SECTION IV LOCALISED NEUROLOGICAL DISEASE AND ITS MANAGEMENT A. INTRACRANIAL
HEAD INJURY
FOCAL DAMAGE
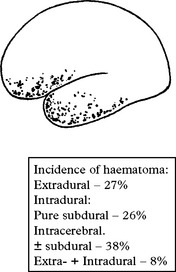
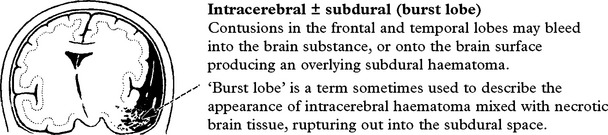
Intracranial haematoma
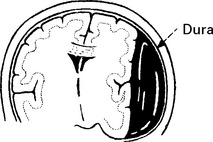
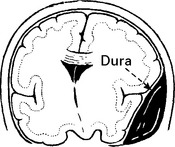
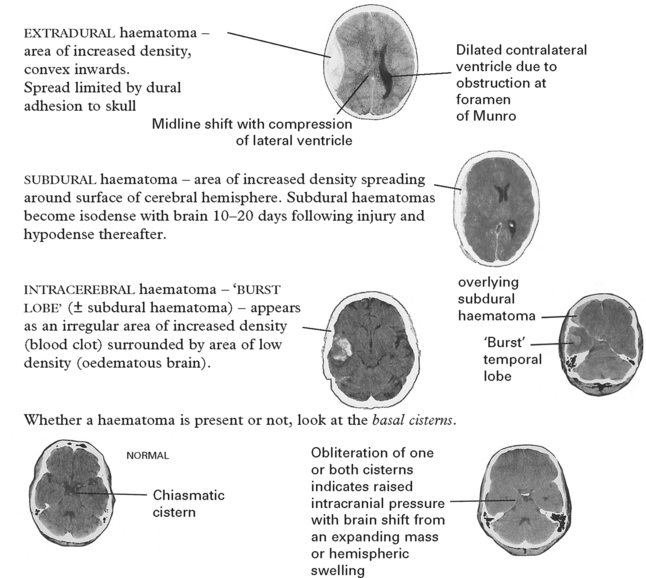
Intracranial bleeding may occur either outside (extradural) or within the dura (intradural).
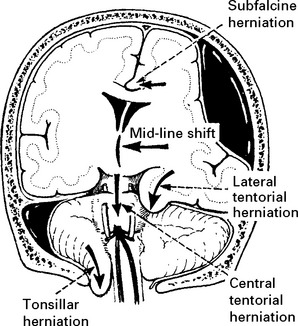
Tentorial/tonsillar herniation (syn. ‘cone”)
It is unlikely that high intracranial pressure alone directly damages neuronal tissue, but brain damage occurs as a result of tonsillar or tentorial herniation (see page 81). A progressive increase in intracranial pressure due to a supratentorial haematoma initially produces midline shift. Herniation of the medial temporal lobe through the tentorial hiatus follows (lateral tentorial herniation), causing midbrain compression and damage. Uncontrolled lateral tentorial herniation or diffuse bilateral hemispheric swelling will result in central tentorial herniation. Herniation of the cerebellar tonsils through the foramen magnum (tonsillar herniation) and consequent lower brain stem compression may follow central tentorial herniation or may result from the infrequently occurring traumatic posterior fossa haematoma.
DIFFUSE DAMAGE
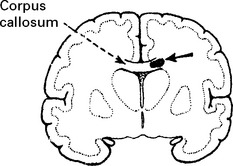
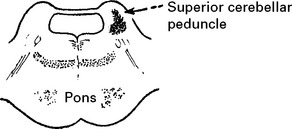
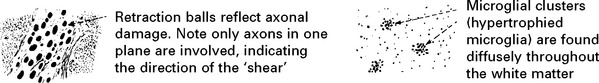
Diffuse axonal injury
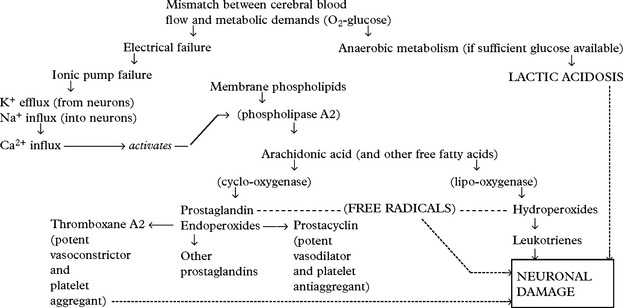
Shearing forces cause immediate mechanical damage to axons. Over the subsequent 48 hours, further damage results from release of excitotoxic neurotransmitters which cause Ca2+ influx into cells and triggers the phospholipid cascade (page 246). Genetic susceptibility conferred by the presence of the APOE ͛4 gene may also play a part. Depending on the severity of the injury, effects may range from mild coma to death.
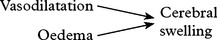
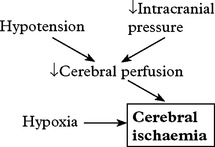
Cerebral ischaemia
Cerebral ischaemia commonly occurs after severe head injury and is caused by either hypoxia or impaired cerebral perfusion. In the normal subject, a fall in blood pressure does not produce a drop in cerebral perfusion since ‘auto-regulation’ results in cerebral vasodilatation. After head injury, however, autoregulation is often defective and hypotension may have more drastic effects. Glutamate excess and free radical accumulation may also contribute to neuronal damage (see page 246).
HEAD INJURY – CLINICAL ASSESSMENT
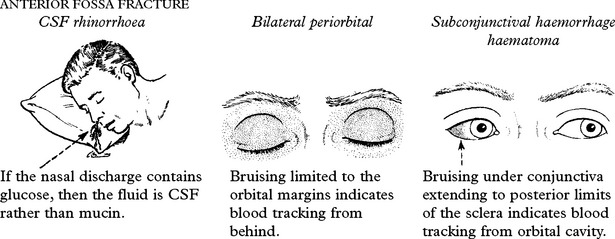
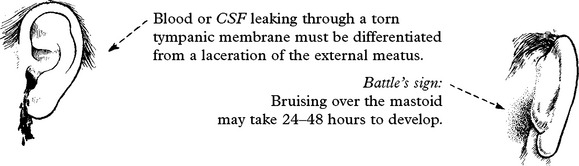
PETROUS FRACTURE
Bleeding from the external auditory meatus or CSF otorrhoea:
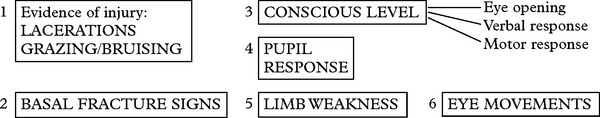
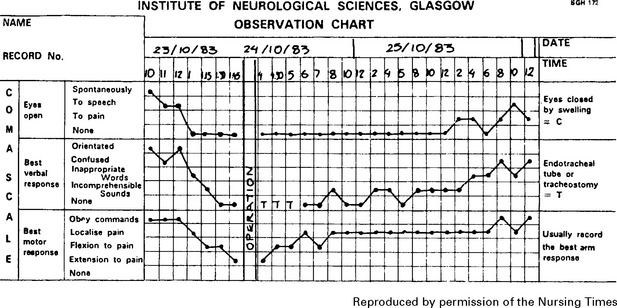
3. Conscious level – Glasgow Coma Score (GCS)
Assess patient’s conscious level in terms of eye opening, verbal and motor response on admission (see page 5) and record at regular intervals thereafter. An observation chart incorporating these features is essential and clearly shows the trend in the patient’s condition. Deterioration in conscious level indicates the need for immediate investigation and action where appropriate.
Note: This chart shows a ‘14 point scale’ with a maximum score of ‘14’ in a fully conscious patient. Many centres use a 15 point coma scale where ‘Flexion to pain’ is divided into ‘normal’ or ‘spastic’ flexion (see page 29).
4. Pupil response
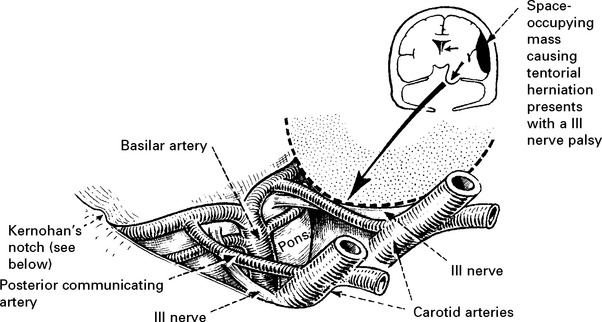
The light reflex (page 142) tests optic (II) and oculomotor (III) nerve function. Although II nerve damage is important to record and may result in permanent visual impairment, it is the III nerve function which is the most useful indicator of an expanding intracranial lesion. Herniation of the medial temporal lobe through the tentorial hiatus may damage the III nerve directly or cause midbrain ischaemia, resulting in pupil dilatation with impaired or absent reaction to light. The pupil dilates on the side of the expanding lesion and is an important localising sign. With a further increase in intracranial pressure, bilateral pupillary dilatation may occur.
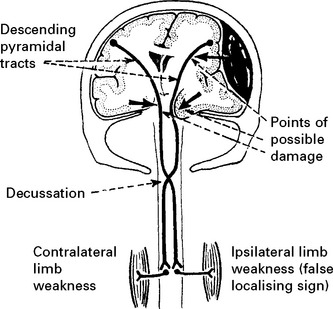
5. Limb weakness
Determine limb weakness by comparing the response in each limb to painful stimuli (page 30). Hemiparesis or hemiplegia usually occurs in the limbs contralateral to the side of the lesion. Indentation of the contralateral cerebral peduncle by the edge of the tentorium cerebelli (Kernohan’s notch) may produce an ipsilateral deficit, a false localising sign more often seen with chronic subdural haematomas. Limb deficits are therefore of limited value in lesion localisation.
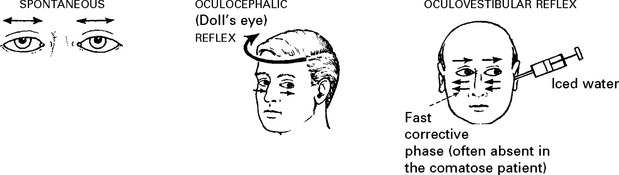
6. Eye movements
Eye movements may occur spontaneously, or can be elicited reflexly (page 30) by head rotation (oculocephalic reflex) or by caloric stimulation (oculovestibular reflex).
HEAD INJURY – INVESTIGATION AND REFERRAL CRITERIA
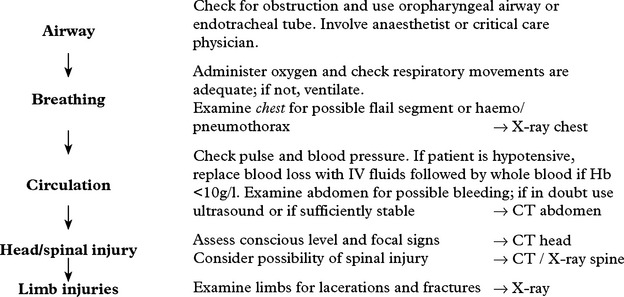
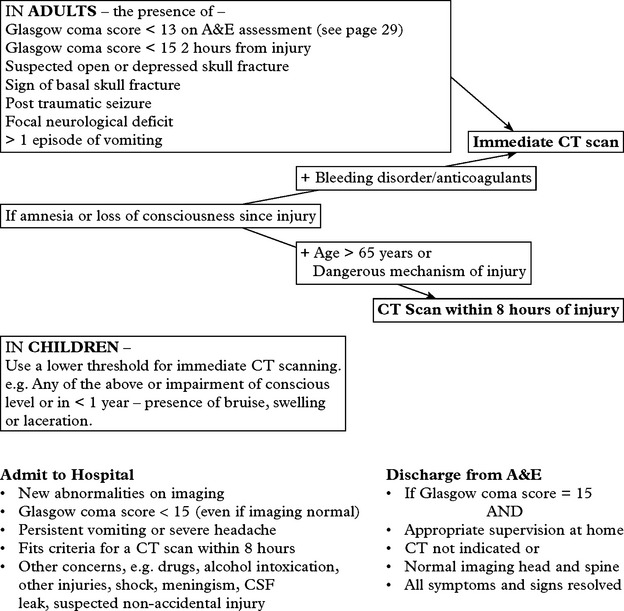
IN THE ACCIDENT AND EMERGENCY DEPARTMENT (A&E)
Various guidelines now exist. The following are based on those from the National Institute for Health and Clinical Excellence (NICE). (Further details available at http://www.nice.org.uk).
