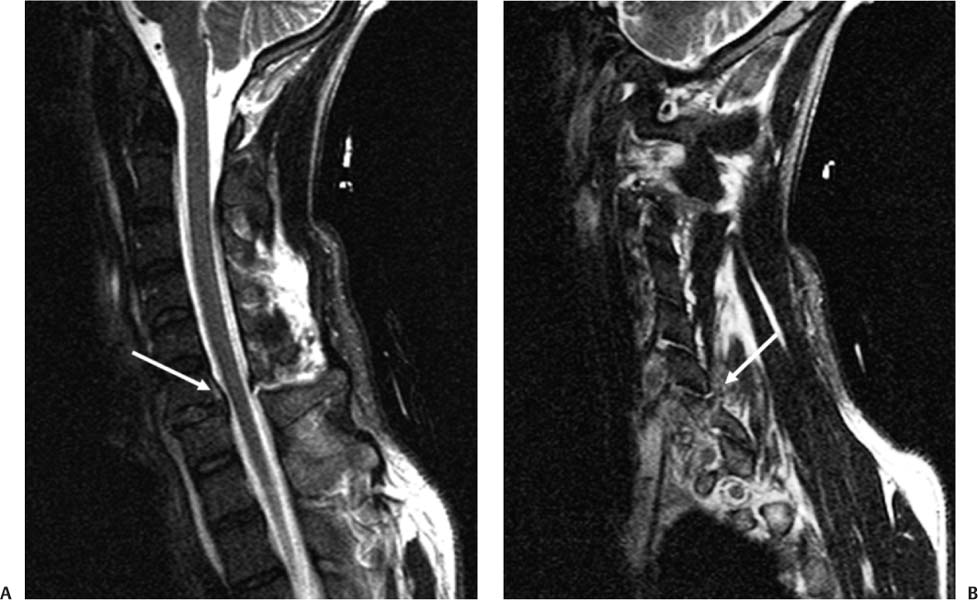
5 In the trauma population it has been reported that cervical spine injuries occur in up to 4% of patients, and this incidence increases to greater than 50% in the spinal cord injury population.1,2 The most common mechanism of injury is through flexion and flexion-rotation forces, which may result in cervical spine disk herniations, vertebral body fractures, dislocations, and subluxations.3 There is a higher incidence of cervical facet dislocation as a result of these forces, which has been attributed to the relatively smaller area of articular surface in the cervical spine.3 Facet dislocations occur as the result of the inferior facet translating over the superior articular surface and being ventral to the superior facet of the inferior vertebral body. Thus these facets are no longer opposed by nor do they have contact with the articular surfaces (Fig. 5.1). This displacement results in narrowing of the spinal canal and neuroforamina, and due to concurrent ligamentous injury there may be an associated disk herniation.4 Retrospective imaging studies have confirmed the presence of a disk herniation in up to 40% of facet dislocations of the cervical spine.4–7 However, presently no large-scale prospective study has been conducted to calculate this incidence.7 Fig. 5.1 (A) Sagittal T1-weighted postreduction magnetic resonance imaging demonstrating a traumatic herniated disk (white arrow) related to (B) unilateral cervical facet dislocation at C6–C7 (white arrow). The treatment of these cervical facet dislocations involves reduction of the deformity to anatomical alignment, through either an open or a closed technique. This reduction provides for the removal of bony compression on the spinal cord and exiting nerve roots. Closed reduction of cervical facet dislocations with axial traction using gradual increasing weights and Gardner-Wells traction has been widely reported with consistently successful results.8–12 In 2002 the American Association of Neurological Surgeons and Congress of Neurological Surgeons (AANS/CNS) performed a systematic evidence-based review of clinical series utilizing cervical traction that included more than 1200 patients.13 The incidence of permanent neurological complication was reported as less than 1% with a temporary neurological deficit rate of 1.7%.6,7,13–15 However, there has been a class III retrospective study insinuating that the presence of a herniated disk in a nonreduced cervical dislocation resulted in neurological decline upon cervical spine reduction due to worsening cord compromise.6 This relationship between postreduction neurological decline and the presence of a posttraumatic herniated inter-vertebral disk is not well established.16 Further, the need for magnetic resonance imaging (MRI) prior to closed reduction is an area of controversy.17 There is the argument that closed reduction without a prereduction MRI of the cervical spine places patients at low risk of neurological decline due to potential worsening cord compression based on anecdotal and retrospective data. However, the literature supports that in the awake, alert individual without distracting injuries, a closed reduction can be performed safely prior to imaging, and that indirect decompression through skeletal traction of the injured cord within the first few hours is beneficial for neurological recovery.17 The fundamental question that must be answered to recommend a treatment algorithm for facet dislocations is whether an MRI scan can identify patients at risk for neurological deterioration with closed reduction without delaying treatment. No randomized, controlled trial has been conducted on this topic, and the best answer must be inferred from existing literature addressing related questions. Questions addressing this issue include the following: (1) What is the incidence of disk herniation on prereduction versus postreduction MRI? (2) Does the presence of a herniated disk on postreduction MRI correlate with a worsening neurological outcome? A comprehensive review of the literature was performed to identify the best evidence available to answer these questions. A systematic review utilizing Medline, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews was performed. Thirteen pertinent clinical articles were found. The bibliographies of these articles were then searched for additional sources (Table 5.1). Table 5.1 Level of Evidence of Reviewed Published Studies
Management of Cervical Facet Dislocations: Role of Magnetic Resonance Imaging
Level | Number of Studies | Study Type |
|---|---|---|
I | 0 |
|
II | 0 |
|
III | 13 | Prospective cohort study (1 study)16 Retrospective cohort study (9 studies)4,6,7,9–11,15,18,19 Systematic review (1 study)13 |
 Incidence of Disk Herniation on Prereduction versus Postreduction Imaging
Incidence of Disk Herniation on Prereduction versus Postreduction Imaging
Level I Data
There are no level I data on this topic.
Level II Data
There are no level II data on this topic.
Level III Data
Several retrospective case series have been conducted on MRI after acute cervical spine and spinal cord injuries associated with cervical disk herniations.16,18,19 These studies note the incidence of cervical acute disk herniation ranging from 5% to greater than 80%, with an average incidence of ~40%.16
Unfortunately, the literature is very inconsistent with regard to methods of evaluation for the presence of disk herniation and the definition of a disk herniation. Some investigators have used various imaging modalities, including computed tomographic (CT) scans, CT scan after myelograms, and MRI to evaluate for disk herniations. No randomized, controlled trial has been performed to compare these modalities, and thus an overall incidence rate using these studies may not reflect the true incidence of a posttraumatic cervical disk her niation. Cervical MRI for acute spine trauma has become more prevalent in major trauma centers and emergency departments, and through its increased use it has been shown to be reliable in detecting disk herniation, epidural hematoma, and soft tissue injuries with sensitivity equal to or greater than that of other modalities.3
Doran et al retrospectively reviewed and reported on 13 acute cervical spine trauma patients with either unilateral or bilateral locked facets of the cervical spine.7 The first nine patients underwent immediate closed reduction using either or both traction and manipulation. Reduction was discontinued in 33% of these patients (3/9) due to new neurological deficits consisting of deltoid weakness, intractable arm pain, and biceps weakness, respectively. Of these nine patients, six had frank disk herniation and three had evidence of disk bulging on postreduction MRI. The authors then changed their treatment algorithm and had all patients undergo MRI prior to reduction, including the last four patients in the series. A frank disk herniation was identified in the remaining four patients of this series. The combined pre- and postreduction incidence of acute cervical disk herniations after cervical facet dislocation in this series was 77%.
Eismont et al reported on 68 patients who presented over a 7-year period with subluxation or dislocation of the cervical facet joints.6 Their protocol included closed reduction with Gardner-Wells skull tongs (Trent-Wells, Inc., Southgate, CA) for a period of up to 72 hours. During this period patients underwent imaging (either myelogram, CT, or MRI) to evaluate for the presence of disk herniation. Six of the 68 patients in this series had evidence of a herniated disk with protrusion of disk material into the canal for a postreduction herniated disk incidence of 9%.
Harrington reviewed 37 consecutive patients with cervical fracture subluxations who presented over a 5-year period.18 Nine patients were found to have radiological evidence of disk herniation that deformed the thecal sac or nerve roots on postreduction CT myelogram or MRI. Almost 50% of patients with partial deficits had evidence of a herniated disk. The authors concluded that neuroimaging should be obtained in all patients with cervical fracture subluxation and neurological deficit prior to reduction to rule out the presence of a compressive disk herniation.
Grant et al published a retrospective review of 82 patients with an acute traumatic cervical spine injury that were treated with early closed skeletal traction reduction.19 This series included 50 patients with either a unilateral or a bilateral facet dislocation. Cervical spine MRI scans were obtained in all patients within 24 hours of completion of the closed reduction. The authors reported an overall incidence of disk injury of 46%, which did not correlate with the mechanism of injury. The incidence of disk injury in this study was significantly associated with age greater than 55 years (p < 0.05).
The single prospective study comparing the pre- and post-reduction MRI in the setting of acute cervical facet dislocations was published by Vaccaro et al in 1999.16 In this series, 14 consecutive patients who presented with cervical spine facet dislocations underwent both pre- and postreduction MRI. After completion of the MRI scans, patients underwent a closed reduction, which was successfully performed in nine patients. All patients were awake, cooperative, and alert during traction, and no patient had neurological deterioration. Despite the clinical results, on MRI two patients had disk herniations prior to the reduction, and this number increased to five after the closed reduction. Thus the overall incidence of disk herniation after reduction was 43%. The authors note that, although there was a radiographic increase in the incidence of disk herniations, this did not correlate with the clinical results where no patient worsened with traction.
Summary of Data
There are no level I or level II data on this topic. However, there were several clinical series that were reviewed, including studies conducted before the widespread use of cervical MRI. The incidence of disk herniation in published studies ranges from 15 to 80%, with an average incidence of approximately one third to one half of patients.16 The data are summarized in Table 5.2.
Pearls
• There is no level I or level II evidence regarding the incidence of disk herniation on prereduction versus postreduction imaging in traumatic cervical facet dislocation.
• There is weak evidence to suggest that disk herniation with closed traction reduction of cervical facet dislocation occurs in roughly one third to one half of patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree