Fig. 12.1
Postoperative cervical spine x-rays in the anteroposterior and lateral projections of a C5–7 LMS fixation
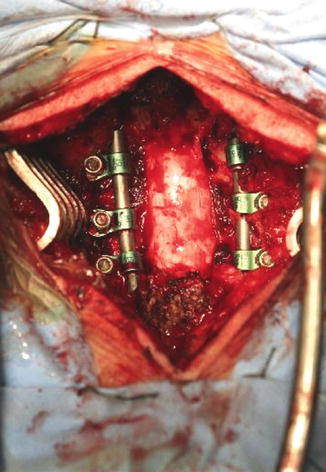
Fig. 12.2
Intraoperative photograph of a three level LMS fixation of the subaxial spine. Note the wide decompression and dural exposure with removal of all posterior elements
We will now carry on to describe the surgical technique of the main LMS fixation procedures.
Surgical Techniques
Four techniques of LMS fixation have been more diffusely described and compared.
The original Roy-Camille procedure was modified by Magerl, Anderson and An. While all four techniques are conceptually the same, involving the placement of a screw in the width of the lateral mass, they differ in the entrance point for screw insertion and in the orientation of screw trajectory.
This is due to the attempt of the various authors to find the ideal combination of maximum screw purchase and minimum risk of injury to the exiting cervical nerve root and the vertebral artery in the transverse process of the cervical vertebra.
Approach to the Posterior Cervical Spine
While the initial exposure of the posterior aspect of the cervical spine is not specific to LMS instrumentation procedures it is worth underlining some peculiar steps from skin incision to muscle dissection that will facilitate the entire procedure.
In approaches to the posterior cervical spine, especially if only a single level fixation is contemplated, it is worth it to plan the skin incision with lateral fluoroscopic control . Particular attention should be paid not only to the rostrocaudal extension of the incision but also to the orientation of the deepening of the incision as muscle dissection proceedes. This will help minimizing the extent of muscle dissection, bleeding and injury to the zygoapophyseal joint capsules not involved in the fusion. Contrarily to pedicle screw insertion techniques, LMS insertion requires a diverging screw trajectory, thus not requiring extensive muscle dissection rostrally and caudally to the instrumented levels for appropriate muscle retraction.
If instrumentation is confined to subaxial levels, attention should be paid not to dissect the rectii capitis and oblique muscles off the posterior aspect of C2 to avoid unnecessary destabilization of the craniocervical junction .
Holding to the midline after incision of the fascia and meticulous dissection of the paraspinal muscles off the spinous processes and laminae can help avoid excessive bleeding often encountered in the posterior cervical spine due to large paraspinal venous plexuses.
Finally, a clean dissection of the levels to be instrumented is mandatory to correctly identify the surgical landmarks which essentially consist in the midpoint of the lateral mass on its posterior aspect. Inferior, superior and lateral confines of the lateral mass to be instrumented should thus be clearly identified.
Once the midpoint of the lateral mass is identified, the four techniques proceed according to their specific indications.
Roy-Camille
The entry point for screw positioning is exactly in the center of the posterior surface of the lateral mass. On the sagittal plane the trajectory is obtained by aiming anteriorly with an inclination perpendicular to the posterior surface and on the axial plane by aiming laterally at 10° degrees (Fig. 12.3).
Fig. 12.3
Schematic drawing of cervical vertebrae depicting on top a view from behind. Note the entry point at the center of the dorsal aspect of the lateral mass (Ebraheim et al. [5]. Reprinted with permission)
Magerl
The entry point is 2 mm medial and 2 mm superior to the center of the posterior facet of the lateral mass. On the sagittal plane the trajectory is oriented cephalad at an angle so as to parallel the joint space and on the axial plane it goes laterally at an angle of 25–30° (Fig. 12.4). In this technique, given that the cephalad orientation on the sagittal plane parallels the facet joint, this landmark can be used in two ways to help guiding screw insertion: a thin straight dissector can be inserted into the joint space between two levels that need to be instrumented, thus guiding orientation, or lateral fluoroscopy can be used to plan the trajectoy, paralleling the cephalad and caudad facet joints.
Fig. 12.4
Schematic drawing of the Magerl technique. Note that the entry point is slightly medial and cranial with respect to the center point (Ebraheim et al. [5]. Reprinted with permission)
An
The entry point is two mm medial to the midpoint of the lateral mass at the same height. On the sagittal plane the trajectory is oriented 15° cephalad and on the axial plane 30° laterally (Fig. 12.5).
Fig. 12.5
Schematic drawing of the An technique. The entry point is slightly medial and at the same level of the center point (Xu et al. [8]. Reprinted with permission)
Anderson
The entry point is again two mm medial to the midpoint of the lateral mass at the same height. On the sagittal plane the trajectory is oriented 30–40° cephaladly and on the axial plane 10° laterally (Fig. 12.6).
Fig. 12.6
Schematic drawing of the Anderson technique. The entry point is the same as for the An technique (Xu et al. [8]. Reprinted with permission)
Once the trajectories have been made according to one or the other technique, as far as screw diameter and length are concerned, nowadays most manufacturers have a cervical instrumentation kit in their program and standard screw diameter is 3.5 mm with a rod of the same measure. In terms of screw length, as we will see in the next section, bicortical purchase should be obtained in order to achieve the highest biomechanical resistance of the implant. Average screw length, based on anatomical studies, is around 15 mm from dorsal to ventral cortex but this is just an indicative value.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








