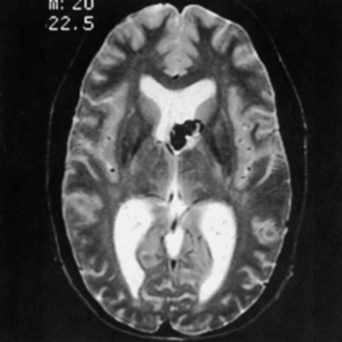
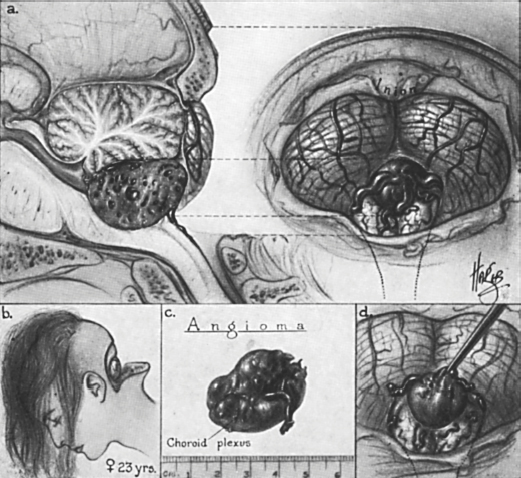
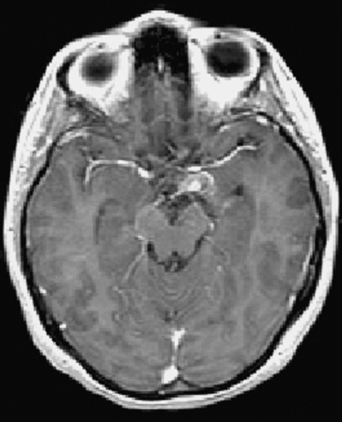
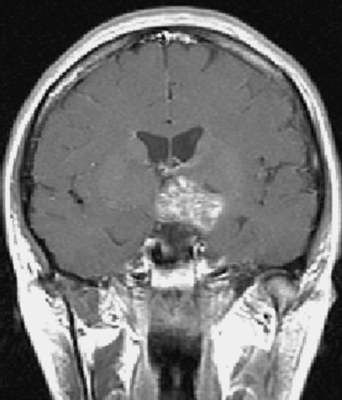
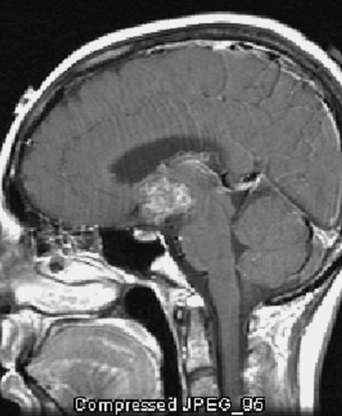
14 Vivek R. Deshmukh and Robert F. Spetzler Cavernous malformations are considered vascular malformations, a designation that they share with arteriovenous malformations, capillary telangiectasias, and venous malformations. Cavernous malformations are angiographically occult. Histologically, they appear as compact, thin-walled, dilated capillary spaces without intervening brain tissue. Their reported incidence is 0.3 to 0.5%.1–3 These lesions occur in sporadic and familial forms. Most are found in the supratentorial compartment (80%) followed by the infratentorial compartment (15%) and spinal cord (5%), a relative predilection that reflects the volumes of the central nervous system compartments. These lesions may become symptomatic with headache, hemorrhage, seizures, and progressive neurologic deficits. Atypical cavernous malformations are lesions located in atypical locations, including the ventricular system and extraaxial space. The latter can afflict the dura and cranial nerves traversing the subarachnoid space. These atypical cavernous malformations pose unique diagnostic and surgical challenges.4 The third ventricle is the most common location within the ventricular axis, followed closely by the lateral ventricles (Fig. 14-1). Fourth ventricular cavernous malformations are exceedingly rare. Patients usually exhibit symptoms related to mass effect. In the contemporary literature, 24 third ventricular cavernous malformations have been reported.5,6 There is a female predilection. Presenting symptoms may be the result of hydrocephalus or local mass effect. The onset of symptoms is usually insidious. It has been theorized that ventricular cavernous malformations undergo more rapid growth than cavernous malformations in other locations. Repeated extralesional microhemorrhages can cause superficial siderosis (hemosiderin deposition in subpial or subependymal lining). Suprachiasmatic lesions can cause field defects and endocrine disturbances. Those located at the foramen of Monro can cause hydrocephalus. Short-term memory loss in particular may result from third ventricular wall involvement. The floor of the third ventricle can be impinged, and hypothalamic dysfunction can be profound as a result.7,8 The fourth ventricle is the least common intraventricular location for cavernous malformations. Dandy first reported the excision of a fourth ventricular cavernous malformation in 1928 (Fig. 14-2).9 Symptoms in these patients are the result of cranial nerve dysfunction, obstructive hydrocephalus, and midline cerebellar deficits.10,11 Intraventricular cavernous malformations should be treated aggressively. The significant deficits that they cause and their rapid growth rate justify gross total resection. However, a solitary lesion that is clinically quiescent may be observed. The interhemispheric transcallosal approach can be used for lesions within the third and lateral ventricle. A transcortical route via the superior parietal lobule should be considered for lesions within the trigone. Septal and caudate nucleus lesions can be approached through either a transcortical or interhemispheric transcallosal approach. For these cases, the interhemispheric approach is preferred because it minimizes the amount of brain injury and offers an elegant corridor through noneloquent existing tissue planes. Fourth ventricular lesions can be excised through the suboccipital approach. Figure 14-1 T2-weighted magnetic resonance image shows a cavernous malformation involving the left caudate and thalamus. An exophytic portion extrudes into the left lateral ventricle. (From Deshmukh VR, Spetzler RF. Cavernous malformations of the brain and spinal cord. Operative Techniques in Neurosurgery 2002;5(3):167. Reprinted with permission from Elsevier, Inc.) Cavernous malformations involving the cranial nerves are extremely rare, but several case reports and series of cavernous malformations involving the optic nerve and chiasm, the vestibulocochlear nerve complex, oculomotor nerve, trigeminal nerve, and hypoglossal nerve have been reported. These lesions must be recognized in a timely manner and surgically excised if cranial nerve function is to be preserved. Twenty-three cases involving the optic pathways have been described.12–22 Most of these patients became symptomatic with acute chiasmal syndrome or chiasmal apoplexy. Sudden onset headache, visual deterioration, and signs of meningeal irritation characterize this apoplectic event. Typically, magnetic resonance imaging (MRI) shows a focal suprasellar lesion involving the optic pathways with heterogeneous signal intensity. A hyperintense signal suggests recent hemorrhage. If present at all, postcontrast enhancement should be minimal (Figs. 14-3, 14-4, and 14-5). This clinical scenario of acute visual deterioration represents a surgical emergency. Such patients should undergo emergent craniotomy and excision of the cavernous malformation. Figure 14-2 Illustration of the removal of a fourth ventricular cavernous malformation by Dr. Walter Dandy, the first such reported case. (Drawing from the Dorcas Hager Padget Collection, Brödel Archives, Department of Art as Applied to Medicine, Johns Hopkins University. Reprinted with permission from Johns Hopkins University.) Figure 14-3 Axial T1-weighted postcontrast magnetic resonance image shows a large cavernous malformation, within the left optic apparatus involving the surrounding structures. (From Deshmukh V, Albuquerque FC, Spetzler RF. Surgical management of atypical cavernous malformations. Operative Techniques in Neurosurgery 2002;5(3):168. Reprinted with permission from Elsevier, Inc.) Figure 14-4 Coronal T1-weighted image shows the rostral extent of this cavernous malformation, which originates within the optic apparatus. (From Deshmukh V, Albuquerque FC, Spetzler RF. Surgical management of atypical cavernous malformations. Operative Techniques in Neurosurgery 2002;5(3):168. Reprinted with permission from Elsevier, Inc.) The preferred surgical approach is a pterional craniotomy combined with an orbital roof and lateral wall osteotomy to obtain adequate exposure of the optic apparatus. An eyebrow key-hole craniotomy also has been used successfully.22 The optic apparatus will be edematous with evidence of hemosiderin staining (Figs. 14-6 and 14-7). Removal of the hematoma alone leads to significant decompression. The lesion must then be resected completely because residual cavernous malformation recurs and leads to progressive symptoms. The hemosiderin-stained tissue should not be resected because it is not part of the malformation; its resection would injure eloquent tissue (Fig. 14-8). Most patients’ preoperative symptoms or deficits improve after resection. Patients who have suffered multiple hemorrhagic events will have persistent deficits after surgery, and this possibility should be emphasized during preoperative counseling.
Management of Atypical Cavernous Malformations
 Intraventricular Cavernous Malformations
Intraventricular Cavernous Malformations
 Cranial Nerve Cavernous Malformations
Cranial Nerve Cavernous Malformations
Management of Atypical Cavernous Malformations
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree




