Lumbar Surgical Approaches for Nonfusion Techniques
Marco Brayda-Bruno
Franco Gobetti
Alessio Lovi
Marco Teli
A nonfusion option in low back pain (LBP) surgery has become more and more popular as an alternative strategy to fusion in the treatment of patients with disc-related pain unresponsive to nonoperative care. Although still in the early phases of development after some pioneer devices, the future in this field is promising and the motion-preservation techniques will become part of the spine surgeon’s armamen-tarium, especially with the introduction of new materials and new implants designs. Lumbar disc or nucleus prosthesis and posterior lumbar “dynamic” instrumentations were introduced in the last 10 to 15 years, showing promising results in short- and midterm outcomes, which must be confirmed in long-term follow-up studies.
One of the most important aspects in this “functional” surgery is to preserve as much of the anatomic structures as possible (muscles, fascia, ligaments, and joints) during the surgical exposure.
Using less invasive surgical approaches to the spine, it is possible to adequately expose the desired anatomic structures while minimizing the disadvantages of excessive soft tissue stripping, dissection, and prolonged retraction. Several studies have demonstrated that prolonged soft tissue retraction generates a greater force per unit area on the retracted tissues, resulting in an increased regional ischemia, leading to paraspinal electromyogram abnormalities and decreased muscle density. Muscle weakness and denervation could be critical consequences resulting in potentially long-term adverse side effects, such as chronic pain and muscular dysfunction.
This can then be prevented by minimizing the traditional approaches (anterior or posterior) to the lumbar spine using new retractors, video-assisted techniques, and/or navigation. On the other side, one of the most important drawbacks to minimally invasive surgery entails the long learning curve necessary to master the various techniques (1).
Posterior Approaches
Posterior approaches to the lumbar spine for nonfusion techniques are used for interspinous devices (2) and for dynamic pedicular screws implants (3).
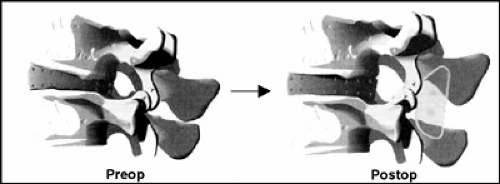
Interspinous systems are designed to provide dynamic stabilization to the lumbar spine, creating a tension-bend in the posterior column. These implants control the
extension of the spine, reduce the stress on the facet joint, and maintain foraminal height. This kind of dynamic stabilization is totally reversible without compromising any other future option for revision/salvage surgery (Fig. 11.1). Different types of interspinous devices are available (i.e., peek, titanium, silicone).
extension of the spine, reduce the stress on the facet joint, and maintain foraminal height. This kind of dynamic stabilization is totally reversible without compromising any other future option for revision/salvage surgery (Fig. 11.1). Different types of interspinous devices are available (i.e., peek, titanium, silicone).
For the implantation of an interspinous device, the patient is placed in prone position, generally with some hip flexion. But it is crucial to choose the proper individual patient position, according to the preoperative lordosis, to allow an easy approach to lumbar canal (when necessary) and the insertion of the correct size of implant, and to prevent any postoperative misalignment of the final segmental lordosis.
A midline approach is used: The skin incision is centered over the target lumbar segment(s) to stabilize, using fluoroscopy (generally for a single-level implantation a 4-cm skin incision is enough to address the two spinous processes).
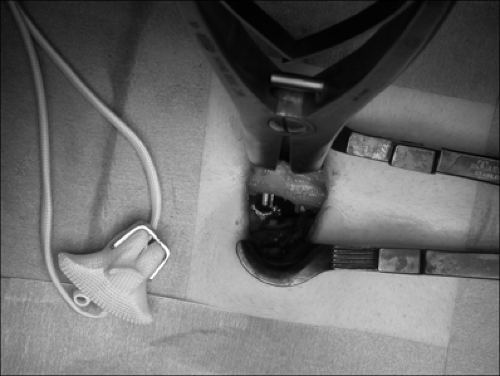
The multifidus muscle is detached from spinous processes bilaterally, the supraspinous ligament is cut, and the interspinous ligaments are deeply removed unto the ligamentum flavum, avoiding any damage to the bony structure of the spinous processes. For one-level stabilization, soft tissues retraction can be obtained with a traditional Caspar retractor used in a specific way (Fig. 11.2).
This technique is common for all interspinous devices (with a longer or shorter skin incision due to the specific characteristics and the ancillary instruments of each different implant). An appropriate size of implant is then inserted into the interspinous space, and if still possible, the supraspinous ligament is sutured.
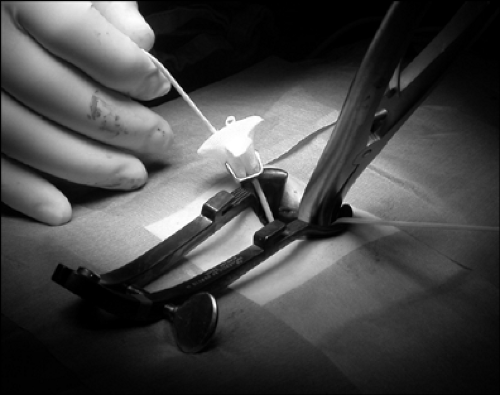
A soft interspinous device (DIAM Spinal Stabilization System, Medtronic) allows a lateral placement, too, by removing only the interspinous ligament and inserting the implant beneath the preserved supraspinous ligament (Figs. 11.3, 11.4, 11.5).
In case a decompression of neural canal and/or a herniectomy-discectomy are necessary at the same level, they must be of course performed before the insertion of the interspinous device.
A dynamic pedicular screws instrumentation (i.e., Dynesys) is designed to stabilize the spine, preserving painless intersegmental kinematics and avoiding fusion in degenerative disease associated with instability (Fig. 11.6).
These implants can be placed throughout the classical midline approach or the Wiltse paraspinal approach (4); the
actual trend in spinal surgery is favorable to the latter, whenever possible, because it is less traumatic than the former in muscular detachment and in blood loss. The Wiltse paraspinal approach allows to expose the posterolateral part of the lumbar pedicles through an intermuscular splitting between the multifidus and the longissimus muscles (Fig. 11.7).
actual trend in spinal surgery is favorable to the latter, whenever possible, because it is less traumatic than the former in muscular detachment and in blood loss. The Wiltse paraspinal approach allows to expose the posterolateral part of the lumbar pedicles through an intermuscular splitting between the multifidus and the longissimus muscles (Fig. 11.7).
Wiltse et al. proposed to make the skin incision approximately 2 cm lateral from the midline and just medial to the posterior-superior iliac spine bilaterally. Similar incisions are made in the fascia at the same distance from the spinal processes. The index finger can then be used as a dissector inside the sacrospinalis above the L4-5 level to reach the lumbar spine.
Although Wiltse et al. described the technical details of this approach in 1968, the exact location of trans-sacrospinalis splitting is still unclear.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree