♦ Preoperative
Planning
- Magnetic resonance imaging (MRI) lumbosacral without contrast. Most common study demonstrates the relationship between the pedicle and disc.
- Magnetic resonance imaging with and without contrast is required when surgery has been performed previously to distinguish scar from disc herniation.
- Computed tomography (CT) myelography is indicated in rare situations either to complement an MRI with significant metal artifact or when an MRI cannot be obtained.
- Computed tomography remains a second choice study, but it should be recognized that current era CT is far superior to CT scans from a decade ago.
Special Equipment
- Basic spine tray
- Kerrison rongeurs
- High-speed drill with “match-head” bit
Operating Room Set-up
- Wilson frame is preferred to place lumbosacral spine in flexion. This allows entry into the spinal canal with minimal bone removal.
- Operating room table must allow for intraoperative x-ray.
- Headlight and loupes
- Operative microscope is utilized once the canal has been entered as a matter of surgeon preference.
Anesthetic Issues
- Balanced general anesthesia in the majority of cases
- Intravenous antibiotics (cefazolin) given 30 minutes prior to skin incision
- Spinal anesthesia can be used for severe systemic disease.
♦ Intraoperative
Positioning
- Prone position (most common)
- Wilson frame
- Abdomen hanging free decreases intra-abdominal pressure, which decreases epidural venous pressure and decreases intraoperative blood loss.
- Pressure points and genitalia are checked.
- Spinal needle (22-gauge) is placed with reference to local landmarks. Position is confirmed with lateral x-ray or fluoroscope.
- Wilson frame
- Three quarter prone position
- Rarely used
- Advantage is less pressure on the abdomen
- Disadvantages are unfamiliar orientation and difficult to impossible intraoperative imaging
- Indications: third trimester pregnancy, marked obesity, hemodialysis patient with only remaining access at femoral arteriovenous graft
- Technique
- Position patient in true lateral.
- Obtain lateral x-ray with spinal needle in place.
- Mark spinal needle with methylene blue and design incision.
- Place bean bag anteriorly, and roll patient into three quarters prone position.
- Secure patient with 4-inch tape.
- The remainder of the operation proceeds as for the prone position.
- Position patient in true lateral.
- Rarely used
Incision
- The incision is designed with respect to the spinal needle and the x-ray image.
- The position of the needle is marked with 0.2 to 0.3 mL of methylene blue. Incisions can be limited to 2 cm if they are well positioned.
- Incisions can be marked utilizing local landmarks without reference to imaging.
- A line drawn between the two iliac crests intersects the spine between the L4 and L5 spinous processes.
- There are two paramedian dimples at S1.
Sterile Scrub and Preparation
- Betadine detergent scrub with sterile gloves for 5 minutes
- Alcohol to remove Betadine scrub
- Sterile towel to dry
- Incision is marked
- Prep and drape widely to allow incision to be extended if needed.
Initial Exposure
- Skin incision is performed with a no. 10 blade knife.
- Self retaining retractors are inserted.
- Monopolar electrocautery is used to expose the ipsilateral aspect of the spinous process above and below.
- Facia is undermined beyond the length of the skin incision to facilitate lateral exposure.
- The exposure is advanced following the subperiosteal plane from spinous process to lamina to facet. The tissue overlying the interspace can be divided with electrocautery only after the bone above and below has been exposed.
- As the dissection proceeds over the facet itself, care is taken not to denude the facet capsule with electrocautery.
- When the lateral aspect of the facet has been exposed, a Taylor retractor is inserted.
Bone Resection
- Curettes are used to clean the inferior side of the lamina above and the superior side of the lamina below.
- Angled curettes detach the ligamentum flavum from the lamina above.
- Soft tissue is cleaned from the interspace with a pituitary rongeur. The ligamentum flavum is left in place.
- A lateral laminotomy and medial facetectomy is performed with a high-speed drill and finished with curettes and a Kerrison punch. After the lamina above and the descending facet have been removed, the ligamentum flavum must be thinned to facilitate access to the ascending facet.
- The bone work is complete when the superomedial aspect of the pedicle below can be palpated with a nerve hook.
Discectomy (Fig. 120.1)
- At this point, the operating microscope is brought into the field.
- The traversing root is identified as it makes its way around the pedicle below.
- Epidural vessels are coagulated with the bipolar and divided with microscissors as the dissection proceeds superiorly to the disc space.
< div class='tao-gold-member'>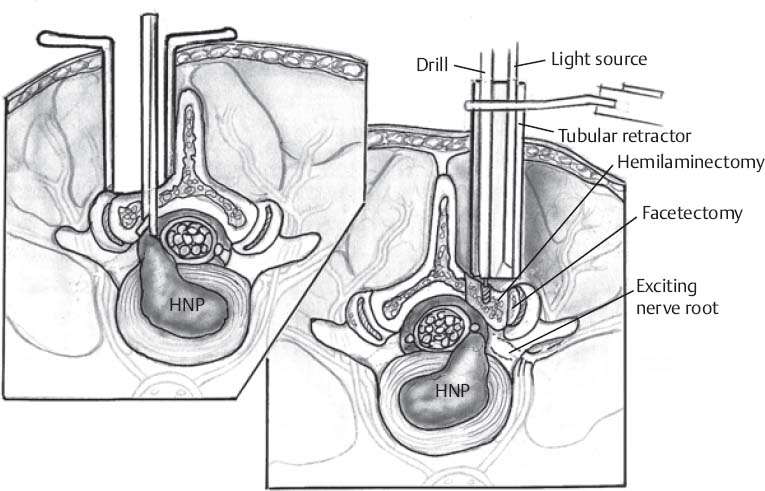 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue







