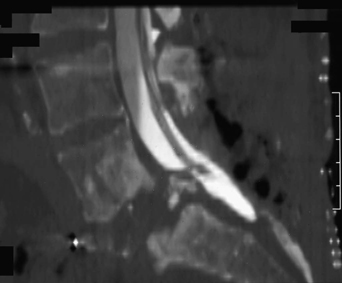
62 A 48-year-old woman had a resection of a lumbosacral giant cell tumor a decade ago, followed by radiation. A few years later, she had facet wiring for lumbar segmental instability. Following a minor trauma, she described low back pain. She also had some pain and limited weakness of the right lower extremity. Workup did not reveal recurrence. Magnetic resonance imaging (MRI) and dynamic films of the lumbosacral spine demonstrated mobile anterolisthesis of L5 on S1, with scar, and some thecal sac displacement. Preoperative, reconstructed lumbosacral computed tomography (CT) myelogram shows thecal sac compression in Fig. 62-1. Segmental instability L5–S1 decompression with bilateral L4–S2 pedicle screw fixation with autograft was completed. The postoperative construct can be seen in Fig. 62-2. Giant cell tumors are rare, benign, resilient, lytic, destructive bony tumors. The sacrum is the fourth most common location for these tumors, following the femur, tibia, and radius bones. The mean age of presentation is 26 years and average duration of symptoms is 4 months prior to presentation. Patients typically present with low back pain and lumbosacral radiculopathy, with or without neurologic deficit based on the stage of the disease. CT scan is a useful staging study. These tumors have a predilection for the upper sacral segments and often extend eccentrically to the sacroiliac joint. This eccentric extension can help differentiate radiologically a giant cell tumor from a chordoma. The treatment of a sacral giant cell tumor remains controversial, and although complete en bloc resection provides the best chance for tumor control (85%), it requires a 360-degree approach, intensive reconstruction of the lumbosacral-iliac region, and has a high risk of neurologic damage. Alternative options include tumor resection and curettage of the bony margins (which preserves the adjacent joint) followed by high-dose radiation therapy. More recently, the use of shaped beam radiosurgery has been advocated. Nonetheless, there is a higher rate of recurrence with less aggressive therapy.
Lumbosacral Giant Cell Tumor with Segmental Instability
Presentation
Radiologic Findings
Diagnosis
Treatment
Discussion
Lumbosacral Giant Cell Tumor with Segmental Instability
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








