Chapter 4
Making Sense of the Clinical Picture
Chapter objectives
- Use the International Classification of Functioning, Disability and Health framework recommended by the World Health Organisation to describe the process of assessment used to understand the client’s personal and environmental contexts, and to gather and link assessment information at the levels of body structure/function and activity/participation.
- Detail processes for assessment of impairment factors including positive and negative features of the upper motor neuron syndrome, passive and active range of motion, movement patterns, hypertonicity and spasticity.
- Discuss the development of realistic and achievable goals for daily life, along with aims for upper limb movement that support these goals.
Abbreviations
| ARAT | Action Research Arm Test |
| AROM | Active range of motion |
| ASAS | Australian Spasticity Assessment Scale |
| CAP-M | Comparative Analysis of Performance—Motor |
| CMC | Carpometacarpal (joint) |
| COPM | Canadian Occupational Performance Measure |
| DIP | Distal interphalangeal (joints) |
| ED | Extensor digitorum (also known as extensor digitorum communis) |
| FDP | Flexor digitorum profundus |
| FDS | Flexor digitorum superficialis |
| GAS | Goal attainment scaling |
| ICF | International Classification of Functioning, Disability and Health |
| IF | Index finger |
| IP | Interphalangeal (joints) |
| LF | Little finger |
| MACS | Manual Ability Classification Scale |
| MAUULF | Melbourne Assessment of Unilateral Upper Limb Function |
| MCP | Metacarpophalangeal (joints) |
| MF | Middle finger |
| MASMS | Modified Ashworth Scale of Muscle Spasticity |
| MTS | Modified Tardieu Scale of Muscle Spasticity |
| PROM | Passive range of motion |
| QUEST | Quality of Upper Extremity Skills Test |
| RPM | Rapid passive movement |
| RF | Ring finger |
| ROM | Range of motion |
| ULADL | Upper Limb Assessment in Daily Living scale |
| UMNS | Upper motor neuron syndrome |
4.1 The ICF as an assessment framework
The purpose of assessment is twofold: to provide a baseline from which to evaluate change over time, and to assist the clinician and client to form an intervention plan. In order to address the first purpose, one must consider which aspects of the client’s functioning may change over time in response to intervention. The International Classification of Functioning, Disability and Health (ICF) [1] is a useful framework for considering the levels at which assessment information can be gathered. Figure 4.1 shows the three different components or levels of functioning and disability conceptualised in the ICF: participation, activity, and body structure and function, as well as the environmental and personal factors that influence health. Participation refers to involvement in life situations (problems are termed restrictions), while activity refers to the execution of tasks (problems are termed limitations). Body structure and function refers to the anatomical parts and physiological functions of the body (problems are termed impairments) [1].
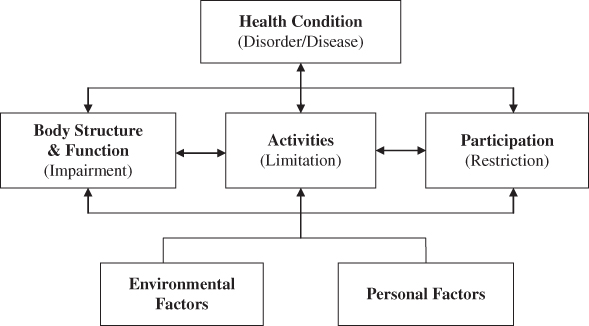
Figure 4.1 The International Classification of Functioning, Disability and Health [1].
An important aspect of the ICF has been its influence on the development of assessment tools that measure activity and participation [2, 3]. While embracing the increasing emphasis on assessing activity and participation, clinicians working with people with brain injury continue to advocate the importance of assessing impairment level factors, such as spasticity, joint range of motion (ROM) and strength [4, 5]. However, rather than just gathering information within different levels of function, it is suggested that the critical component of assessment is linking this information across levels, so that it is clear how impairment factors are contributing to activity limitations and participation restrictions [6, 7].
Evidence suggests that impairment factors do contribute to activity limitations and quality of life. For example, impairments such as spasticity, muscle tone, stiffness and reduced ROM were found to be significantly correlated with scores on the Action Research Arm Test (ARAT), an upper limb activity measure [8, 9]. In addition, using a self-report spasticity questionnaire, Petropoulou [10] found that participants reported greater difficulty with daily tasks, such as sleep, hygiene, routine tasks and social activities in the presence of more severe spasticity. Turner Stokes et al. [11] used Goal Attainment Scaling (GAS) to measure improvements in upper limb activity, mobility, self-care, domestic and community activity after Botulinum toxin injection. Findings indicated that a reduction in spasticity was highly correlated with achievement of these goals. Linking information across the activity, participation and body structure/function levels can therefore guide the second purpose of assessment, namely, forming an intervention plan that addresses activity and participation directly, and that also targets impairment factors which are limiting activity and participation [6, 12, 13].
However, all information about body structure and function, activity and participation needs to be considered against the background of the person’s context. Understanding the physical, social and cultural environments within which a person spends his or her time, together with personal factors such as habits, and past and current experience, is critical to planning and implementing an intervention that is meaningful to the client and which motivates commitment.
This chapter describes information gathering related to personal and environmental factors, assessment at the three levels of participation, activity and body structure/function, and linking this assessment information between the various levels of assessment. The remainder of the chapter details how to gather relevant and individualised information about each person’s upper limb.
4.2 Gathering information
4.2.1 The whole picture: assessment information about personal and environmental contexts
Any intervention that is chosen to address upper limb performance issues must both accommodate the person’s environmental and personal contexts (see Figure 4.1) and seek to make positive changes to, or maintain, valued aspects of his daily life. Therefore, it is critical that the information gathered during the ‘assessment process’ builds as clear a picture as possible of the client’s situation. In particular, it is important to understand the factors that may impact on the person’s ability to commit to an intervention and which may later influence her perception of the effectiveness of the intervention in making a difference to daily life. For people with acquired brain injury this ‘big picture’ information may assume different degrees of importance at different stages of recovery and rehabilitation. For example, when in acute care, carrying out upper limb interventions
may be predominantly the responsibility of health care staff. At a later stage, it will be important that the clinician has gathered sufficient information about the client’s home supports and resources to determine whether the same intervention can continue to be
used at home or in other care environments. However, even in the early phase of intervention, information about the client’s family situation and the roles that the person hopes to maintain or assume within daily contexts will impact on treatment priorities and decisions.
Contextual and personal information play a key role in the clinician’s provision of tailored information to the client and significant others, and in the promotion of collaborative decision-making about goal setting and intervention choice. For example, information about context (the client’s social situation, relevant medical history, past interventions) and personal factors (daily activities, interests and preferences, client and caregiver goals and expectations for intervention, experiences of, and attitudes towards, particular interventions, client and caregiver capacity to implement interventions) were found to be gathered by an expert occupational therapist working in a neurological setting [14]. The therapist indicated that the overall purpose of gathering such assessment information was to facilitate the client and/or caregivers to make the final decision about intervention in an informed manner, with a realistic view of what the intervention process was likely to entail and what it might achieve. It is anticipated that broad, but detailed, information gathering will assist the clinician to understand client and caregiver needs and motivations, and that such understanding will assist in facilitating client commitment to the intervention (see Box 4.1 for an example).
Most organisations use setting-specific interview tools for initial information gathering. Depending on the service environment and scope, these tools may take the form of closed-response checklists or standard, structured questionnaires that ask the same information of all clients. This type of interview format will be appropriate in certain settings, such as emergency services or in the initial stages of acute care when only limited contextual information can be used to shape goals. However, once the client is receiving rehabilitation or community-based services, this type of questioning will be inadequate for helping the clinician to form a clear picture within which to situate goal setting and intervention decisions. As the breadth and nature of the information gained will reflect the questions asked, it is worthwhile for the clinician to consider the processes that will most effectively elicit a complete picture of the client’s contextual and personal circumstances (see Box 4.2).
4.2.2 Assessment information about activity and participation
Although participation in life situations is recognised as the ultimate aim of rehabilitation and health services [15], defining the concept of participation and finding ways to measure it has presented a challenge [16, 17]. Some assessments purport to measure participation, but more often actually measure activity performance. Although related, these two concepts are subtly different [18]. ‘Performance’ considers an individual’s ability to achieve certain life activities [19, 20], for example, cutting out paper shapes with scissors or washing oneself in the shower. In contrast, ‘participation’ reflects one’s ability to assume certain roles in life situations at the societal level [17, 21]. For instance, even if a child is able to perform the task of cutting with scissors, she may not participate in this activity when the rest of her kindergarten class is making a collage. An adult with an upper limb impairment who is able to wash himself in the shower may still ask his partner for help due to the effort and time involved in completing the task independently. In these cases, participation in the life situation is more about whether the individual chooses to perform the task within the societal context in which it is usually executed.
Commonly used assessments such as the Modified Barthel Index [22] or the Functional Independence Measure [23] are, therefore, useful measures of performance, but do not capture participation [17]. Consequently, clinicians may either consider adopting measures that have been evaluated as assessing participation if such measures suit the service context, or they may gather information about a client’s participation in daily life roles using in-depth interviewing techniques. Examples of assessment tools that measure adult participation include the Activity Participation Questionnaire [24] and the Personal and Social Performance scale [25]. For children, examples include the Participation and Environment Measure for Children and Youth which can be used with children from 5–17 years [26] and the Children’s Participation Questionnaire, aimed at children aged 4–6 years [27]. In-depth interviewing techniques may include asking the client to explain a typical day or life situation, or to complete a log of participation in activities within usual environments across the week. In health service settings, time limitations often require that this information is only gained for a targeted range of daily activities. Even so, gathering key participation measures can be a powerful indicator of intervention outcomes.
Within neurorehabilitation settings, information gathering at the level of activity is more developed than at the participation level. A number of reviews have been published to assist the clinician in comparing and contrasting available activity measures, some also describing the development of new assessment tools [3, 28–31]. It is important to note that the usual focus of these tools is the activity of the person with the impaired upper limb. Considering the high level of dependence on caregivers that some clients with more severe impairments have, ways of measuring change in activity for the caregiver is often also important (see Box 4.3).
Tools developed at the activity level of the ICF have been created to measure two different aspects of activity: capacity (the highest level of functioning of which a person may be capable, usually measured in a standardised environment) and performance (how the person functions in daily life situations, measured in his current environment) [3]. In a systematic review of instruments aimed at activity-level assessment for people with hemiplegia, Lemmens et al. [3] found that many common tools, such as the Action Research Arm Test (ARAT) for adults [35], and the Quality of Upper Extremity Skills Test (QUEST) [36] and the Melbourne Assessment of Unilateral Upper Limb Function (MAUULF) [37] for children, assessed capacity rather than performance (the QUEST and the MAUULF were found to be the best measures of unilateral capacity in a separate systematic review of upper limb activity measures for children [29]).
Capacity assessments use prescribed tasks, such as reaching for a pre-determined object or playing with a pre-selected toy. For example, the ARAT has four subtests that cover gross arm movement, grasp, grip and pinch, and involves the client performing specific actions and picking up standard objects, such as a block [35]. The Motor Assessment Scale is another capacity assessment that focuses on the client’s ability to perform a number of specific arm and hand actions in three of its eight subscales, such as picking up a jellybean from a cup and putting it in another cup [38]. These upper limb capacity assessments are often used as baseline measures that can be easily repeated in a clinical environment. However, the degree to which these measures can represent meaningful outcomes in daily life may be limited, and the need for additional measures of change in daily activity performance is increasingly being recognised. For example, after identifying the limitations of capacity assessments, Rousseaux et al. [30] developed the Upper Limb Assessment in Daily Living (ULADL) Scale as a tool to collect patient-reported and observational information about upper limb function in daily life activities from adults with stroke.
In the systematic review of activity measures by Lemmens et al. [3], the majority were described as assessing perceived performance (as reported by questionnaire or interview) rather than actual performance. These included the ABILHAND [39] and ABILHAND-Kids [40] as well as broader goal-setting tools, such as the COPM [41] and GAS [42]. Only a few tools were considered to assess actual performance, including the Assisting Hand Assessment developed for children with cerebral palsy [20], and the Functional Arm Activity Behavioural Observation System developed for stroke clients [43].
A subset of these activity performance tools are those that are primarily classification tools, such as the Manual Ability Classification Scale (MACS), which classifies manual performance of children with cerebral palsy across five levels depicting the quality of object handling and the degree of assistance that is required [44]. Classification tools, as well as the activity performance measures described previously are useful as baseline measures to determine intervention effectiveness. These tools provide more information about the quality of upper limb activity in daily-life situations than those that measure capacity. For example, a child with cerebral palsy may move from a pre-intervention Level IV on the MACS (handles a limited selection of easily managed objects but with continuous support) to Level III (handles objects with difficulty but only needs help to prepare or modify activities) post-intervention. Similarly, the ULADL aims to rate changes in the quality and effectiveness of using the stroke-affected upper limb in daily activities by means of a continuous visual analogue scale [30].
Even these more ecologically-based activity performance measures do not, however, fulfill all the purposes of assessment, in that they are limited in terms of assisting clinicians to make decisions about which intervention to choose. Although such measures might clarify the next level of upper limb performance to aim for (e.g. stabilising an object using a fingertip grasp), assessment information about body structure/function is still required to determine specifically what it is about the upper limb that needs to change in order to support increased performance. For example, does the client need to achieve a certain isolated movement? Do particular muscles or muscle groups need to be lengthened to achieve a different limb position for reach and grasp? Does malalignment of certain joints during activity, either due to weakness or hypertonicity, need to be controlled or reduced in some way to allow particular positions to be maintained or movements to occur? Does severe malalignment at rest need to change in order to make daily care easier for a caregiver? And how much does it need to change? These questions can only be answered by gathering information about body structure and function.
4.2.3 Assessment information about body structure and function
The type of information gathered at the body structure and function level has typically included measurements of passive and active range of motion (PROM, AROM), type and degree of spasticity, and muscle strength [45]. Depending on the client group, assessment of sensory status may also be routinely gathered. Many clinical settings will use a standard assessment form or process to gather this information from each client at defined points, such as initial assessment and post-intervention. Often, though, the clinician will spend significant time gathering comprehensive information on many aspects of body structure and function, but the information will not automatically lead to clear decisions about how intervention should be targeted. For example, it may be clear that the client has an organic contracture in his elbow flexors and reduced tactile sensation and weakness in his wrist extensors, but which of the identified impairment factors should be prioritised for intervention, and for what purpose, is not immediately evident.
Two additional components of body structure and function assessment have become more common in some clinical settings: assessment of positive and negative features [46, 47] (see Section 2.4) and analysis of movement patterns. Although common patterns of movement and positioning after brain injury have been identified (see Section 2.5.1), clinicians acknowledge that because “every person’s different” [4, p.24] there is a need to identify the specific contributors to each individual’s performance. Accordingly, movement analysis is a valuable tool for assessing individualised patterns. For example, Levin et al. [48] developed a scale for rating motor compensations used by people with stroke when reaching. Analysis of positive and negative features and movement patterns goes some way towards identifying performance contributors, but will be limited if this information is gathered in isolation from task performance. Jaspers et al. [49] reviewed quantitative movement analysis studies conducted with children with hemiplegic cerebral palsy and concluded that standardisation of a three-dimensional movement analysis protocol that uses functionally relevant upper limb tasks was needed to provide a complete assessment picture.
While positive and negative features and movement analysis might be more obviously connected with task performance, other impairment factors, such as ROM, spasticity and strength also need to be considered in relation to their effect on task performance [6, 12]. It is only by individualising assessment of body structure and function impairments, and linking these impairment factors to activity (and ultimately, to participation) that the clinician can understand why activity limitations exist and identify priorities for intervention at each level of the ICF to optimise activity and participation outcomes.
4.2.4 Linking assessment information between body function and structure, activity and participation levels
Once the clinician has an understanding of how specific impairments are contributing to activity performance limitations, intervention decisions can be made that target those specific impairments [50]. Although the clinician is likely to address activity performance to some extent through task practice, aiming intervention partly at the activity level and partly at impairment factors may potentially address performance across a range of different activities that require control of the same movement or position, that is, it may generalise performance benefits across activities [13]. For example, if the client is having difficulty using a spoon, assessment of impairment level factors together with task analysis may indicate that wrist flexion contracture and supinator muscle weakness are contributing to difficulties maintaining a reliable grasp on the spoon and turning it to successfully place food in the mouth. Intervention to reduce the wrist flexion contracture, to assist in maintaining the wrist in a less flexed position during activity and to strengthen or facilitate supination, together with simulated or real life task practice, may improve this skill; it may also assist the client’s performance of other tasks that require the same type of movement, for example, brushing the teeth or hair.
While task analysis is not new to rehabilitation [51–53] and can be performed through informal clinical observation of daily tasks, linking the impairment factors with the task performance may require a more structured process (see Box 4.4). While three-dimensional movement analysis has potential for accurately identifying the contributors to adapted movement patterns used by clients, further work is required to standardise this process [49]. It is also likely to be some time before the resources for 3D movement analysis are available in most clinical settings. The Comparative Analysis of Performance—Motor (CAP-M) is an observational tool that can more easily be used for identifying movement limitations during activity performance. The CAP-M is a component of the Upper Limb Performance Analysis tool [7] which involves analysing a client-chosen task by systematically identifying impairment-level missing or excessive muscle activity that is impacting on task performance (the terms “missing” and “excessive” muscle activity in the CAP-M equate to positive and negative features as described in Section 4.3.2). The client is visually recorded while performing the relevant task, and the recording is then used to complete the CAP-M assessment (Appendix 4.B) by describing the position and movement of each upper limb joint during task completion.
Although the CAP-M was originally designed for use with adults post-stroke [54], its utility for assessing children with cerebral palsy has also been demonstrated [6]. Clinicians reported that use of the CAP-M with children facilitated more explicit observation and analysis of movement and positioning during the performance of meaningful tasks than other existing assessment tools. This analysis, in turn, allowed clinicians to pinpoint the specific joint movements and upper limb positions that needed changing in order to improve task performance, leading directly to the establishment of clear clinical aims (see Box 3.2) and a selection of interventions to achieve those aims. Only two other activity performance measures have been identified for use with more than one client population, the COPM and GAS, both of which measure perceived rather than actual performance [3]. The CAP-M shares the advantage of these tools in reflecting improved performance of activities that are meaningful to the client, with the added benefit of leading the clinician to intervention aims and options.
Whether using the CAP-M or an informal process of movement analysis during task performance, linking impairment factors to activity performance can facilitate the clinician to identify clinical aims for upper limb function or status that directly connect to the achievement of a daily-life goal. For example, a client’s daily-life goal may be “to safely clear the dinner plate(s) from the table each night”.
The clinical aims that link upper limb function to this goal might include achieving:
- active forearm supination to mid-position
- a lateral pinch grasp
- and sufficient grasp strength to transport the plate to the sink, as well as
- sufficient control of shoulder and elbow movement and effective release of grasp to place the plate in the sink or dishwasher.
A key characteristic of identified clinical aims is that they specify achievement of certain movements or abilities only to the extent required for successful task performance, rather than to the “normal” level of function expected of people without neurological injuries. These specifications help the clinician and client to clarify what they expect from the intervention and to judge when the intervention has been successful.
4.3 Upper limb assessment
4.3.1 Individualised assessment
Given the wide variation in upper limb presentation among people with neurological injury, it is unlikely that exactly the same assessment information is required for every client. For example, there may be no need to measure PROM in all upper limb joints if initial observation of the client’s resting position suggests that full ROM exists in some joints. If early observation and discussion with the client about the extent of voluntary movement indicates gross control of hand function, then administering a fine motor assessment involving grasp of small pegs will be unlikely to give useful information, and may inadvertently frustrate the client.
Consideration of the client’s overall functional status, potential for upper limb movement and daily-life goals can also guide assessment. For example, for a person with upper limb function described by HIPM 3 (Table 3.2) whose caregivers indicate lack of voluntary movement, and for whom ROM assessment indicates significant upper limb contractures, assessment of two-point discrimination may not be a priority. However, assessment of general pain and temperature perception may be important to determine whether certain intervention options, such as casting or surgery, can be safely pursued to reposition the person’s limbs to assist with daily care.
Given these variations in assessment process for each client, it is recommended that specific questions to the person or caregivers, together with careful observation of the resting position of the limb, and initial investigation of available voluntary movement are used to guide the clinician towards further information that needs to be gathered. This process of individualising assessment of upper limb impairments is described here (Section 4.3) and in Chapter 5. Having a flexible assessment format that provides an overall structure, but that can be tailored to each client, will prompt the clinician to use systematic clinical reasoning to identify an individualised assessment process (see Appendix 4.C).
4.3.2 Positive and negative features
One of the first assessment tasks is to identify the positive and negative features influencing the person’s upper limb. As discussed in Chapter 2 (see Section 2.4), positive features of the upper motor neuron syndrome (UMNS) include excesses or exaggerations of movement, such as hypertonicity (including stiffness, spasticity and clonus) and stereotyped movement patterns. In other words, positive features present as too much of a particular movement or position in relation to the usual demands of a task, or to the typical resting position of the upper limb. Negative features include movement deficits, such as missing movements, slowness of movement, fatigability, loss of dexterity, loss of arches of the hand or joint instability. That is, not enough of a particular movement or position that is required for usual task demands or for a comfortable resting position.
The presence of positive and negative features of the UMNS is often identifiable at rest and can be observed by the clinician whilst conducting the initial interview. For example, the client may display posturing at rest due to hypertonicity in some muscle groups or structural changes at some joints. As a general rule, persistent flexion of joints against gravity (e.g. elbow flexion when sitting upright) indicates a positive feature. Flexion or extension of joints in a gravity-assisted position may indicate either a positive or a negative feature (e.g. wrist flexion when seated upright may be due to hypertonicity in the wrist flexor muscles or paralysis in the wrist extensor muscles). Hyperextension of a joint, such as hyperextension of the finger metacarpophalangeal (MCP) joints, indicates a negative feature in the muscles opposing the hyperextension (e.g. in the lumbricales, which typically facilitate finger MCP flexion and IP extension). For some clients, positive and negative features are not apparent at rest and can only be identified by observing movement patterns (see Section 4.3.2). Figure 4.3 illustrates some examples of positive and negative features. For some clients, positive features can be divided into primary and secondary features (see Box 4.5).
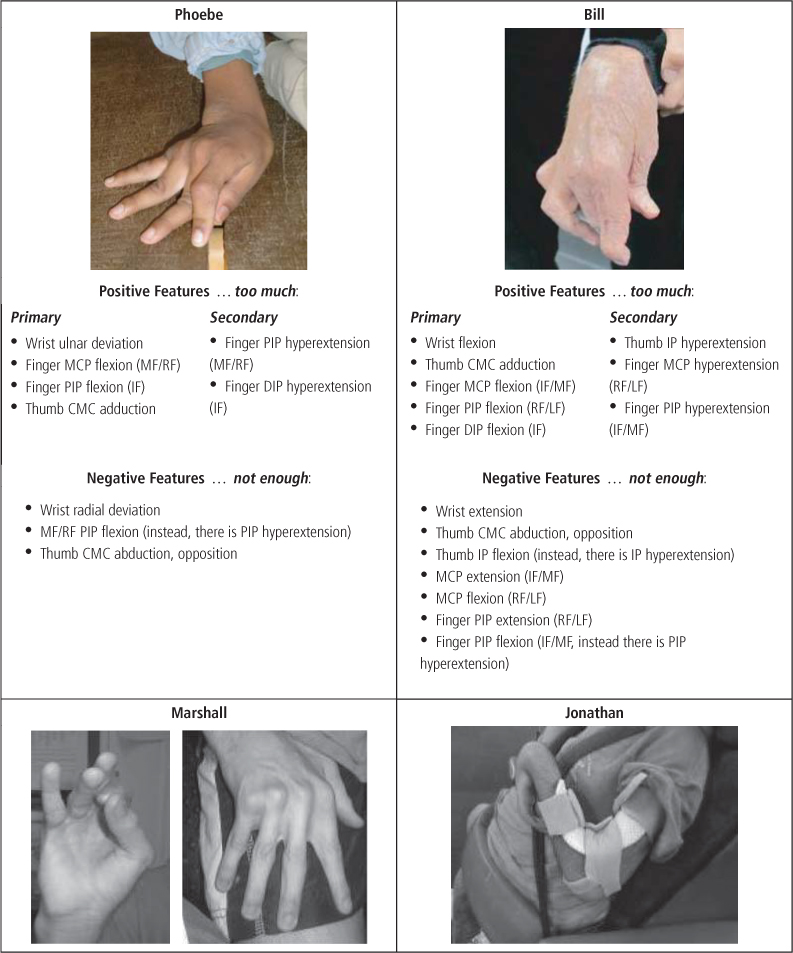
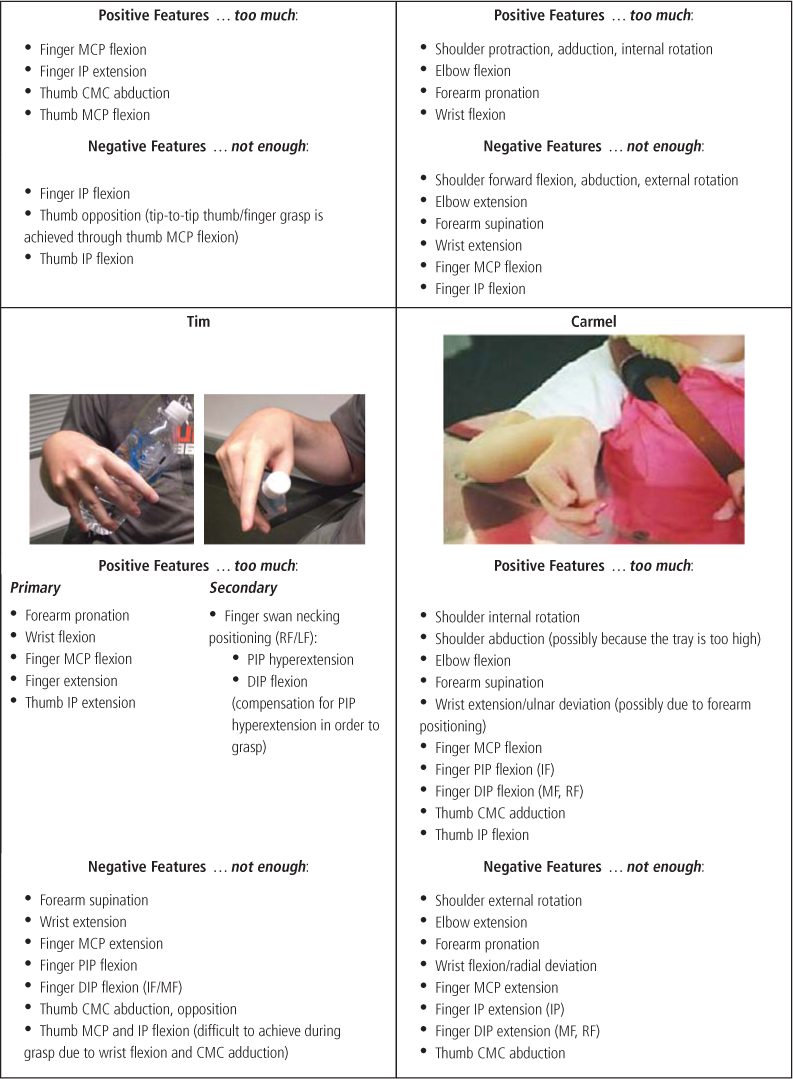
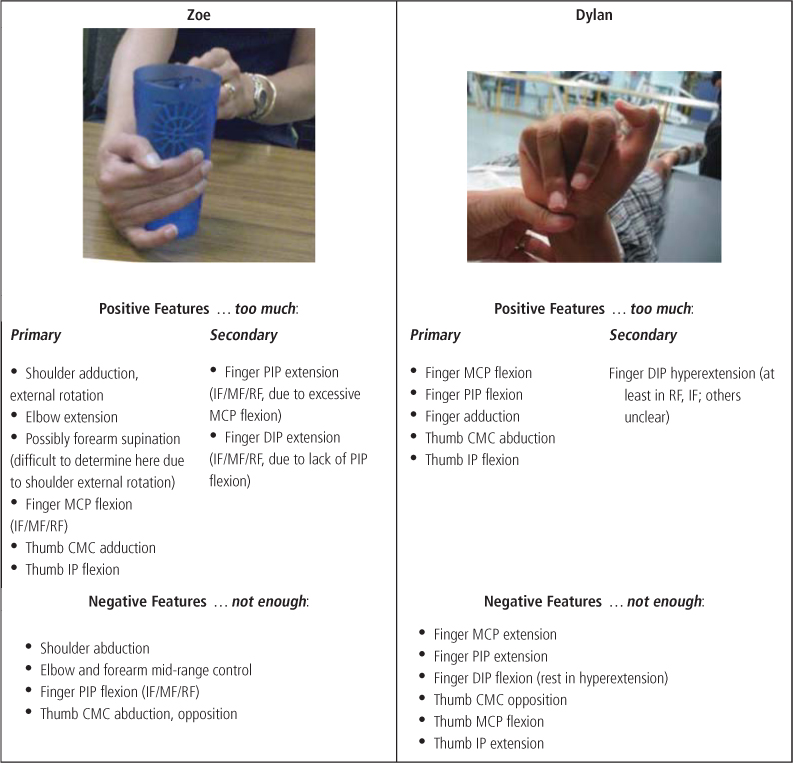
Figure 4.3 Positive and negative UMNS features affecting the upper limb after brain injury.
4.3.3 Active range of motion and movement patterns
4.3.3.1 Determining what to measure and observe
In general, the initial interview conducted with the client should include questions about daily-life activities that give some indication of the types of activities the client is involved in (self-care, school/work and productivity, leisure) and the degree of participation in those activities. That is, questions about which parts of the task the person can complete independently, with supervision, or with full assistance. For example, in relation to dressing, probing questions might be used to establish whether the client is able to reach and grasp the clothing, push her arm through the sleeve, and so on. The starting point for these questions can be informed by the client’s initial presentation; if the client appears to have a dense hemiplegia with severe malalignment of the joints at rest, questioning may start at a broader level, such as “Are you able to help in any way to get your shirt on?” If the client’s upper limb appears less affected and a greater amount of purposeful movement is observed questioning may start at a more specific point, for example, “So how do you manage with fastenings, like doing up your buttons?”
Even after the client’s performance and participation in daily-life tasks is discussed, direct questioning about available movement and control of movement patterns may still be required. This is because the client and caregivers will often have developed a day to day routine that, due to practical considerations such as time constraints and the effort involved, does not always use the client’s movement control as optimally as possible. For example, a parent may say that “dressing is fine” but not clarify specifically what the child can do, or a client may say “I can’t do anything with that arm, its useless!”, but is then able to demonstrate some movement control at various joints (indicating that his statement was, in fact, conveying the sentiment that “My arm won’t do what it used to do/what I want it to do”).
Direct questions to establish the client’s movement control need to begin broadly but are then shaped to systematically determine the specific movements and functions available. The importance of establishing these specific movements and functions becomes clearer at the point where the clinician needs to help the client set goals that reflect a realistic and achievable level of function (see Section 4.4.1). The initial request to “Show me how you can move your arm”, and consideration of the client’s response will indicate whether movement is proximal only, for example, generalised shoulder movement or shoulder shrug. The clinician can then check “Is there any movement at all in your hand/wrist/elbow?” If it is clear that no further voluntary movement exists, the clinician can focus on the client’s existing shoulder movement and establish whether more isolated control of shoulder flexion, abduction, internal or external rotation exists. If some movement appears possible in distal joints, the clinician can work through the process of measuring AROM at these joints. When completing this process, it will often be necessary to stabilise the limb just proximal to the joint to assist movement isolation, and to attempt the movement in various positions, including gravity assisted and gravity eliminated positions. For example, to measure active wrist extension, ask the client to attempt the movement with the forearm stabilised in pronation (wrist extension against gravity), mid-position (wrist extension, gravity eliminated) and supination (wrist extension, gravity assisted) if needed.
The main points to recognise about this process are that:
- Clinically it is not always necessary to measure AROM in every joint of the limb if it is established early in the process where movement exists and where it does not (research protocols may demand that all joints be measured).
- It is rarely necessary to measure all directions of movement at each joint (flexion, extension, abduction, adduction, etc.). The movements that are measured are informed by observation of the positive and negative features influencing the client’s initial positioning. For example, if the client is posturing in significant elbow or wrist flexion (a positive feature), only elbow or wrist extension (the consequent negative feature) needs to be measured; if the client’s thumb postures in adduction from the CMC joint, abduction and opposition need to be measured.
- As a result of Points 1 and 2, relevant AROM measures may be different for each client in the clinical setting.
- The key information provided by taking AROM measures is whether weakness is evident in specific muscle groups. As a rule of thumb, if AROM at a joint is less than PROM, it is likely that weakness exists in the muscle groups responsible for the movement.
- As a result of Points 1 and 2, relevant AROM measures may be different for each client in the clinical setting.
In relation to the hand affected by hypertonicity, it is often unproductive to measure AROM at each finger and thumb joint separately. Due to the action of the extrinsic finger flexor and extensor muscles across both the wrist and fingers, positioning of finger joints is likely to be affected by wrist position. Similarly, the position of proximal thumb joints will influence more distal ones. It is, therefore, often most useful to observe reach, grasp, manipulation and release patterns in the context of daily-life tasks. Taking into consideration the information gained at the initial interview regarding the client’s involvement in daily tasks, the clinician can ask “Show me how you can grasp and use …” (presenting an item that is the same as, or approximates, the item discussed, e.g. a washcloth, a television remote control, a fork, a pencil, a toy). Observing the person using such items gives the clinician information about:
- The client’s ability to orient and position the hand using shoulder/elbow/forearm and/or wrist movement to approach and grasp the object, and whether difficulties with this result in awkward or effortful positioning and movement, or in an inability to reach the item without it being positioned close enough to the hand or in a specific orientation to allow grasp.
- The ease with which the client can open the hand for grasp and release, and the position of the wrist during grasp. Observe whether this can be achieved with the wrist in a neutral or slightly extended position (the latter facilitates strength and reliability of some types of grasp), or whether some degree of wrist flexion is required to enable finger extension (using a tenodesis action, where flexion at the wrist allows sufficient excursion in contracted or hypertonic extrinsic finger flexor muscles for finger opening. See Figure 4.4). If wrist flexion is consistently used to allow finger extension, a baseline active ROM measure can be taken of wrist position during this movement, since a change in wrist position (for example, increased wrist extension during grasp) is likely to be a clinical aim of intervention in order to achieve a more efficient grasp. If finger opening is difficult, determine whether the client uses the affected hand for grasp by placing items in the hand using the less-affected hand. If so, establish if the person does this due to the effort required for finger extension, but can actively extend the fingers if necessary; or whether the object is only maintained in the hand due to spasticity/hypertonicity in the finger flexor muscles.
- Type of grasp the client can achieve and whether this is appropriate to the object. For example, does the client use a whole hand grasp to pick up a water bottle? Can he appropriately use a digital grasp with thumb opposed, a lateral pinch, a pincer grasp, and so on? (see Table 2.4).
- Adaptations to the expected grasp. For example, is the client grasping a water bottle with the fingertips (due to increased flexion of the finger MCPs and inadequate flexion of the PIPs) and thumb adduction, resulting in difficulty securing a firm hold on the item? (see Tim, Figure 4.3) Is she using a lateral pinch on a clothes peg or puzzle piece because she cannot achieve thumb–finger opposition? Can the client achieve a digital grasp but not maintain it due to reduced control of finger pressure or increased flexion of finger joints over time? (see Figure 5.5)
- Adaptations to the expected transport or manipulation of the object. For example, does the client use forward trunk flexion to reach the plate with his fork due to limited active shoulder flexion? Is it difficult for the client to use an eraser due to limited control of forearm positioning to orientate the eraser in relation to the page and limited control of wrist movement to make the alternating movements required to rub out pencil marks?
- Whether these adaptations adversely affect task achievement. For example, is placement of the clothes peg more effortful and inaccurate due to lack of thumb opposition or forearm pronation? Is the client’s grasp on the water bottle less reliable, requiring frequent adjustment? Does the client rip his page when trying to erase his work?
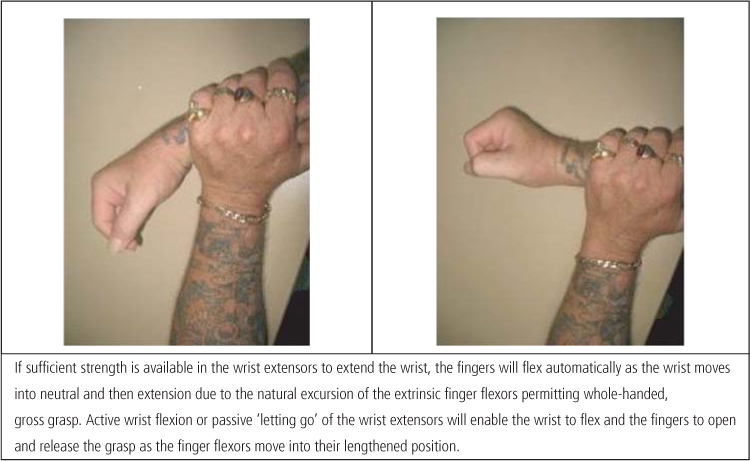
Figure 4.4 Tenodesis action on the wrist and fingers.
4.3.3.2 Describing movement patterns
As advocated in the CAP-M [7], describing a person’s patterns of reach, grasp and manipulation is often a comparative process. That is, the clinician has an initial awareness of the usual positioning, type and extent of movement at each joint that is most efficient to achieve the task. Observation of the client’s task performance is compared with the expected pattern in order to identify missing and excessive movements. It is essential, then, that the clinician continues to develop a mental ‘blueprint’ of patterns of movement expected to occur within various daily tasks (with the understanding, of course, that there may be more than one way of completing the task efficiently). Given that people may partake in an endless array of personally meaningful tasks (from playing lawn bowls, to accessing a communication device, to dressing dolls), the clinician may regularly be performing a mini-task analysis on ‘typical task completion’ in the absence of upper limb impairments, and using a process of constant comparison to detect differences between this and the client’s performance. As a basis for task analysis, a working knowledge of the usual resting and functional positions of the hand, structural arches that shape the hand, normal patterns of prehension and the functional anatomy of the upper limb (including joint and muscle names) is required; such information is widely documented in the literature (see Chapters 2 and 7) [55].
Detailed documentation (and/or visual recording) of reach, grasp and manipulation patterns during performance of the client’s current and desired daily tasks not only leads the clinician to the specific aspects of upper limb positioning and movement control that need to be targeted to address task performance, but also provides a baseline for measuring change at the activity level. Evaluating change using thick description of movement patterns provides a more sensitive measure of change in upper limb performance than most assessment tools such as the MACS and the Motor Assessment Scale. As described in Section 4.2.2, these tools use broad categories of upper limb performance or capacity, such as “handles most objects but with somewhat reduced quality and/or speed”, [44] or evaluate the ability to complete a pre-determined task, for example “take a dessert spoon of liquid to the mouth” [38] without detecting change in particular activity components. Observation of, and feedback regarding, smaller, incremental changes in a person’s task performance may help maintain motivation to persist with an intervention. It may also be useful for the clinician to identify such change to evaluate whether specific interventions are worth continuing or require adaptation.
Standard patterns of movement and positioning of the upper limb have been described in the literature and can assist the clinician to document movement analysis in a manner that facilitates communication among team members and over time (see Section 2.5). For example, five upper limb spasticity patterns that are commonly encountered post-stroke have been identified [56]. Similarly, hand [57] and thumb [58] patterns that are typically experienced by people with cerebral palsy have been described.
4.3.3.3 Analysis of muscle and joint dynamics: blocking and supporting joints
While using standard classifications of common hand and thumb patterns is useful to assist observational analysis, they do not describe all patterns of movement seen in clients with brain injury. In particular, they do not capture the dynamic adaptive or compensatory movement patterns that clients may develop over time to achieve a task in the presence of missing or excessive movement components or joint malalignment. For example, if a client has difficulty extending the fingers at the PIP and DIP joints, she may instead hyperextend the MCP joints in an effort to open the hand for grasp. If there is co-existing weakness in the lumbricales (which flex the MCP joints) then, over time, the MCPs may habitually posture in a hyperextended position (see Figure 4.5), resulting in ‘intrinsic minus’ hand posturing which causes difficulty achieving grasp since active MCP flexion is not possible (see also Sections 2.5.1.1 and 2.5.1.3). Similarly, if a person has limited ability to actively flex the wrist or pronate the forearm, he is likely to use excessive shoulder abduction and internal rotation to orientate the hand to grasp items from a work surface, and without control of thumb opposition or IP flexion, thumb adduction against the side of the index finger (a lateral pinch grasp) may be the only grasp option.
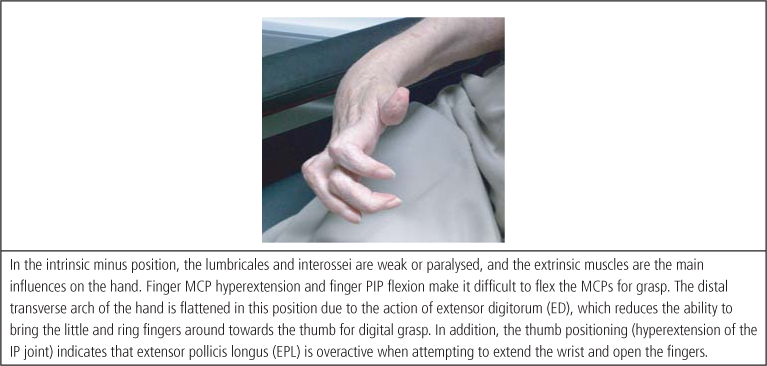
Figure 4.5 Common ‘intrinsic minus’ hand pattern.
The challenge for clinicians, when observing movement patterns, is to determine whether a joint position or movement is due either to hypertonicity or weakness in specific muscle groups (causing excessive or missing movements), or whether it occurs in compensation for excessive and missing movements. In other words, is the movement pattern a primary or a secondary problem? Analysis of muscle/joint dynamics can be used to refer to the process in which the clinician holds relevant joints, immobilising them and providing external stabilisation while the client undertakes an activity. Positioning the hand or arm in this way assists the clinician to distinguish the muscle groups in which hypertonicity or weakness exist, and which may be impacting the movement patterns used by the person. It also provides information about whether blocking excessive or supporting missing components make a constructive difference to the movement patterns being used. The process of blocking and supporting (see Box 4.6) can help predict whether intervention that addresses joint positioning, immobilisation and/or stabilisation (through interventions such as strengthening, taping, splinting, casting or surgery) will assist the client to develop more control of isolated movements and coordinated patterns of reach, grasp and manipulation.









