Fig. 9.1
Atlantoaxial instability and basilar invagination. (a) Atlantoaxial instability is determined by the atlantodens interval (ADI) and the space available for cord (SAC) (b): basioccipital hypoplasia associated with Chiari I malformation. There is a protrusion of the dens’s tip above McGregor’s line (this line is drawn from the hard palate to the base of the occipital bone), so-called basilar invagination with impression on the brainstem. Wackenheim’s clivus baseline (which should fall tangent to the dorsal surface of the odontoid process) falls too posterior, compatible with a posterior craniocervical dislocation
Normal physiological displacement can be found in children at the level of C2–C3 and to a smaller degree at the level of C3–C4 up to 7 years of age. In addition, dentocentral synchondrosis (visible up to 11 years of age) and ossiculum terminale (appears after 5, mostly after 8 years of age) may be confused with odontoid tip fracture. Be aware that normal wedging of the C3 is seen in 7 % of younger children.
Cervical instability is frequently discovered incidentally in an asymptomatic patient
CCJ anomalies, in particular congenital atlantoaxial dislocation, can be missed in children if not looked for.
If trauma is not present, rule out congenital anomaly, skeletal and metabolic dystrophy, as well as rheumatoid arthritis. Typical syndromes associated with CCJ anomalies are Klippel–Feil and Down syndromes, achondroplasia, mucopolysaccharidoses, and osteogenesis imperfecta.
Patients with connective disorders should have an MRI around 6 years of age (spine is more fully ossified and modeling has happened).
Relative motion of more than 5 mm between anterior surface on the dens and the posterior aspect of the anterior ring of C1 indicates surgical intervention in children. This value is higher than the adults (3 mm).
In children, a distance of less than 13 mm between posterior surface of dens and anterior surface of the posterior arch of C1 is considered abnormal.
Basilar invagination is the protusion of dens tip more than 0.5 cm above McGregor’s line. It is typically caused by occipital bone anomalies and atlantooccipital non-segmentation.
Platibasia is the displacement of the upper cervical vertebrae with an increase of the basal angle, >150°.
Pseudo-“physiological subluxation” at the level of C2–C3 and to a smaller degree at the level of C3–C4 is normal findings up to 7 years of age.
In general, the best diagnostic clue in imaging (MRI and/or CT) for CCJ anomalies is the flattening or malformation of the clivus, anterior ring of C1, or odontoid process. Flexion–extension MRI is often necessary to fully evaluate the pathology.
Chen and Liu ( 2009) described a simplified classification for malformations of the CCJ, as follows:
Malformations of the occipital bone
Platybasia
Basilar invagination (basioccipital hypoplasia)
Condylar hypoplasia
Condylar dysplasia
Malformations of the atlas
Occipital atlas assimilation
Aplasia and hypoplasia of the atlas
Atlas arch anomaly
Malformations of the axis and odontoid process
Aplasia or hypoplasia of the dens
Persistent ossiculum terminale
Os odontoideum
Klippel–Feil anomaly
Instability associated with childhood diseases
(a)
Down syndrome
(b)
Neurofibromatosis
(c)
Juvenile rheumatoid arthritis
(d)
Mucopolysaccharidoses
(e)
Achondroplasia
(f)
Osteogenesis imperfecta
(g)
Spondyloepiphyseal dysplasia
(h)
Larsen syndrome
(i)
Others
9.2.1 Malformations of the Occipital Bone
Platybasia Displacement of the upper cervical vertebrae with an increase of the basal angle (normal <150°) Basilar invagination Refers to the cranial displacement of the foramen magnum with radiological protusion of the dens tip more than 0.5 cm above McGregor’s line
The lower part of the clivus is formed by the basiocciput, and malformations of the occipital bone, such as basioccipital hypoplasia (Fig. 9.1b), can cause platybasia, basilar invagination (upward migration of the cervical spine into the foramen magnum), condylar hypoplasia, and condylar dysplasia. Platybasia can cause bony impingement on the brainstem (Fig. 9.1b) and obstructive hydrocephalus if it is associated with basilar invagination. Basilar invagination is associated with not only platybasia but also occipitalization of C1, fused upper vertebrae, Klippel–Feil syndrome, Chiari malformation (Fig. 9.1b), and skeletal dysplasias, mainly achondroplasia. In children, due to the greater laxity of the cervical spinal ligaments, basilar invagination can be attributable to trauma or bone softening (Fig. 9.2), as, for example, in rheumatoid arthritis. Other diseases with potential risk for basilar invagination are osteoporosis, hyperparathyroidism, osteomalacia, rickets, renal osteodystrophy, and Hurler syndrome.
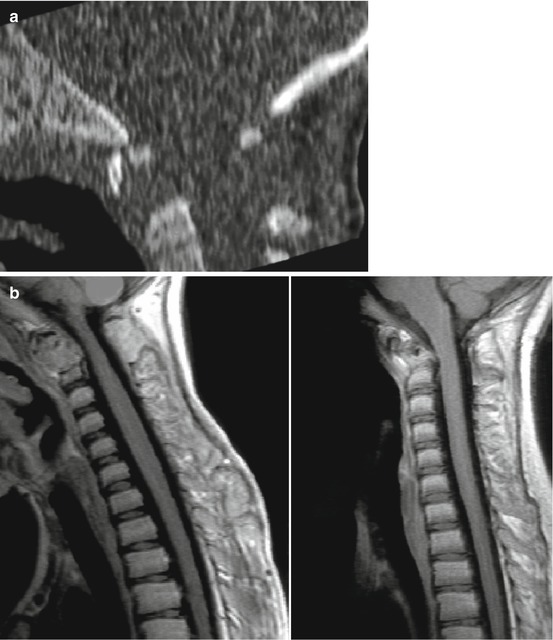
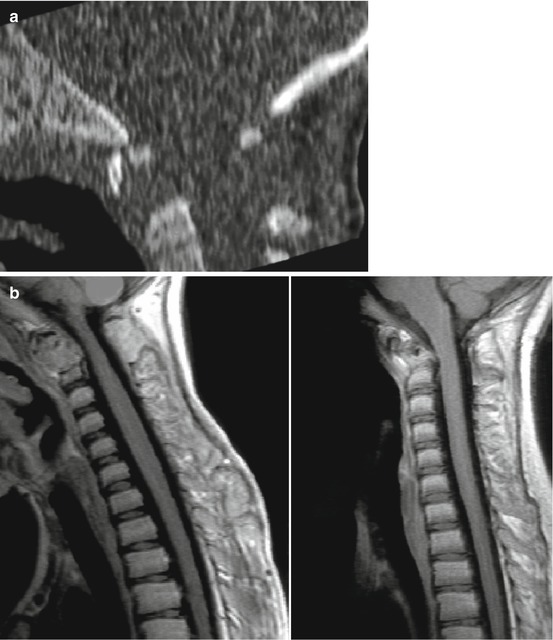
Fig. 9.2
Farber disease, a very rare lysosomal storage disease due to defective ceramidase causing accumulation of lipids leading to abnormalities in the joints, liver, throat, tissues, and central nervous system. (a) Sagittal CT shows a soft tissue mass eroding much of the dens axis (C2) pre-transplant. (b) T1-w after contrast before (left image) and after (right image) bone marrow transplantation. There is a large soft tissue mass (C2 level) which extends into the spinal canal. Note the skin nodules over spinous processes pre-transplant. Right image: clear improvement after therapy
Wackenheim’s clivus baseline is useful for assessment of cervical instability in children with Down’s syndrome and also in the assessment of traumatic injuries. It runs from the posterior surface of the clivus and normally is tangential to the posterior margin of the dens. If the line falls far of the posterior limits of the odontoid, a posterior dislocation is present. If the line intersects the anterior or middle body or the base of the odontoid, an anterior dislocation is diagnosed (Fig. 9.3).
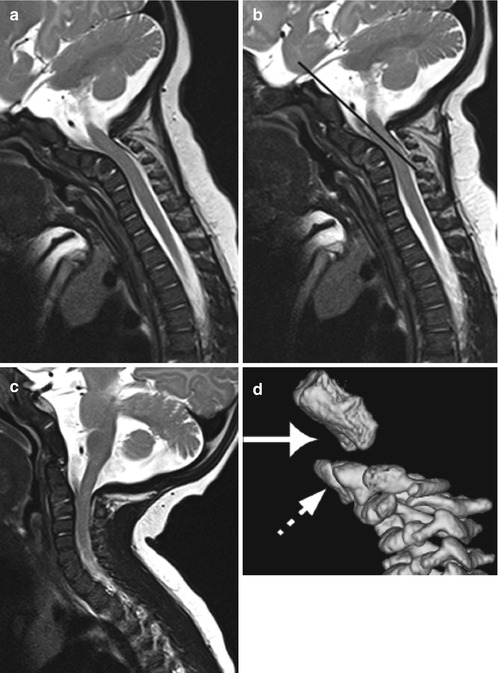
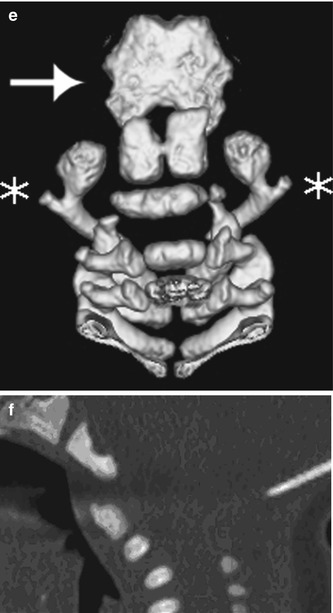
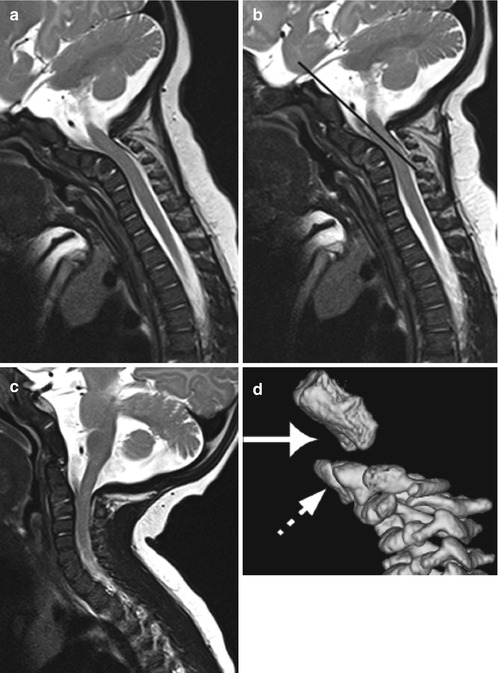
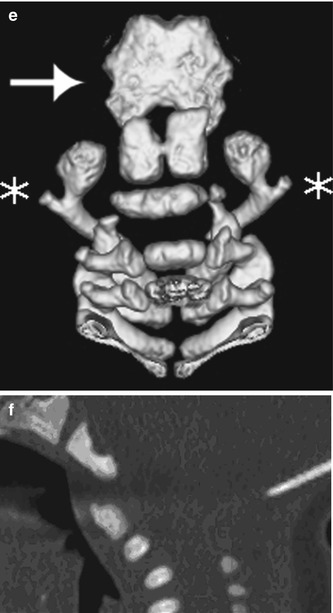
Fig. 9.3
Newborn child with incidental finding: atlantodental occipital subluxation. (a) Midsagittal T2-w MRI in flexion. The MR image best reveals the narrow spinal canal with compression of the spinal cord at the C1–C2 level, especially in anteflexion. (b) Midsagittal T2-w image in neutral position. The Wackenheim’s clivus baseline intersects the body of the odontoid, well matched with an anterior craniocervical dislocation. (c) Midsagittal T2-w image in extension. Note that the narrowing of the spinal canal at the C1 level in flexion and neutral positions reduces in extension. (d) The CT scan with 3D sagittal reconstruction at the time of presentation showed an anterior displacement of unfused dens (dotted arrow) relative to the occipital condyles (straight arrow). Note the two separate ossification centers of the odontoid, so-called bifidus; normally the ossification centers fuse by the 7th fetal month. (e) CT scan with 3D coronal reconstruction. The neural arch is present (star) but unfused posteriorly. (f) CT scan with sagittal reconstruction. Notably, the anterior arch is not ossified in this child, which is the case in 80 % of the newborns. Besides, no unification of the posterior synchondrosis of the spinous processes is seen, which is also normal for a newborn. Therefore, during the newborn period, it is difficult to evaluate malformations, such as atlas hypoplasia, or more specifically hypoplasia of a non-united posterior arch, due to the lack of ossification, presence of synchondroses, and variants. As a differential diagnosis, one should include traumatic delivery. A control evaluation at 3 years of age is necessary
9.2.2 Malformations of the Atlas
Due to failures of chondrogenesis, the majority of atlas anomalies are posterior arch anomalies.
Rachischisis: Cleft of the posterior arch located in the midline, found in ca. 4 % of autopsies and in 70 % of children with myelomeningoceles
In children, the knowledge of atlas ossification centers is essential to the diagnosis of clefts, aplasias, and hypoplasias. The atlas has three ossifications sites: its anterior arch and the two neural arches. The anterior arch is ossified at birth in 20 % of children only. Usually, it becomes visible as an ossification center by 1 year of age (varying between 6 months and 2 years). During the 7th fetal week, the neural arches appear. The posterior synchondrosis of the spinous processes unites by 4–6 years of age. The complete fusion of the anterior and neural arches (neurocentral synchondrosis) does not happen before 7 years of age.
Clefts of the atlas arches are more frequent, compared to arch aplasia and hypoplasia. The greatest part of posterior arch clefts is located in the midline (rachischisis). In contrast, anterior arch rachischisis is exceptional, only found in 0.1 % of autopsies. Importantly, clefts of the anterior arch may be a sign of dysraphic anomaly of the meninges and spinal cord. Even though most of the atlas’s clefts are incidental findings, its presence may be associated with other malformations of the spine, and more importantly, large clefts with fibrous tissue may present with atlas instability.
Occipital assimilation of the atlas results from a segmentation failure between the skull and the first cervical vertebra, also known as occipitalization of the atlas. The assimilation may involve the anterior arch only, the posterior arch, or both combined. This anomaly is reported as the most common anomaly involving the CCJ, encountered in 0.14–0.25 % of the population. It is always linked to basilar invagination, and there is an increased association to Klippel–Feil anomaly in C1 and C2. In this constellation, atlantoaxial subluxation and dislocation may occur. In an excellent overview, Smoker et al. describe that with the exception of the previously described atlantooccipital assimilation, most of atlas anomalies, when isolated, are not associated with abnormalities of the CCJ.
Half-sided pathology of C1 varies from hypoplasia of the lateral mass, up to complete agenesis of the hemiatlas with rotatory instability and basilar impression. In two-thirds of the patients, symptoms are present at birth; others show torticollis later. Partial hemiaplasias may simulate fractures on RXs.
9.2.3 Malformations of the Axis and Odontoid Process
The axis is formed by four ossification centers: one for the odontoid process, one for the body, and two for the neural arches. The odontoid process is formed in utero from two separate ossification centers which fuse by the seventh fetal month (Fig. 9.3d). The body of the axis fuses with the odontoid process around 3–6 years of age. Between 3 and 6 years of age, a secondary ossification center appears at the apex of the odontoid process (os terminale), and fusion of the os terminale with the odontoid process is completed by the age of 12 years.
By 2–3 years of age, the neural arches fuse posteriorly; their fusion to the body of the odontoid process happens between 3 and 6 years of age.
The most frequent congenital anomaly of the axis is malformation of its odontoid process, and this is not associated with basilar invagination. The malformations of the odontoid process range from mild hypoplasia to complete aplasia. In odontoid hypoplasia, a short odontoid process can be recognized. Complete aplasia is particularly uncommon. The presence of a hypoplastic odontoid can be associated with spondyloepiphyseal dysplasia, mucopolysaccharidoses, and metatropic dwarfism. In the rare case of hypoplasia or aplasia, there is a predisposition to atlantoaxial dislocation with cord compression due to the absence of the apical and alar ligaments. Secondary to the hypermobility, patients may present with pannus similar to that seen in rheumatoid arthritis. In addition, there is an association with metatropic dwarfism, spondyloepiphyseal dysplasia, and Morquio syndrome.
The ossiculum terminale at the tip of the dens appears between 5 and 8 years and fuses to the dens between 10 and 13 years. The failure of fusion of the terminal ossicle with the rest of the odontoid process is called persistent ossiculum terminale.
Os odontoideum
Independent osseous structure located cranially to the axis body with a gap between these two structures. Usually a small hypoplastic dens is present.
Persistent ossiculum terminale.
Failure of fusion of the terminal ossicle with the rest of the odontoid process.
When isolated, the persistent ossiculum terminale is a stable anomaly and of little clinical significance. In contrast, os odontoideum (Fig. 9.4) is associated with a number of congenital conditions, such as Down and Morquio syndromes, spondyloepiphyseal dysplasia, Klippel–Feil anomaly, and Laron syndrome. If the os odontoideum is associated with ligament weakness, patients present with atlantoaxial instability (Fig. 9.4) with compression of the spinal cord. The hypermobility at C1–C2 level may cause transient occlusion of the vertebral artery. Patients with a gap between the os odontoideum and the axis body should be carefully assessed with flexion and extension examinations (Fig. 9.4).
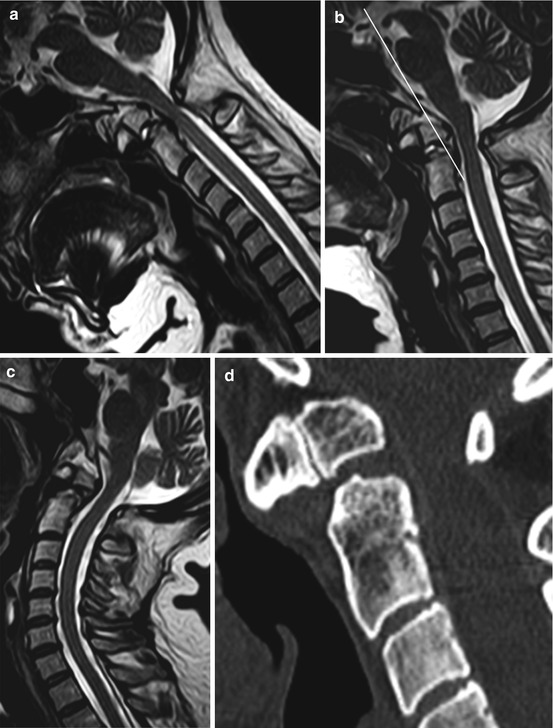
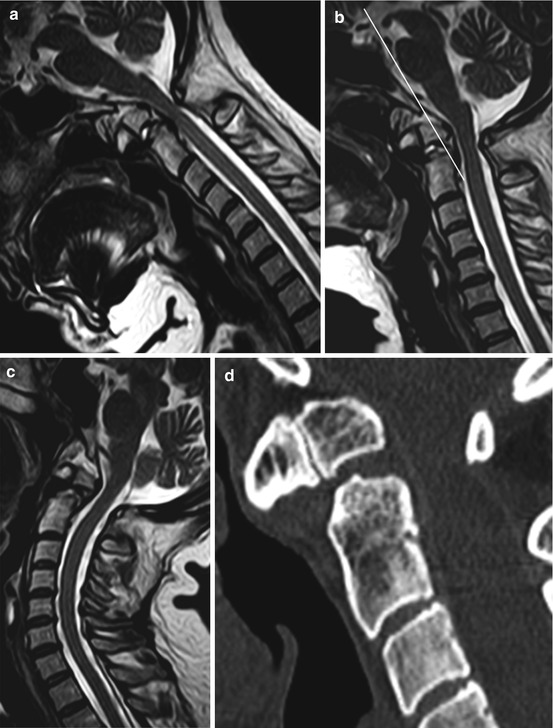
Fig. 9.4
Older patient with os odontoideum and atlantoaxial instability. (a) Midsagittal T2-w image in flexion. The MR image best shows the narrowing of the spinal canal with compression of the spinal cord at the C1–C2 level. (b) Midsagittal T2-w image in neutral position. The Wackenheim’s clivus baseline intersects the body of os odontoideum, compatible with an anterior craniocervical dislocation. (c) Midsagittal T2-w image in extension. The narrowing of the spinal canal at the C1 level in flexion positions reduces in extension. (d) The CT scan shows the os odontoideum as an independent osseous structure located cranially to the axis body with a gap between these two structures. Note the presence of small hypoplastic dens
Atlantoaxial rotatory subluxation (Fig. 9.5) in children occurs often after a minor trauma; other causes include surgery of the head and neck, following an infection or inflammation of the adjacent neck tissues. Consider anatomical variations in the differential diagnosis, i.e., children with normal atlantoaxial articulation fixed in a vicious rotatory position due to extreme torticollis (Fig. 9.6c). Clinically, children with rotatory subluxation present with new torticollis because of pain. Fortunately, most of the atlantoaxial subluxation resolves spontaneously. But, if an unresolved subluxation remains untreated, plagiocephaly may follow.
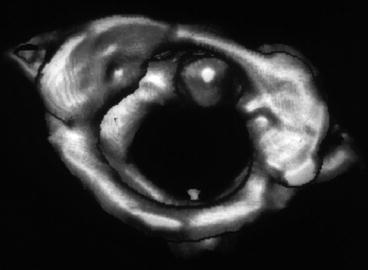
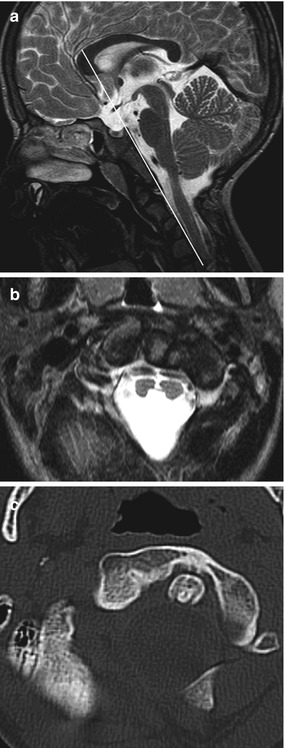
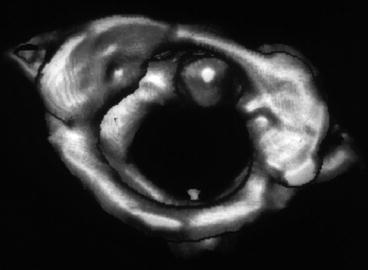
Fig. 9.5
Traumatic atlantoaxial rotatory luxation after a car accident. In children, the greater laxity of the cervical spinal ligaments results in more frequent high cervical cord injury
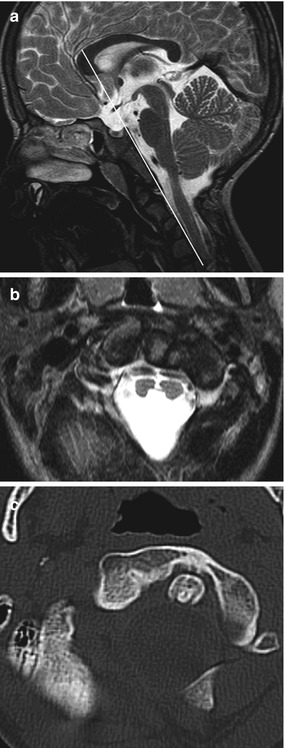
Fig. 9.6
Klippel–Feil syndrome associated with diastematomyelia. (a) Sagittal T2-w image shows multiple segmentation anomalies with congenital fusion. In this patient, there are associated anomalies of the atlas and odontoid process with instability of the CCJ. The Wackenheim’s clivus baseline falls far too posterior to the odontoid, compatible with a craniocervical dislocation. (b) Almost complete split of the cord into two hemicords within a single dural sac (type II diastematomyelia). No osseous or fibrous septum was seen. (c) In the CT images, note the vicious rotatory position of atlantoaxial articulation due to extreme torticollis in this patient with Klippel–Feil syndrome
Klippel–Feil syndrome (Fig. 9.6) is a rare condition characterized by the congenital fusion of any 2 of the 7 cervical vertebrae. It is the result of a failure of the vertebrae’s segmentation.
Be aware that fusion can be missed in infancy due to the incomplete ossification.
The patient usually presents with a short neck, low posterior hairline, and limited cervical motion.
Classification
Type 1 (9 %): Extensive cervical and thoracic segmentation anomalies
Type 2 (84 %): Fusion of 2 or more cervical vertebrae
Type 3 (7 %): Type 1 or 2 associated with lower thoracic/lumbar anomalies
Approximately 20 % of the patients have a complete or partial diastematomyelia (Fig. 9.6b). Other associated abnormalities may include basilar invagination, odontoid hypoplasia, atlantooccipital assimilation, platybasia, Chiari I, scoliosis, kyphosis, Sprengel’s deformity of the scapula with a bridging omovertebral bone, spina bifida, Dandy–Walker, malformations of the kidneys and the ribs, cleft palate, respiratory problems, and heart malformations. There is an increased likelihood for early instability of the CCJ in patients with atlantoaxial fusion or odontoid hypermobility associated with occipitalization of the atlas or with multiple fusion of the cervical vertebrae associated with anomalies of the atlas and odontoid process. It is important to look for instability, progressive degenerative changes, and brainstem compression.
9.2.4 Instability Associated with Representative Inherited Syndromes
9.2.4.1 Down Syndrome
In Down syndrome, a combination of osseous anomalies and lax ligaments contributes to C1–C2 instability. Patients usually present with hypoplasia of the dens without soft tissue dens mass. The prevalence of cervical instability has been estimated at 9–30 % in children with Down syndrome, although only 2.5 % of the patients present with symptomatic instability. This small group, however, has a higher prevalence of associated bone abnormalities, such as os odontoideum, persistent synchondrosis, or posterior rachischisis. As a general rule, children with Down syndrome show no major compression symptoms of the spinal cord. Patients usually present with slowly progressive neurological symptoms, which can eventually lead to a main injury.
Instability can be easily evaluated using Wackenheim’s clivus baseline. According to the literature, children with Down syndrome who have no C1–C2 instability will not develop a dangerous instability. Therefore, this group of patients will not need further screening after the age of 10 years. Be aware that this cutoff age can be controversial.
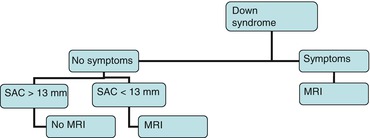
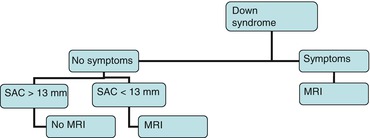
9.2.4.2 Neurofibromatosis
Neurofibromatosis can present with dystrophic changes in the vertebral bodies and dysplasia of vertebral bodies; abnormalities can also be secondary to pathological alignment. Furthermore, patients may present with focal or acute kyphoscoliosis. RX is important to quantify and to follow-up the scoliosis, while MRI is the ideal method to evaluate cord compression and nerve pathology in patients with severe cervical kyphosis. Although instability is rare, the strategy is similar as in the diagram above for Down’s syndrome.
9.2.4.3 Juvenile Rheumatoid Arthritis
Juvenile rheumatoid arthritis is an important differential diagnosis to CCJ variants and anomalies.
Rheumatoid arthritis (Fig. 9.7) is a systemic disease characterized by persistent synovitis, which can affect the joints of the cervical spine.
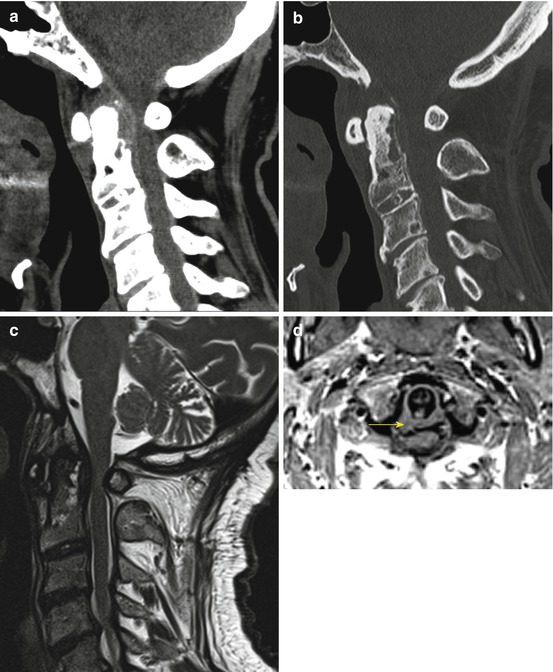
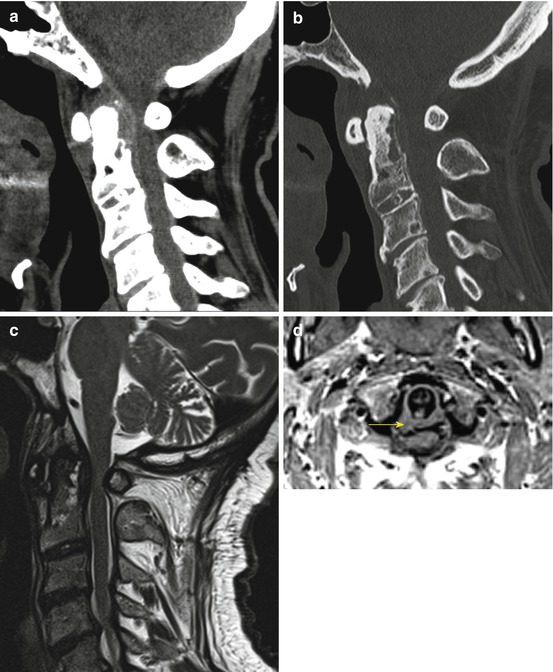
Fig. 9.7
Older patient with rheumatoid arthritis with cervical involvement. (a, b) Atlantoaxial joint CT in sagittal reformatted images: gross bone erosions of odontoid process and synovial joints, associated with joint instability (c, d) Sagittal T2-w and axial T1-w images, respectively, show the synovial pannus (yellow arrow) and cord compression by the odontoid process. MRI can assess the relationship of the occiput, atlas, and axis, and it is useful in depicting the extent of subluxation and the compression of the spinal cord
The incidence of cervical involvement ranges from around 40 to 80 % of cases, depending on the duration of the disease. Typically, the cervical spine is involved in the beginning of the disease and shows erosive synovitis, ligamentous subluxation, osteopenia, and vertebral fractures. Patients usually develop C1–C2 subluxation within 2 years of disease onset, and spontaneous clinical remission is uncommon.
Imaging
Patients usually present with enhancing “pannus” best seen on T1-w MRI (Fig. 9.7). C1–C2 subluxation is best seen with CT reconstructions. To evaluate instability, dynamic flexion–extension plain films or T2-w MRI are invaluable.
9.2.4.4 Mucopolysaccharidoses
Deformities of the spine are caused by deposits of glycosaminoglycans in the tissues surrounding the spinal cord, which can result in spinal cord compression. In the case of mucopolysaccharidosis IV, also called Morquio syndrome, the “os odontoideum” is invariably present; this is due to a partially cartilaginous dens. On top, the anterior ring of C1 can be unstable because of failure in the ossification process. All these components associated with pannus lead to C1–C2 instability classically described in Morquio syndrome. However, odontoid hypoplasia and associated soft tissue thickening have been shown to reverse after bone marrow transplantation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