| Admit to Hospital | Discharge from A&E |
|---|---|
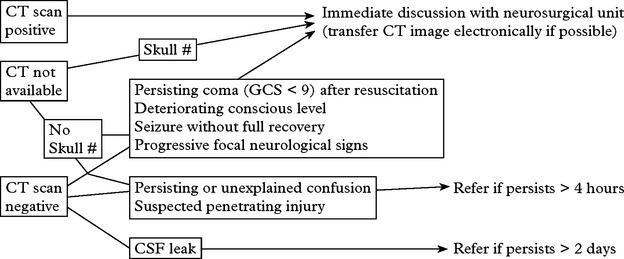
Transfer to the neurosurgical unit
Prior to the transfer, ensure that resuscitation is complete, and that more immediate problems have been dealt with (see page 221). Insert an oropharyngeal airway. Intubate and ventilate if the patient is in coma or if the blood gases are inadequate (PO2 <8 kPa on air, 13 kPa on O2 or CO2 > 6 kPa). If the patient’s conscious level is deteriorating, an intravenous bolus infusion of 100 ml of 20% mannitol should ‘buy time’ by temporarily reducing the intracranial pressure.
Cervical spine injury may accompany head injury. Guidelines also exist with criteria for investigation. (For full details see http://www.nice.org.uk/guidance/index.jsp?action=download&o=36259).
For ADULTS and CHILDREN 10 years and over
| AP, Lateral and Odontoid Peg X-rays if | CT cervical spine if |
|---|---|
HEAD INJURY – INVESTIGATION
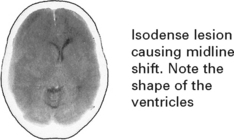
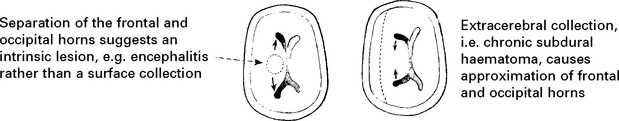
CT scan: the investigation of choice for head injury (and cervical spine injury incertain circumstances – see page 227).
Further investigation may be required to exclude other coincidental or contributory causes of the head injury, e.g. drugs, alcohol, postictal state, encephalitis (Cause of coma, see page 86).
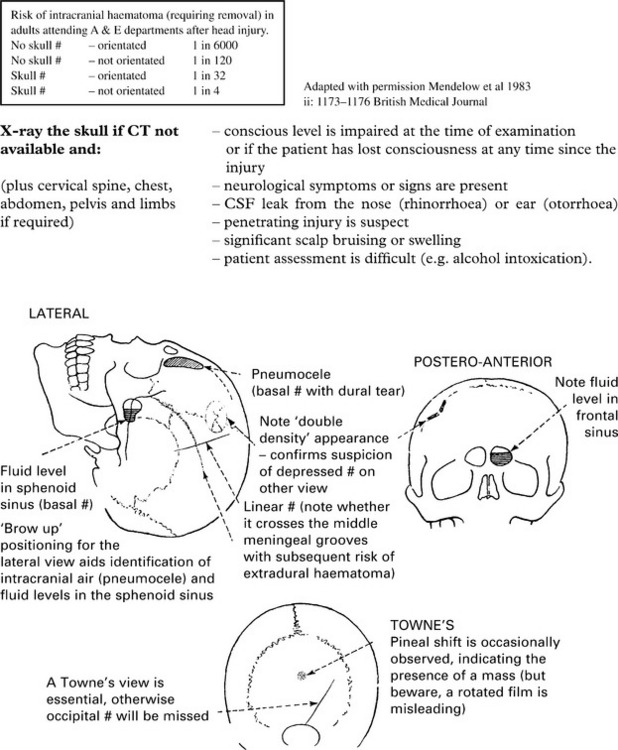
If a CT scan is not available, a skull fracture on X-ray identifies those at high risk of intracranial haematoma. In those patients, referral to a neurosurgical unit for a CT scan is essential (see page 227).
HEAD INJURY – MANAGEMENT
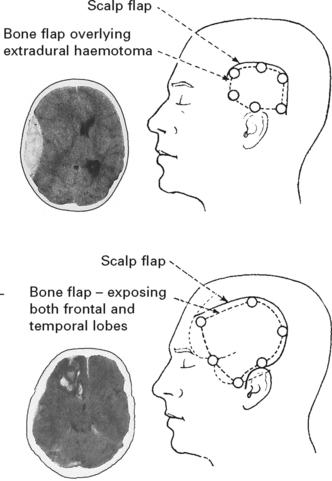
INTRACRANIAL HAEMATOMA
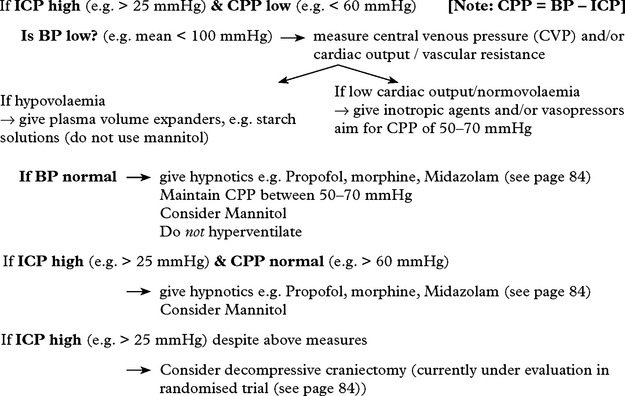
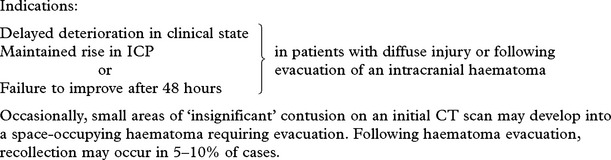
TREATMENT OF RAISED INTRACRANIAL PRESSURE (ICP)
Raised ICP in the absence of any easily treatable condition (e.g. intracranial haematoma or raised pCO2) requires careful management. The various techniques used to lower ICP have already been described (pages 83–84) but these must not be applied indiscriminately.
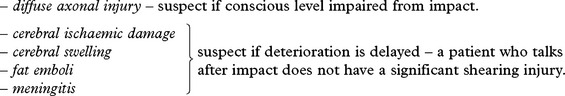
DIFFUSE BRAIN DAMAGE/NEGATIVE CT SCAN
In these patients, coma or impairment of conscious level may be due to:
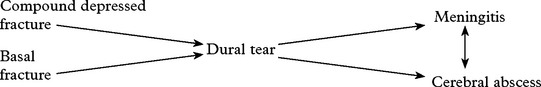
Meningitis may occur several days after injury in the presence of basal fractures.
Cerebral swelling may occur at any time after injury and cause a rise in intracranial pressure.
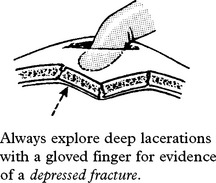
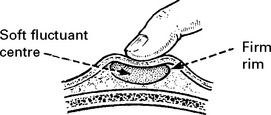
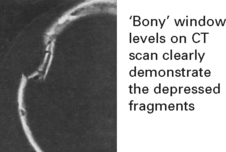
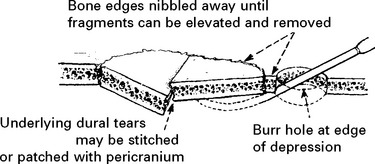
DEPRESSED SKULL FRACTURE
DELAYED EFFECTS OF HEAD INJURY
POST-TRAUMATIC EPILEPSY
Early epilepsy (occurring within the first week from injury)
The risk of early epilepsy is high in
Late epilepsy (occurring after the first week from injury)
Prophylactic anticonvulsants appear to be of little benefit in preventing the development of an epileptogenic focus. Management is discussed on page 102.
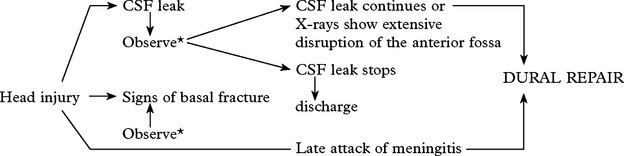
CEREBROSPINAL FLUID (CSF) LEAK
Clinical signs of a basal fracture have previously been described (page 222). The patient may comment on a ‘salty taste’ in the mouth. Anosmia suggests avulsion of the olfactory bulb from the cribriform plate.
POSTCONCUSSIONAL SYMPTOMS
Even after relatively minor head injury, patients may have persistent symptoms of:
OUTCOME AFTER SEVERE HEAD INJURY
Outcome is best categorised with the Glasgow Outcome Scale (GOS – see page 214) which uses dependence to differentiate between intermediate grades. After severe injury, about 40% regain an independent existence and may return to premorbid social and occupational activities. Inevitably some remain severely disabled requiring long term care, but few (< 2%) are left in a vegetative state with no awareness or ability to communicate with their environment (see page 214). Prognosis in this group is marginally better than for non-traumatic coma – with about one-third of those vegetative at one month regaining consciousness within one year; of those who regain consciousness, over two-thirds either subsequently die or remain severely disabled. Of those vegetative at 3 months after the injury, none regain an independent existence.
Prognostic features following traumatic coma
| Poor outcome (GOS 1–3) | Favourable outcome (GOS 4–5) | |
|---|---|---|
| Patients in coma for > 6 hours | 61% | 39% |
| Best Glasgow Coma Score > 11 | 18% | 82% |
| Best Glasgow Coma Score 8–10 | 32% | 68% |
| Best Glasgow Coma Score < 8 | 73% | 27% |
| Pupillary response – reacting | 50% | 50% |
| Pupillary response – non-reacting | 96% | 4% |
| Age < 20 years | 41% | 59% |
| Age > 60 years | 94% | 6% |
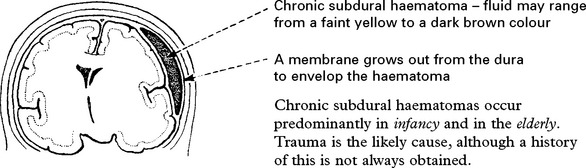
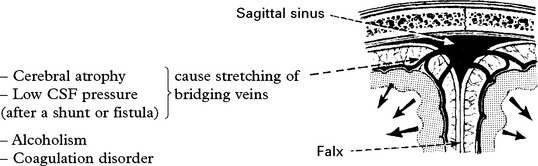
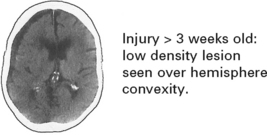
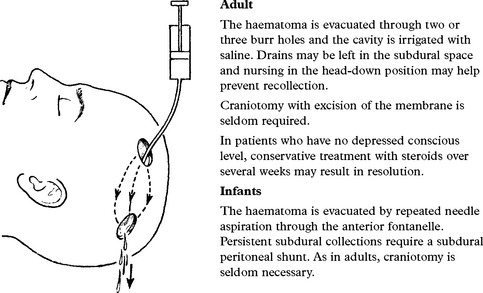
CHRONIC SUBDURAL HAEMATOMA
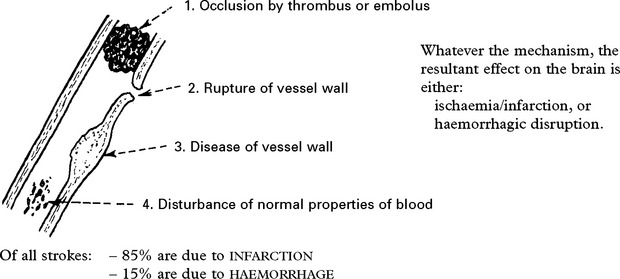
CEREBROVASCULAR DISEASES
CEREBROVASCULAR DISEASE – NATURAL HISTORY
CEREBROVASCULAR DISEASE – CAUSES
HAEMORRHAGE (20%)
| Into the brain substance – parenchymal (15%) and/or subarachnoid space (5%) | Neoplasm |
| Coagulation disorder e.g. haemophilia | |
| Hypertension | Anticoagulant therapy |
| Amyloid vasculopathy | Vasculitis |
| Aneurysm | Drug abuse e.g. cocaine |
| Arteriovenous malformation | Trauma |