(1)
Department of Neurological Surgery, University of Southern California Keck School of Medicine, Los Angeles, CA, USA
The major objective in surgery of herniated lumbar discs is decompression of the involved nerve root or roots and cauda equina with restitution of the normal anatomical disposition of elements of the cauda equina within the spinal and root canals. Minimal manipulation of neural elements is imperative, as an anatomical environment that will preclude recurrent root entrapment at the operated region is provided.
The lateral position provides a physiologic placement of the patient with maximum exposure of lateral elements of the main lumbar dural tube and nerve roots. At the same time, it provides a postural substrate that offers maximum exposure of the intralaminar space, ligamentum flavum, and interbody spaces in the region without risk of increased intraabdominal or intrathoracic pressure and secondary distension of the epidural venous complex.
Get Clinical Tree app for offline access

1.
Essentials of positioning. Following the induction of adequate general anesthesia, position the patient so that, with respect to the lateral position, his painful extremity is placed superiorly. In initiating positioning, we have found that the surgeon and three assistants are the optimum number to effect this maneuver with ease. The proposed level of operation is placed at the midpoint for flexion of the operating table and the patient’s back is moved to the lateral table edge closest to the surgeon. The table is then fully flexed and the inferior lower extremity is flexed at the hip and knee, with the knee supported by a padded kidney rest inserted at the break point. The superior extremity is fully extended and supported medially by two pillows, one at the level of the thigh and the other at the level of the leg. At this time several bands of 3-inch cloth adhesive tape are run from one lateral runner of the operating table to the other to maintain the pelvis in a flexed position. These maneuvers accomplish the following: (1) the lumbar curve is straightened and largely reversed, (2) the ligamentum flavum at the operative level as well as the intralaminar space is distracted, (3) the nerve root sheaths at the superior aspect of the canal are disposed and lengthened to allow for optimum exposure and visualization of the lateral recess of the spinal canal, and (4) the interbody space is distracted posteriorly and superolaterally so that adequate evacuation and visualization within the interspace may be accomplished.
The inferior axilla is supported on an axillary roll. The upper limb is supported either in a cradle or on a pillowed Mayo stand. The patient’s thorax is made parallel with the floor by manipulation of the reverse Trendelenburg setting of the operating table. The table is then side-tilted away from the surgeon so that the lumbar region is turned approximately 15 to 20 degrees from the vertical plane.
2.
The lumbodorsal region is appropriately prepped and then marked with a soft pen. Initially the posterosuperior iliac spines are identified and marked. The first interspace palpable superior to a line drawn between these spines is the L5–S1 intraspinous space. This is identified and an appropriate mark for level is made. To assist with identification of the appropriate operative level, a perpendicular line is drawn from the iliac crest to the midline, and the relationship of this line to the L4–L5 interspace is judged according to anteroposterior (AP) lumbosacral spine films. Rather than using X-ray identification of the proper level, we have found it efficacious to identify the sacrum and the L5–S1 level in all cases before embarking on decompression of the L4–L5 region. At higher levels X-ray identification has been used in the operating room.
For the purposes of this discussion, a L5–S1 exposure for decompression of the S1 nerve root and excision of the herniated nucleus pulposis at the L5–S1 level are described. An incision is marked 1 cm superior and lateral to the spines of L5 and S1. The length of this mark is variable according to the physique of the given patient. Infiltration is undertaken in the subperiosteal and paraspinous muscular planes at both the L5 and S1 levels with a solution of 0.5 % xylocaine with epinephrine. Approximately 5 to 7 mL of this solution is used at each level. The subcutaneous tissues are then infiltrated with a similar solution in the region of the marking for the incision. We use a draping system that incorporates three towels, one at the superior, one at the inferior, and one at the medial surface of the field. A 3 M Steridrape is then placed over the three towels and marked area with a cuff fashioned on the lateral field that acts as an anchor for the secondary laporotomy drapes which will follow.
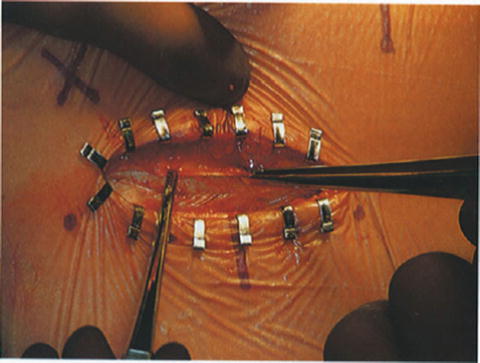
After draping, the surgeon has the option of either sitting or standing during the operative procedure. The scrub nurse positions herself or himself to the right in the case of a right-handed surgeon and the assistant is positioned to the left. A Mayo stand is placed between the surgeon and the nurse with a secondary table at his or her side to augment the essential instrumentation for each portion of the case as it evolves. A 9 French suction apparatus is positioned on the surgeon’s left and a blunt-tipped bipolar coagulating forceps is placed on the surgeon’s right for easy access (Fig. 47.1).


Fig. 47.1
The lateral position for lumbar disc surgery provides a physiologic placement of the patient with maximum exposure of lateral elements of the dural sac and nerve roots. The lateral position offers maximum exposure of the intralaminar space, ligamentum flavum, and interbody spaces in the region. There is no risk of increased intraabdominal or intrathoracic pressure with its secondary distension of epidural veins with the lateral decubitus position. It is a comfortable position for the surgeon either sitting or standing and provides excellent visualization for teaching. The operative level is placed at the midpoint for flexion of the operating table and the patient’s back is moved to the lateral edge of the table. The lower leg is flexed and padded. The upper leg is fully extended, supported on two pillows
The patient is stabilized in this position with rolls of tape. The inferior axilla is supported with an axillary roll. The upper limb is in a cradle. The patient’s thoracic spine is made parallel with the floor by manipulation of the reverse Trendelenburg setting on the operating table. The table is then tilted away from the surgeon so that the lumbar region is turned approximately 15–20 degrees from the vertical plane. In summary, the position allows (1) straightening and reversal of the lumbar curve; (2) distraction of the inner laminar space and ligamentum flavum; (3) maximum visualization of the lateral recess of the spinal canal; and (4) distraction of the inner body space posteriorly and superolaterally so that adequate evacuation and visualization within the inner space may be accomplished.
3.
Incision and laminar exposure. With incision of the cutaneous and subcutaneous spaces, the lumbodorsal fascia is identified approximately 1 cm parallel to the spines of L5 and S1. Bleeding at the cutaneous margins is controlled with Michel clips, which also prevent the displacement of the Steri-drape from the wound edge. The spines of L5 and S1 are identified by palpation and an incision is made parallel to these spines in the lumbodorsal fascia to expose the paraspinous muscular groups (Fig. 47.2). The assistant introduces a hand Meyerding retractor and the surgeon, using a 20-mm Hoen periosteal elevator, develops a subperiosteal plane at the level of the spine of S1 and develops this plane inferiorly along the spine to the level of the lamina. Once the lamina is appreciated, the periosteal instrument is rotated in position and appropriately utilized so that the subperiosteal plane can be developed laterally to the level of the facet joint. The assistant introduces gauze sponges to assist in the dissection of the paraspinous musculature (Fig. 47.3). Attention is then turned to the L5 spine where a similar dissection is undertaken, before which Mayo scissors are employed to incise the multifidus rotator that separates the two spines in a muscular band. This dissection being completed, the gauze packings are removed; the hand Meyerding retractor is introduced laterally to the level of the facet joint and palpation is undertaken. The sacrum is identified as well as the lamina of L5. Retraction of the paraspinous musculature is then maintained with a Hoen self-retaining retractor. To position this instrument optimally, initially the spinous component of the retractor system is placed at the midline; next, the muscle retracting blade is placed over the hand Meyerding retractor and that retractor is removed; finally, the handle of the retractor system is attached to both blades and retraction is effected. Removal of retained muscle may then be undertaken with a pituitary rongeur.