28 | Klippel-Feil Syndrome |
 | Case Presentation |
History and Physical Examination
A 14-year-old girl with an unremarkable past medical history presented 4 years after a fall from a trampoline. Her main symptom after her fall was persistent axial neck pain. However, her symptoms gradually progressed to weakness and atrophy of the proximal musculature of her left arm. Additionally, 3 months before her presentation, she was struck in the back of the neck by a softball. After the impact, she fell to the ground and noted difficulty with movement in her left upper extremity. Over the next few weeks, she had progressive exacerbation of her neck pain and new onset of numbness and tingling in both of her hands.
On physical examination, the patient appeared to be a developmentally normal young female. She was noted to have very limited range of motion of her neck, especially in rotation. Her musculature appeared normal with the exception of profound atrophy of her left deltoid muscle. Her neurological examination showed no cranial nerve deficits. On motor examination, her right arm and bilateral lower extremities were normal strength. Her left arm was noted to have weakness in deltoid (1/5), biceps (4/5), brachioradialis (4/5), triceps (4/5), grip (4/5), and hand intrinsics (4/5). Sensation was intact to light touch and pinprick throughout. Reflexes were normal and her toes were downgoing. She walked with a normal gait.
Radiological Findings
Radiographic abnormalities were noted, including (1) assimilation of the atlas to the occiput, (2) absence of posterior elements at C2 and abnormal (incomplete) posterior elements from C3 through C6, (3) congenital fusion between the vertebral bodies of C5 and C6, and (4) retrolisthesis of C3 on C2 and C4 in flexion (Fig. 28–1). Sagittal T2 magnetic resonance imaging (MRI) showed retrolisthesis of C3 with a kyphotic deformity and the spinal cord draped over this floating vertebral body (Fig. 28–2).
Diagnosis
Klippel-Feil syndrome
 | Background |
Klippel-Feil syndrome, first described by the French physicians Maurice Klippel and Andre Feil,1 originally characterized the triad of shortened neck, low posterior hairline, and neck hypomobility. The diagnosis of Klippel-Feil syndrome has since evolved to incorporate a congenital fusion of any two or more cervical vertebrae because the classic triad appears in less than 50% of patients with such congenital fusions.2 Klippel-Feil syndrome has an incidence of ~1 in 42,000,2,3 with a reported 3:2 female predominance.2,4–10
Klippel-Feil syndrome patients can exhibit many other clinical abnormalities that accompany their cervical deformity due to the congenital nature of this disorder. These additional abnormalities can be more clinically relevant to patients’ outcomes.2 This chapter describes the established classifications of Klippel-Feil mutations and addresses the associated abnormalities that should be sought and diagnosed, as well as the ultimate recommendations for the management of the cervical deformity that defines the Klippel-Feil syndrome.
 | Classification |
Numerous attempts have been made to classify or categorize the congenital cervical fusions in Klippel-Feil patients. Feil, in a 1919 follow-up paper to the original 1912 work,11 defined three categories. Type I patients have fusion of multiple cervical and sometimes upper thoracic vertebrae and are more likely to present with the classic triad of symptoms (Fig. 28–3).12 Type II patients have fusions across one or two intervertebral spaces (Fig. 28–4), most commonly involving the high subaxial cervical segments (C2-3 or C3-4, depending on the series).6,8,12,13 Occipitalization of the atlas or axis or both is also seen in this, population. Type II patients are most common, with this category representing 84% of the total population in one series.14 Type III patients are least common and are defined to have the characteristics of either type I or II cervical fusions with concurrent lower thoracic or lumbar congenital fusions.
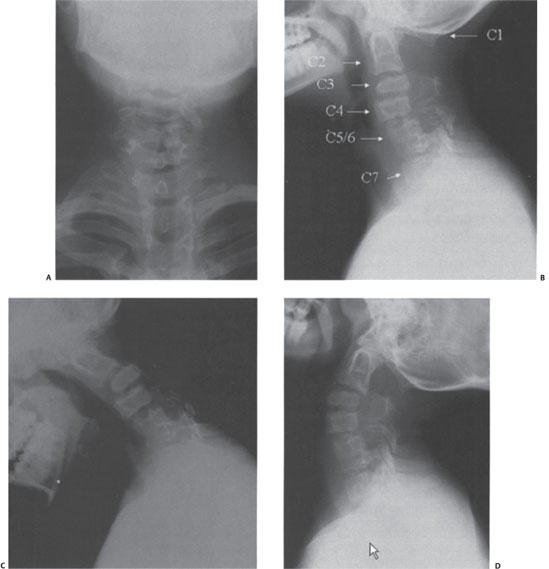
Figure 28–1 (A) Anteroposterior, (B) neutral lateral, (C) flexion, and (D) extension radiographs showed multilevel cervical anomalies and instability. Cervical levels are labeled in (B).
The large preponderance of type II patients relative to the other two categories provides more clinical data to analyze this population. David et al reported a series of 30 patients, with 37% having only subaxial cervical congenital arthrodesis, whereas 63% involved either partial or complete assimilation of the atlas to the occiput.13 In addition, coronal asymmetry is also very common and has been reported in 57 to 74% of patients, often manifesting with a hemivertebra.2,14 Despite the striking radiographic features, these patients can often be clinically asymptomatic.
An additional classification system proposed by Pizzutillo et al is based on radiographic flexion-extension range of motion of the cervical spine. The cervical spine is divided into upper (above the inferior border of C2) and lower segments (below the inferior border of C2).7 Pizzutillo’s class I patients have normal range of motion; class II patients are hypermobile in the upper segment; class III patients are hypermobile in the lower segment; and class IV patients are hypermobile in both the upper and lower segments.

Figure 28–2 T2-weighted magnetic resonance images of the cervical spine for the presented patient
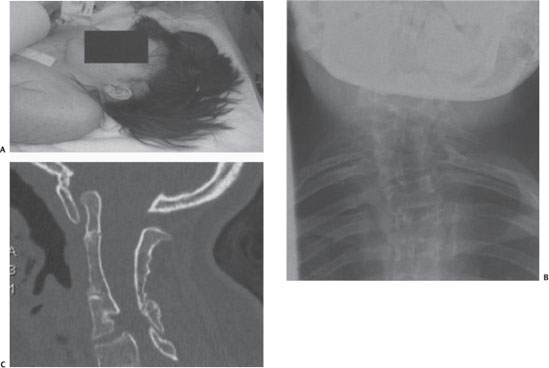
Figure 28–3 Demonstration of a Klippel-Feil class I mutation. (A) Patient was noted to have a short neck, low hairline, and very limited mobility of her cervical spine. (B) Anteroposterior plain radiograph demonstrating the short neck and segmentation anomalies. (C) Computed tomographic scan sagittal reconstruction showing congenital fusion of the cervical vertebrae from C1 to C6.
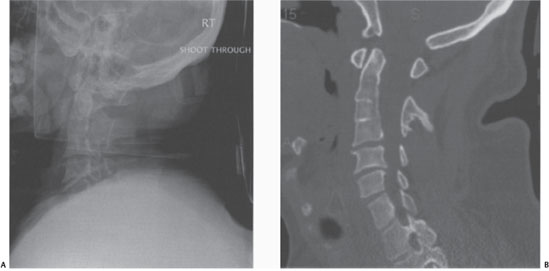
Figure 28–4 (A) Lateral cervical radiograph and (B) computed tomography demonstrating a Klippel-Feil class II anomaly.
 | Associated Abnormalities |
When fewer than three vertebrae are involved, or if only lower subaxial cervical vertebrae are involved in the congenital arthrodesis, patients may not experience any limitation of motion.3 In fact, many Klippel-Feil patients typically present for medical attention due to an associated congenital abnormality. The associated anomalies are summarized in Table 28-1.3
In particular, congenital scoliosis, which is found in over half of Klippel-Feil patients,10,15 can often be the inciting cause for workup. Other musculoskeletal deformities, in descending order of frequency, include rib abnormalities (not including the presence of cervical ribs, found in approximately one third of patients); Sprengel’s deformity (the uni- or bilateral failed descent of the scapula, found in 20 to 35%); and cervical ribs (found in 12 to 15%).3 Congenital upper limb deficiencies are also found in less than 10% of Klippel-Feil patients, ranging from hypoplasia of the thumb, hand, or distal upper extremity. These limb deficiencies are usually unilateral but may be bilateral.10,15 Craniofacial malformations and spina bifida have also been linked to Klippel-Feil syndrome.5
Other organ systems are also commonly involved. The genitourinary system has been reported to be involved in 25 to 35% of patients.15,16 Unilateral absence of a kidney is the most frequent abnormality. Double collecting systems are also seen, as are renal ectopia or malrotation, horseshoe kidneys, and hydronephrosis from uteropelvic obstruction.17 These issues can be severe enough to require renal transplantation. The index patient in Klippel and Feil’s case report died of nephritis.3 Mayer-Rokitansky-Kuster syndrome, or the congenital absence of the uterus and upper vagina, has also been associated with Klippel-Feil syndrome.18
Anomaly | Percentage of Patients |
Congenital scoliosis | >50 |
Genitourinary abnormalities | 25–35 |
Rib abnormalities* | 33 |
Deafness | 30 |
Sprenqel deformity | 20–30 |
Cardiovascular abnormalities | 4–29 |
Synkinesia | 15–20 |
Cervical ribs | 12–15 |



