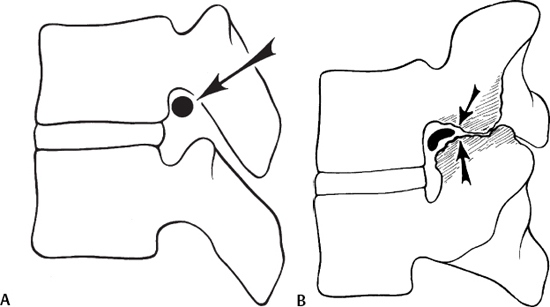
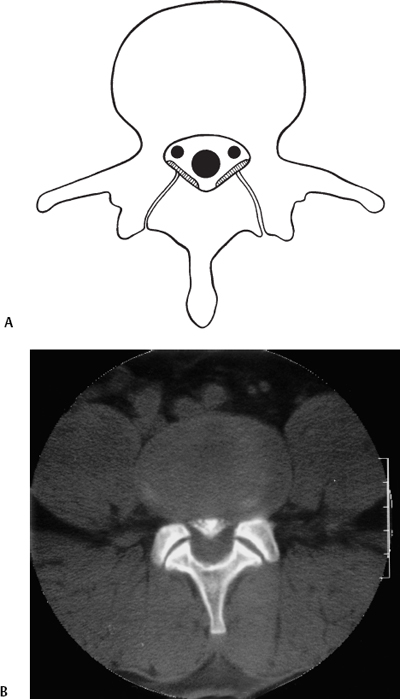
14 I. General considerations A. Definition: narrowing of the spinal canal (central stenosis), lateral recess (lateral recess stenosis) or the foramen (foraminal stenosis) with neural impingement that produces symptoms of neurogenic claudication or radiculopathy B. Degenerative spinal the stenosis is significant only if clinically symptomatic. C. More common after the fifth decade D. Men more affected than women E. Associated with disc degeneration II. Classification A. Congenital: usually developmental and primarily central canal stenosis 1. Idiopathic 2. Dwarfism (achondroplastic) B. Acquired 1. Degenerative stenosis a. Central stenosis (1) Enlargement of the inferior facet, ligamentum flavum, and bulging disc b. Lateral stenosis (1) Enlargement of the superior facet and ligamentum flavum c. Foraminal stenosis (1) Narrowing of the foramen 2. Degenerative spondylolisthesis a. L5 nerve is entrapped between the inferior facet of L4 and the posterior aspect of the body of L5. 3. Combined a. Disc herniation, superimposed upon a degenerative or congenitally stenotic canal 4. Iatrogenic a. Postlaminectomy, postfusion, post-disc surgery 5. Posttraumatic changes a. Paget’s disease, fluorosis III. Pathogenesis A. Variation of spinal canal may predispose to spinal stenosis. 1. Three types of spinal canal a. Round canal b. Oval canal c. Trefoil canal (15%) (1) Napolean’s hat shape (2) Trefoil canal predisposes to lateral recess stenosis. B. Disc degeneration 1. Aging versus degeneration 2. Changes in the collagen, proteoglycans, and water content C. Facet joint involvement 1. Follows disc degeneration 2. Joint cartilage loss, hypertrophy, osteophytes, and subluxation D. Three-joint complex 1. Two posterior facet joints and the disc are all involved in the pathogenesis. 2. Degenerative changes of the three-joint complex secondary to repeated rotational and compression injuries. 3. Intervertebral discs develop circumferential and radial tears, with a loss of disc height. 4. Posterior joints undergo synovitis, cartilage destruction, osteophyte formation. a. Results in capsular laxity, ligamentum flavum hypertrophy or buckling, and joint instability or subluxation 5. Instability a. Degenerative spondylolisthesis b. Retrolisthesis c. Degenerative scoliosis d. Rotatory listhesis E. L4 or L5 nerves are more typically affected 1. Greater compressive and shear stresses 2. Pedicles of low lumbar spine have convex inferior borders as compared to concave inferior border in the upper lumbar spine. 3. Disc degeneration is most common at L4-L5 and L5-S1. F. Nerve 1. Anatomy a. Cauda equina and thecal sac (central canal) b. Superior nerve root (lateral recess) c. Dorsal root ganglion (intervertebral foramen) d. Spinal nerve (extraforaminal) 2. Cauda equina is compressed centrally from the anteroposterior direction at the intervertebral disc level a. Bulging disc anteriorly b. Ligamentum flavum and facet joints posteriorly Figure 14–1 (A) Schematic demonstrating the anatomic location of the nerve root within the neuroforamen. (B) Neuroforaminal stenosis with nerve root impingement secondary to facet hypertrophy and osteophytic compression secondary to the superior articular process. 3. Nerve root can be compressed at multiple anatomic locations a. Entrance zone (1) Posterolateral herniated disc (2) Hypertrophic superior articular process b. Middle zone (1) Pars interarticularis (spondylolysis) 4. Exit zone (foramen) (Fig. 14–1) a. Anatomy (1) Bounded by vertebral body and disc anteriorly, pedicles superiorly and inferiorly and pars, ligamentum flavum, and tip of superior articular facet posteriorly (2) Laterally herniated disc or anulus (3) Superior facet subluxation may compress the nerve against pedicle, body, or bulging anulus. b. Extraforaminal compression (1) Extreme lateral or extraforaminal herniated disc (2) “Far-out syndrome” (a) Transverse processes of L5 and sacral ala in spondylolisthesis (3) Transverse fracture or bone graft anterior to the transverse processes 5. Dimensions of stenosis (Fig. 14–2) a. Central (1) Absolute stenosis: midsagittal lumbar diameter <10 mm (2) Relative stenosis: 10 to 13.5 mm b. Lateral recess (1) Less than 3 to 4 mm
Lumbar Spinal Stenosis
Neupsy Key
Fastest Neupsy Insight Engine