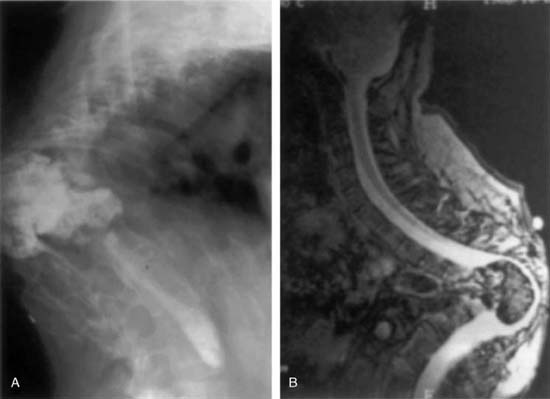
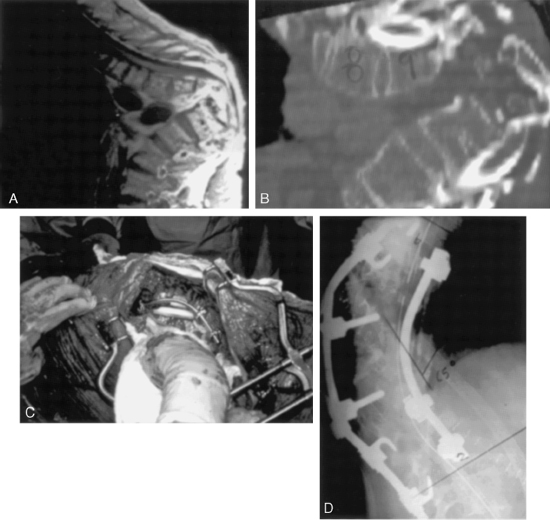
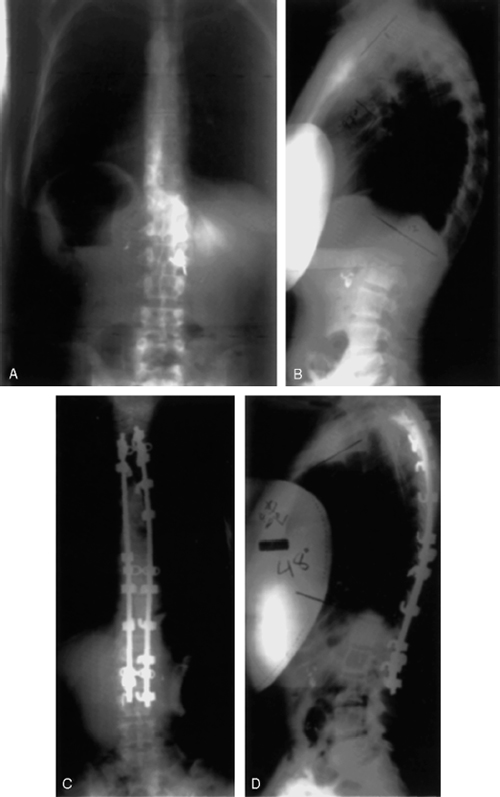
18 I. General considerations A. Anatomic variation 1. Cervical lordosis, thoracic kyphosis, and lumbosacral lordosis 2. Sagittal plumb line (odontoid) should normally cross C7–T1, T12–L1, and posterior aspect of the sacrum (S1). B. Normal thoracic kyphosis 1. Twenty to 45 degrees, mean = 34 degrees C. Normal lumbar lordosis 1. Forty to 60 degrees 2. Two thirds of lordosis occurs between L4–L5 and L5–S1. II. Biomechanics A. Anterior column failure results in compression, and posterior column fail ure results in tension. B. Posterior structures 1. Lamina and ligamentum flavum are relatively stronger in resisting tension than facets, capsules, and interspinous ligaments. C. Deformity increases moment arm, resulting in further decompensation. D. Eccentric loading can affect cartilaginous growth. 1. Compression decreases growth anteriorly. 2. Tension increases growth posteriorly, resulting in increased kyphosis. III. Classification A. Postural B. Congenital (Fig. 18-1) 1. Defect of formation 2. Defect of segmentation 3. Mixed C. Scheuermann’s disease (Fig. 18-2) D. Neuromuscular E. Myelomeningocele 1 Developmental (late paralytic) 2. Congenital (present at birth) F. Traumatic 1. Due to bone, ligament, and/or cord injury G. Postsurgical 1. Postlaminectomy 2. Following excision of a vertebral body I. Metabolic 1. Osteoporosis a. Senile b. Juvenile 2. Osteomalacia 3. Osteogenesis imperfecta J. Skeletal dysplasia 1. Achondroplasia 2. Muchopolysaccharidoses 3. Neurofibromatosis K. Collagen disease 1. Marie-Strumpell disease L. Tumor 1. Benign 2. Malignant a. Primary b. Metastatic M. Inflammatory and infectious IV. Specific kyphotic deformities A. Postural kyphosis 1. Most common in adolescents and young adults 2. Round back deformity 3. Modest kyphosis (40 to 60 degrees) 4. Smooth and flexible 5. No radiographic changes B. Congenital kyphosis 1. May be single or multilevel a. Type I (1) Failure of formation (hemivertebra) (2) Worse prognosis for progression and paraplegia (a) Upper spinal levels have a worse prognosis than lower levels. b. Type II (1) Failure of segmentation (bar) c. Type III (1) Combination of I and II 2. Treatment a. Nonoperative treatment is ineffective. b. Surgery (1) Type I lesions (a) Posterior in situ fusion if <50 degrees at 1 to 5 years (b) Anterior and posterior fusion if >50 degrees and older children (i) Better correction and maintenance (ii) Lower rate of pseudarthrosis (i) Release of all the tethering structures * Anterior longitudinal ligament ** Intervertebral disk and end plate *** Posterior longitudinal ligament (ii) Intraoperative distraction and correction of the deformity * Rib, fibula, or iliac crest strut grafts (iii) Simultaneous or second-stage posterior fusion with compression instrumentation (iv) Postoperative bracing is recommended. (2) Type II lesions (a) Posterior fusion only if less than 55 degrees of kyphosis (i) For severe deformity, an anterior osteotomy and correction and fusion may be attempted followed by a posterior fusion. (b) Skeletal traction is contraindicated as it may cause paraplegia. C. Scheuermann’s disease (juvenile kyphosis) 1. Scheuermann first described radiological manifestation of this disease in 1920. 2. Incidence is 0.4 to 8.3% of the population, but only 1% seeks medical attention. 3. Pathogenesis is unknown. a. Familial tendency with no genetic link b. Collagen weakness and stunted ossification of the vertebral end plate are characteristic. c. Osteopenia d. Nutritional deficiencies e. Mechanical alterations and muscle weakness have been theorized. (1) No scientific evidence exists. (2) Growth centers adjacent to the vertebral end plate (not ring apophyses) (a) Anterior cartilaginous columns experience stunted growth with axial loading. (b) Posterior physis hypertrophy due to tensile forces (3) With kyphotic deformity, spinal flexors become stronger than extensors because of moment arm. 4. Pathoanatomy a. Thickened and contracted anterior longitudinal ligament b. Wedging of the anterior vertebral bodies c. Nucleus pulposus (1) Protrusion anteriorly and into the bony spongiosa (Schmorl’s nodes) 5. Clinical findings a. Onset is commonly between 12 and 14 years of age. b. Equal male:female ratio c. Deformity is the most common presenting complaint. d. Pain occurs in ~50% among those who seek medical attention. (1) Increased rate of symptomatology if lumbar spine is involved (a) Some patients develop lumbar spondylolysis later. 6. Physical examination a. Increase in thoracic kyphosis (rigid) b. Compensatory lumbar and cervical lordosis (1) Round shoulders (2) Head forward c Muscle tightness and contractures are seen typically in the hamstrings. d. Thirty percent have an associated mild scoliosis. 7. Radiographic findings a. Early (1) Disordered endochondral ossification (2) Irregular end plates (3) Narrowing of the intervertebral disk space (4) Schmorl’s nodes b. Intermediate (1) Vertebral wedging (2) Increasing kyphosis greater than 45 degrees (a) More than 5 degrees of anterior wedging in three or more vertebrae at the apex of the kyphosis (Sorenson’s criteria) c. Late (1) Degenerative changes (a) Osteophytes (b) Facet hypertrophy d. Standing lateral and supine hyperextension views are used to assess rigidity of the curve 8. Treatment a. Observation is indicated for mild deformity with minimal symptoms. b. Bracing indications (1) Vertebral wedging greater than 5 degrees (2) Kyphotic curves between 45 and 65 degrees and 1 to 2 years of growth remaining (a) Milwaukee brace for apex above T9 (b) Thoracolumbar Sacral Orthosis (TLSO) for apex below T9 and thoracolumbar curves (3) Curve correction and wedging improvement of -40% can be expected after 6 to 12 months. (4) Brace should be weaned with skeletal maturity, but loss of correction is expected after 10 years. c. Exercise (1) Stressing pelvic tilt, abdominal strengthening, spinal flexibility, and thoracic spine extension exercises is an important part of the treatment plan 9. Surgery a. Indications (1) Severe deformity after growth completion with unrelenting pain (a) Typically >75 degrees and >10-degree wedging in three or more contiguous vertebral bodies (2) Resistance to bracing after 6 months (3) Neurological signs or symptoms b. Techniques (1) Posterior-only instrumented fusion (a) Curves less than 75 degrees and bending correction to less than 50 degrees (b) Posterior instrumentation should extend the entire kyphotic region, and distally it should include one lordotic vertebra (usually L1 or L2). (2) Anterior fusion (transthoracic approach) followed by posterior fusion and instrumentation (a) Curves greater than 75 degrees with minimal bending correction (>50 degrees) c. Postoperative protocol (1) TLSO for 6 to 9 months until solid fusion d. Complications (1) Pseudarthrosis and instrumentation failure (greater in posterior fusion alone) (2) Loss of correction (3) Infection (4) Pulmonary complications (5) Neurological deficits D. Neuromuscular kyphosis (Fig. 18-1) 1. Associated conditions a. Poliomyelitis b. Anterior horn cell diseases (spinal muscular atrophy) c. Cerebral palsy d. Charcot-Marie-Tooth disease e. Muscular dystrophy f. Friedreich ataxia 2. Lack of the extensor muscle strength contributes to development of a kyphotic deformity 3. Natural history is progressive even after skeletal maturity. 4. Treatment a. Bracing until the patient is ~11 to 12 years old to maximize truncal height b. Posterior fusion with instrumentation in milder and flexible curves (1) Compression instrumentation is preferred over Luque rods with sublaminar wires for correction of kyphosis. (2) Combined anterior and posterior fusion with instrumentation in severe fixed deformities E. Myelomeningocele 1. Congenital a. It is generally not recommended to correct deformity at birth because of the lack of bone stock and associated problems. 2. At 3 to 5 years of age, posterior resection followed by of correction of kyphosis a. Posterior instrumentation should be applied two to three vertebrae proximal to the apex. b. Followed by 6 to 9 months of bracing F. Developmental or paralytic kyphosis 1. The deformity is progressive, because the extensors of the spine (sacrospinalis and quadratus lumborum muscles) rotate anteriorly to increase flexion force. 2. Treatment a. Bracing is indicated for young patients with mild deformity. b. Posterior fusion involving long fusion to the sacrum c. Anterior release and fusion followed by posterior fusion with compression instrumentations G. Posttraumatic kyphosis 1. Acute or late secondary to severe compression fractures, burst fractures, or fracture-dislocations 2. More common for unstable fractures after conservative treatment 3. Symptoms include deformity, pain, and neurological deficit. 4. Treatment a. Observation and conservative treatment if the deformity causes mild pain that is controllable b. Surgery is most commonly done by a combined anterior and posterior fusion. (1) Anterior decompression with anterior instrumentation alone may be done if adequate correction has been achieved and the instrumentation is stable. (2) Posterior-only transpedicular osteotomy may be done if there is no neurological compression. H. Postsurgical kyphosis 1. Usually observed after laminectomy for spinal cord tumors and syringomyelia 2. Fusion is recommended when extensive laminectomy has been performed. 3. Severe deformity is approached with a combined anterior and posterior fusion. I. Infectious kyphosis (Fig. 18-3) 1. Infection may be caused by tuberculosis and pyogenic osteomyelitis. 2. Thoracolumbar junction is most commonly affected. 3. Treatment a. Antibiotic treatment includes long-term intravenous antibiotics and bracing. b. Anterior debridement and fusion indications (1) Unresponsive to medical treatment (2) Multiple-level involvement (3) Spinal cord compression (4) Presence of an abscess
Kyphotic Spinal Deformities in Children and Adults
Neupsy Key
Fastest Neupsy Insight Engine