke in another vascular territory within 2 weeks [12, 13]. Therefore, if AF is detected in patients with TIA in the acute setting, anticoagulant therapy should be started as soon as possible because prior TIA is a red flag indicating a last chance to avoid severe neurological impairment.
Carotid artery stenosis is responsible for crescendo TIA and stroke. In practice, the North American Symptomatic Carotid Endarterectomy Trial (NASCET) found an 8.9 and 20.1% incidence of ipsilateral stroke during 7 and 90 days, respectively, after TIA onset in patients with carotid artery severe stenosis [14]. Bond et al. [15] reported that the prognosis of patients with TIA accompanied by carotid stenosis differs greatly depending on whether or not treatment is provided within 2 weeks of disease onset. However, the reality is that carotid endarterectomy (CEA) and stenting often proceed several weeks after onset.
Key Points of Risk Stratification at First Visit
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








