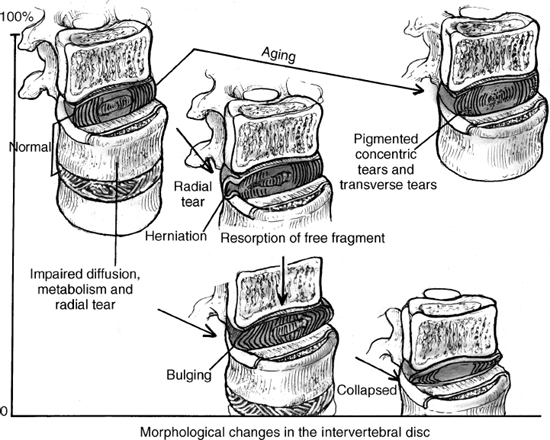
13 I. General considerations A. Incidence 1. Eighty percent of the population will experience back pain. 2. Two to 3% will experience lower extremity radiculopathy. B. Age 1. Mean age of onset is 35 years. 2. Unusual under 20 years and over 60 years of age 3. Herniated disk in children is rare. a. Slippage of an entire disk and vertebral end plate or “slipped vertebral apophyses” may mimic herniated disk. 4. Herniated disk in the elderly is also uncommon. a. May be associated with spinal stenosis C. Gender ratio is approximately equal. 1. Females typically present a decade later. D. Natural history of low back pain and sciatica 1. Low back pain resolution a. Fifty to 60% recover in 1 week. b. Ninety-five percent recover in 3 months. 2. Sciatica resolution a. Fifty percent recover in 1 month. b. Seventy-five percent recover in 1 year. 3. Surgical results are better after 1 year but no significant difference after two years when compared with nonoperative management. E. Epidemiological factors 1. Occupational a. Heavy lifting b. Vibrational exposure Figure 13–1 Schematic demonstrating the morphological changes associated with degeneration in the intervertebral disk. Signal intensity (MRI) decreases as degeneration progresses with loss of disk height. 2. Driving certain motor vehicles 3. Multiple pregnancies 4. Cigarette smoking 5. Sedentary lifestyle 6. Obesity 7. Anxiety and depression II. Pathogenesis A. Intervertebral disk degeneration (IVD) (Fig. 13–1) 1. Decreased nutrition to the IVD a. End plate sclerosis b. Decreased vascularity (1) O2 tension decreases (2) Lactate increases (3) pH decreases in the center of the nucleus pulposus 2. Decreased water content a. Normally 88% decreases to 60% by the eighth decade 3. Increased likelihood of annular tears with aging a. Decreased proteoglycan content of the nucleus pulposus leads to greater peripheral annular loading and less central nucleus pulposus resistance. b. Annular tear may cause low back pain without radiculopathy.
Lumbar Disk Disease: Pathogenesis and Treatment Options
| Type | Findings |
| Protrusion | Broad-based disk bulge |
| Extrusion | Disk herniation through the posterior longitudinal ligament. The fragment is larger than its base but still in continuity |
| Sequestered | Complete displacement of the disk with no continuity of the fragment and the intact disk |
c. Nociceptors are found on the outer anulus and posterior longitudinal ligament.
(1) The posterolateral corner is most susceptible to a fear from flexion/rotation or torsional stresses.
4. Herniation
a. Types (Table 13–1)
b. Locations
(1) Most common at L4-5 and L5-S1
(a) Less common at high lumbar and thoracic regions
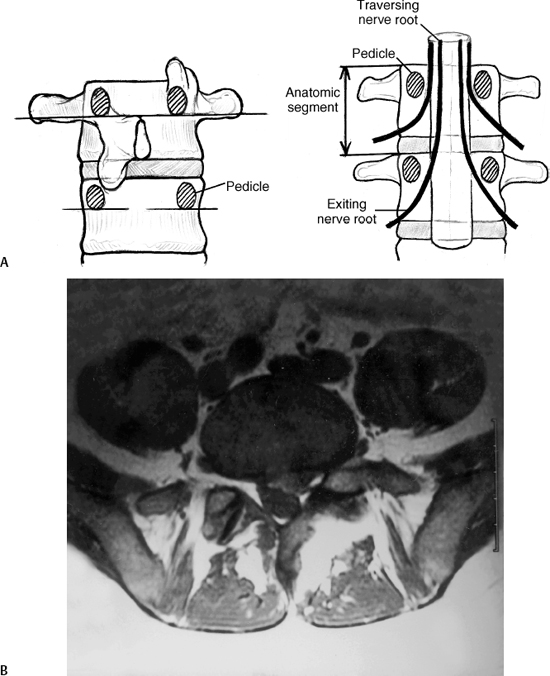
(2) Classically posterolateral with impingement of the nerve below (i.e., L4-L5 Herniated Nuclear Pulposus (HNP) affects the traversing L5 nerve root) (Fig. 13–2)
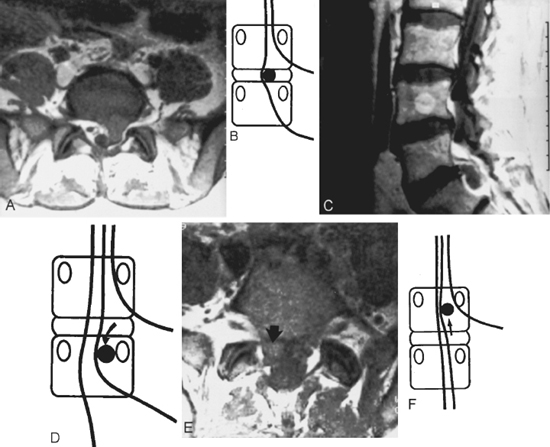
(3) Axillary herniations
(a) Usually due to cephalad and medial migration of the disk fragment
(b) Medial retraction becomes difficult and dangerous (Fig. 13–3).
(4) A small central disk herniation may cause back pain without radiculopathy or cauda equina syndrome.
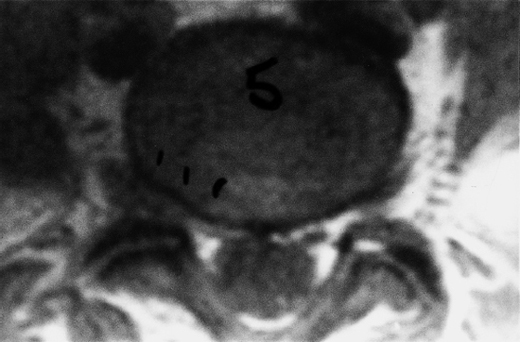
(5) Extreme lateral or foraminal herniation
(a) Impinges upon the nerve root above
(b) More common in older patients
(c) Typically found at L3 and L4 (Fig. 13–4)
(6) Intradural herniation is extremely rare.
B. Nerve roots
1. Anatomy
a. Each lumbar nerve root exits below the pedicle and above the disk.
(1) For example, the L5 nerve exits below the L5 pedicle and above the L5-S1 disk.
b. Dorsal root ganglion lies in the intervertebral foramen inferior to the pedicle, which may be the main source of pain.
c. Each nerve root has three branches.
(1) Ventral ramus for motor function
(2) Sinuvertebral nerve
(a) Innervates the outer layer of the posterior anulus fibrosus
(b) Anterior part of the anulus fibrosus has sympathetic innervation, and the afferent fibers connect with the sinuvertebral nerves.
Figure 13–2 (A) Schematic demonstrating the anatomic orientation of the exiting and traversing nerve root in relation to the intervertebral disk. Note that the exiting nerve root can only be affected by a far lateral disk herniation. (B) Typically, posterolateral disk herniations affect the traversing nerve root. An MRI showing a posterolateral L5-S1 disk herniation impinging on the left S1 nerve root.
Figure 13–3 Illustrations and MRI demonstrating various types of lumbar disk herniations. (A,B) Left paracentral L5-S1 disk herniation. (C,D) Sequestered disk fragment that migrated inferiorly to the level of the S1 pedicle. (E,F) L5-S1 axillary disk herniation.