6 Cervical facet dislocations occur after high-energy trauma to the cervical spine and occur most commonly after motor vehicle accidents, diving injuries, and falls. Unilateral facet dislocations are typically associated with flexion-rotation injury, whereas bilateral facet dislocations are flexion-distraction type injuries. Translation at the dislocated cervical segment compromises spinal canal and neural foraminal diameter. In addition, an associated disk herniation rate as high as 42% has been reported.1 As a result, varying degrees of spinal cord and nerve root injury can occur. Injuries associated with cervical facet dislocations have an extremely high morbidity and can be difficult to manage in the acute trauma setting. The first step in addressing cervical facet dislocations involves an appropriate plan for reducing the dislocated segment. Although the spine literature does not define a specific time window that is ideal to accomplish reduction, it is generally accepted that the sooner a successful reduction is accomplished, the better likelihood that some degree of neurological recovery may occur. Animal models have supported this hypothesis. Delamarter et al created a canine model of cauda equina compression and showed that somatosensory evoked potentials at 6 weeks were directly correlated with the length of compression; the dogs undergoing compression for 6 hours or longer showed no improvement, whereas those undergoing compression for 6 hours or less showed some improvement.2 Although the translation of animal data to human use should be performed with caution, it provides sound evidence that leads us to believe that timing of decompression may affect neurological outcome in patients with spinal cord injury. The first report of closed reduction was performed by Walton in 1893 in a patient with cervical deformity secondary to facet dislocation.3 A modern technique of closed reduction was described by Cotler et al.4 They described a technique of skeletal traction using stainless steel tongs and the sequential addition of weight beginning with 10 lb and continuing in 5 to 10 lb increments with lateral cervical x-rays to monitor for overdistraction as well as meticulous neurological exam to monitor for worsening neurological deficit. Muscle-relaxing agents such as valium were used to relax the paraspinal musculature, and in cases of locked facets, manipulation of the direction of traction was performed with mild flexion to unlock the facets. There has been no maximum weight for cervical traction described, but further studies by Cotler et al supported by cadaveric studies showed that weights of 100 to 140 lb could be tolerated by the cervical spine as long as no evidence of overdistraction was present.4 Hadley et al characterized further those patients that would most likely experience successful closed reduction. In their series of 68 patients they found that those patients with fractures at other levels of the cervical spine, fracture of the facet at the level of subluxation, or worsening of their neurological deficit with cranial traction were most likely not to undergo a successful closed reduction.5 Immediate closed reduction of cervical facet dislocation has been supported in the spine literature, and in an awake, alert, cooperative, and properly monitored patient with no distracting injuries, it can be performed safely without aggravating or creating new neurological deficits. There have been reports of neurological worsening secondary to herniated cervical disk at the level of subluxation after posterior open reduction but no reports of permanent worsening neurological deficit after closed reduction in the appropriate patient.6 However, this perceived risk of canal compromise secondary to disk herniation has prompted some clinicians to obtain prereduction magnetic resonance imaging (MRI). This practice has been debated in the literature by those who feel that unnecessary delays in restoring spinal alignment could potentially worsen outcomes. Table 6.1 Level of Evidence of Published Studies
Management of Cervical Facet Dislocations: Timing of Reduction
Level | Number of Studies | Study Type |
|---|---|---|
II | 1 | Prospective cohort8 |
III | 4 | |
IV | 3 | Case series10 |
|
|
There have been many reports in the literature examining the role of closed reduction in acute cervical facet dislocations. There are several issues that remain controversial: (1) Does timing of reduction affect neurological outcome? (2) Is closed reduction with cranial tongs safe? (3) Is there an increased risk of cervical disk herniation with closed reduction?
A comprehensive review of the literature was performed to ascertain the best available evidence for each of these topics. A Medline search was performed and the references of each of the articles were reviewed for any additional studies. A search for the term cervical facet dislocation returned 203 articles. An additional search of the terms cervical facet dislocation and reduction returned 70 articles. There were no level I studies identified in the search criteria. There was one level II study, and the majority of studies were levels III and IV (Table 6.1).
 Does Timing of Reduction Affect Neurological Outcome?
Does Timing of Reduction Affect Neurological Outcome?
Level I Data
There are no level I studies available.
Level II Data
There are no level II studies available.
Level III Data
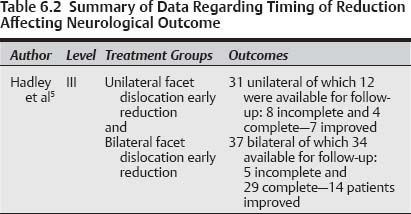
Hadley et al reported a retrospective cohort of 68 patients with cervical facet dislocation, 37 of which had bilateral locked facets, and 31 patients had unilateral facet dislocations, to examine methods of reduction, methods of spinal stabilization, and long-term outcome (Table 6.2).5 Median age of the patients was 29 years, and males outnumbered female patients four to one. The majority of injuries were caused by motor vehicle accidents (61%), with diving injuries being the second most common type of injury (15%).
Thirty-one patients presented with unilateral facet dislocations, and the most common level of injury was C6–C7. Twenty-four patients had neurological injury: seven had root injury only; 10 had incomplete spinal cord injury; and seven had complete spinal cord injuries. Twenty-nine patients were treated immediately upon arrival to the emergency department with placement of Gardner-Wells (Trent-Wells, Inc., Southgate, CA) cranial tongs or a halo cranial ring for cervical traction. The two patients excluded from this population were admitted in a subacute fashion and were not treated with cervical traction.
Eighteen patients had successful closed reduction of uni-lateral facet dislocation requiring an average passive weight of 9.8 lb per superior injury level. Eleven patients could not have their injuries reduced by closed reduction, and eight were taken to the operating room for open reduction and internal fixation. The remaining three patients had complete spinal cord injury and coexistent severe traumatic injuries and medical morbidities that precluded open reduction. These patients were treated with external immobilization.
Thirty-seven patients presented with bilateral facet fracture dislocations of the cervical spine. The most common level of injury was C6–C7. Six patients had incomplete spinal cord injury, and 31 had complete spinal cord injuries. All patients were again treated with aggressive attempts at closed reduction by the same methods employed for the unilateral facet dislocation cohort.
Twenty patients had successful closed reduction with passive cervical traction (average 9.4 lb per superior injury level). Fifteen patients were treated with external immobilization, and five were treated with internal fixation followed by external stabilization. All 17 patients with failed closed reduction were treated with open reduction and internal fixation.
Successful reduction was achieved in 58% of patients treated with “immediate” or “early” craniocervical traction upon presentation to the emergency room. Follow-up was achieved in 83% of unilateral facet injury patients and 92% of bilateral facet injury patients (mean duration 18 and 24 months, respectively).
In the unilateral facet dislocation cohort, neurological recovery ranged from improvement of neck pain and radicular symptoms to resolution of incomplete spinal cord injury and some improvement in one patient with complete spinal cord injury. Of eight patients with incomplete spinal cord injury available for follow-up, three were neurologically intact, three others had significant but incomplete recoveries and were ambulatory. One of the four patients with complete injury regained ambulatory status but still had significant residual motor and sensory deficits.
Of all the patients, eight suffered neurological deterioration, of which seven patients worsened during closed reduction. Four of those seven patients improved after ORIF. Two regained root function but remained complete injuries, and the remaining patient deteriorated after ORIF secondary to complications of a posterior fossa stroke.
Successful closed reduction and realignment of the cervical spine was achieved in 58% of the patients in this retrospective cohort, and 78% of those patients achieved some degree of neurological recovery after reduction. Factors that were responsible for unsuccessful closed reduction included fractures at another cervical level, facet fracture at level of subluxation, and worsening of neurological deficits.
The authors could not discern which method of reduction was superior to the other in terms of recovery of neurological function. They conceded that too few patients in the two groups made neurological recovery that would allow statistical comparison of the two groups. Their impression of the 10 cases that experienced significant neurological recovery was that time to reduction was the most compelling factor that influenced neurological recovery, although this group was very small.
Summary of Data
The data provided by the authors support early decompression of neural elements by closed reduction. Their cohort, although relatively small, was one of the largest patient populations examined where neurological outcome was assessed directly with long-term follow up. Although a specific time period was not defined for “early” reduction, attempts were made in the emergency department on presentation, and their data support the idea that the earlier neural elements are decompressed, the better chance there is for those neural elements to recover function. This hypothesis was supported by animal models of spinal cord injury that also demonstrated the benefits of early decompression.2 The most readily accessible means to achieve decompression is by closed reduction using cervical traction. It can be applied quickly, and many studies have shown that rapid addition of weight can be performed safely with a high rate of successful reduction.4,5,7,8
Pearls
• At this time the human clinical evidence that immediate reduction of facet dislocation can impact neurological recovery is weak.
• The animal data in favor of immediate reduction are compelling and favor reduction as rapidly as possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree