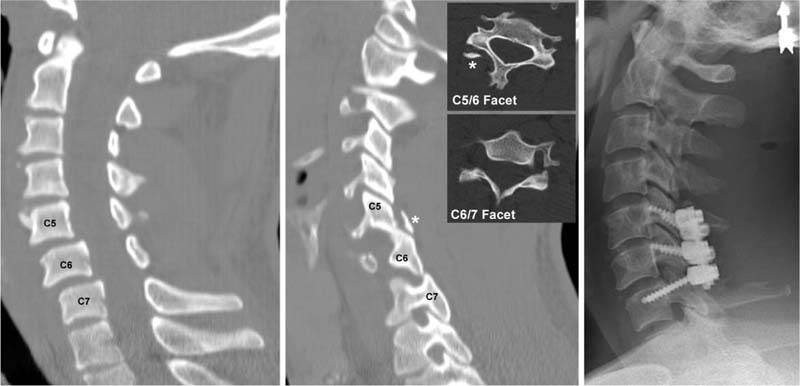
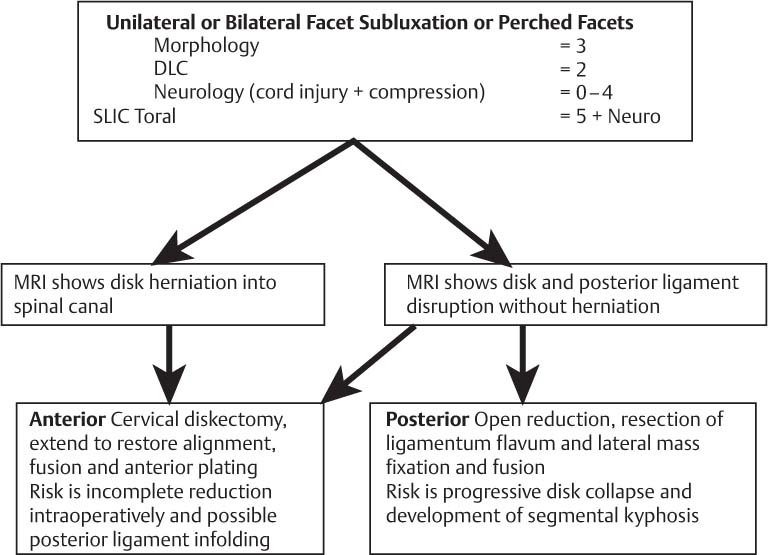
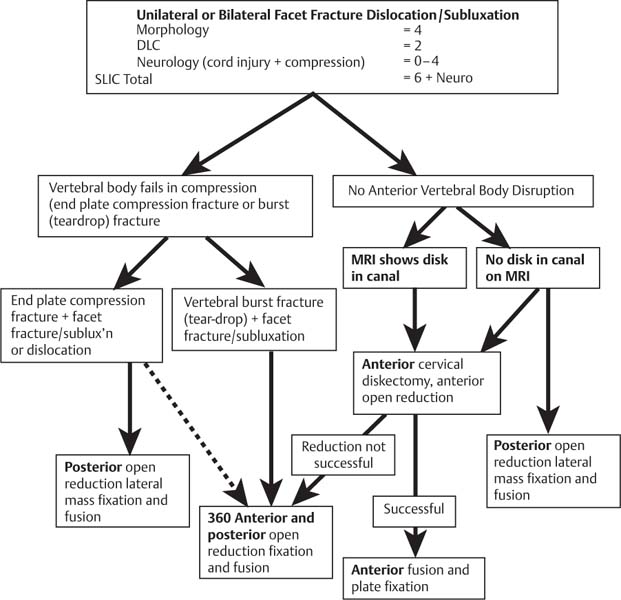
4 Cervical facet fractures and dislocations represent ~6% of all cervical spine fractures.1 Despite being so common, their nomenclature, diagnosis, and treatment remain controversial. These injuries present with a spectrum of neurological injury from neurologically intact to complete tetraplegia. They may be unilateral (involving one facet joint) or bilateral (involving both facet joints), may involve the superior or inferior articular processes, and may be associated with subluxation or dislocation. Subluxation is an abnormal position of the inferior facet of the upper vertebra on the superior facet of the vertebra below while maintaining some contact between the two joint surfaces.2 Dislocation is characterized by the facet of the vertebra riding up and over the superior facet of the vertebra below, giving rise to no residual articular surface contact between the two.2 This chapter highlights some of the controversies associated with these relatively common injuries and provides evidence-based recommendations for treatment. Motor vehicle accidents, physical violence, and falls are the most common cause of facet fracture/dislocations.3 Flexion alone is not capable of producing unilateral facet dislocation,4 and hyperextension, lateral tilt, and rotation are thought to contribute to unilateral facet fracture/dislocations.5 The mechanisms of bilateral facet dislocation include a flexion moment, forces of axial compression, and anterior shear.6 This results in facet separation and anterior dislocation with a resultant posterior shear force upon the facets as they are locked, leading to a high likelihood of facet fractures.6 Most (73%) of these bilateral facet dislocations are associated with a facet fracture.7 A floating lateral mass (fractured pedicle and lamina) occurs in up to 19% of fracture/dislocation cases, creating instability involving two motion segments.8,9 Facet injuries most commonly occur in the lower cervical spine,1,2,6–8,10–12 C5–C6 (25 to 60%) and C6–C7 (25 to 30%).11,13 The superior facets at C6–C7 have shorter facet length, shorter facet height, and in vivo have a more horizontal orientation than the more cranial facets, all of which pre-dispose this joint to a greater likelihood for dislocation and fracture.14 Multiple levels of injury are common, with rates of 25% reported.4,8,15 Clinically, many patients with cervical fractures have associated head or chest trauma or both.9,12 There may be a paucity of clinical signs if the patient presents with intact neurology; however, careful assessment can demonstrate root pathology or cord injuries in most cases associated with dislocation. Isolated undisplaced fractures may present with a paucity of clinical signs and symptoms. The presence of midline cervical tenderness or a reduced or painful cervical range of motion necessitates a careful investigation for a facet fracture or dislocation. A large number (33%) of facet injuries are missed at initial presentation despite medical evaluation.9 About 90% of fracture/dislocation injured patients have a neurological injury.1 Up to 87% of patients with unilateral facet dislocation report a history of transient cord concussion, including transient quadripareses.3,11 Bilateral facet dislocations are associated with neurological compromise in up to 100% of cases (with 83.8% complete cord injuries).1 However, in unilateral facet fractures or dislocations, the rate of complete spinal cord injury has been reported as 15.6%, incomplete spinal cord injury 22%, with isolated nerve root deficits in 37% of cases.4 In cases of nerve root injury with unilateral facet fractures, there is often a fragment of the facet within the foramen, which may be responsible for some degree of residual nerve root compromise.3 The presence of spinal shock (profound hypotension and associated bradycardia) occurs in ~19% of facet fracture/dislocations.1 It has been associated with a poor prognosis of neurological recovery, with no recovery noted in a series of 13 such patients.1 Historically, unilateral facet dislocations were defined as having vertebral body translation up to 25% of the anteroposterior diameter of the adjacent vertebral body on plain lateral radiographs.13,16 A “bow-tie” sign is indicative of a facet dislocation as one lateral mass lies in front of the other rather than articulating normally.10 Computed tomo-graphic (CT) scanning with reformatted images5,17–19 has to a great extent supplanted plain radiographic images, oblique views,5 and flexion-extension radiographs.3,12,20 Magnetic resonance imaging (MRI) is the most appropriate modality for assessing the discoligamentous complex (DLC) and the spinal cord.21,22 The ultimate goal of treatment of any spine injury is to return patients to their preinjury state of health; however, specific to cervical facet fractures, goals include either or both preservation and recovery of neurological function, the restoration of anatomical alignment, and the establishment of short- and long-term spinal stability.4,5,10,13 We will assume that all of these patients are treated according to the latest trauma protocols, and we will thus focus simply on the spinal column and cord injury. Controversy remains as to which patients necessitate operative versus nonoperative management. Once the choice for operative management has been made, opinions conflict as to which operative approach or approaches to utilize.23 The safety and efficacy of closed reduction have long been debated in the management of facet dislocations. Contraindications to closed reduction include the presence of fracture fragments in the foramen, herniated disk disruption, and the inability to adequately monitor the patient’s neurological and radiographic status.3 Braakman and Vinken suggested that spontaneous stabilization occurred in facet dislocations, and that this was independent of reduction.24 Beatson25 suggested that unilateral fracture dislocations of the cervical spine could be left dislocated with minimal long-term symptoms. Cheshire26 suggested that nonoperative management resulted in an acceptable rate of late instability (7.3%).10 Conversely, Rorabeck et al16 and O’Brien et al27 found that unreduced patients developed significant pain, progressive deformity, and significant late instability (> 20%), despite long periods in halo immobilization.10 If a closed reduction is to be attempted, then there are several prerequisites4,15,28: 1. An alert cooperative patient in whom a reliable neurological exam can be performed 2. Ability to visualize the cervical spine segment affected on either x-ray or fluoroscopy 3. Ability to safely apply traction (no skull fracture) Reduction is accomplished using cranial tongs and a weight or a traction device. The weight is gradually increased from 10 lb initially (to rule out gross ligamentous instability, particularly at the occipitocervical junction), to as high as 140 lb.24,29 An average of 9.4 to 9.8 lb per segment above the injury level was necessary for reduction of uni-lateral and bilateral facet dislocations.1 Traction should be ceased if greater than 10 mm distraction of the affected segment has been achieved even in the absence of reduction.4 Sequential radiographic and clinical neurological observation is mandatory.1,4 Bilateral facet dislocations reduce more often than unilateral facet dislocations.3,8,16 Reduction is often effected with an audible click. Burke and Berryman described a closed reduction maneuver involving traction and flexion coupled with rotation in the opposite direction to that of the dislocation.2,4 Positioning the neck in slight extension following reduction will often hold the reduction. The association of a facet fracture with dislocation may result in a mechanical block to reduction.1,2,15 With a presentation of neurological compromise and/or spinal instability, the prompt availability of an operating room obviates the need for an awake closed reduction. Can weighted traction alone reduce unilateral facet dislocations? As low as 25% successful closed reduction rates of unilateral facet dislocations have been reported.7,8,16 Other series report successful reduction in up to 100% of cases by using large traction weights.15,29,30 Whether to perform a closed reduction with traction, proceed to an MRI scan, or proceed directly to the operating room remains a point of contention. The degree of neurological injury often guides management, so that in a complete spinal cord injury one may argue that there is nothing to lose from an emergent reduction in the emergency room. In patients that have no neurological injury, a clinician may consider an urgent MRI scan prior to reduction, or definitive surgery to obtain some appreciation for the location of disrupted disk material or other ligamentous structures such as the ligamentum flavum (Fig. 4.1). In patients who have an incomplete cord injury, debate remains as to the most appropriate sequence of management. Fig. 4.1 Facet dislocation with associated disk herniation, C6–C7. (© 2006 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 14(2), pp. 81–85 with permission.) Cervical orthoses have been utilized as definitive treatment for facet fractures with varying success. Although many forms of orthoses have been used, traditionally a halo vest orthosis for unstable injuries is usually favored. The halo is applied for a period of 12 weeks, followed by flexion-extension x-rays and then physical therapy with a cervical collar for comfort in patients that had reasonable radiographic stability. However, poor results have been associated with halo immobilization in lower cervical fractures, in particular with unstable facet fractures and dislocations.28,30 Johnson et al30 and Ivancic et al31 have noted the “snaking phenomenon” first described by Koch and Nickel32 of the lower cervical spine in both the coronal and sagittal planes with the use of halo immobilization. This phenomenon predisposes unstable injuries to displacement, loss of reduction, and poor outcomes when treated in a halo brace. Indications for operative intervention fall into two categories: absolute indications and relative indications. Absolute indications include the following4: 1. Fractures with impingement of the spinal cord or nerve root (s) associated with spinal cord injury or progressive neurological deterioration 2. Unstable fracture patterns unreducible by closed means 3. Displaced fracture separation of the lateral mass33 4. Fracture/dislocations or subluxations with an associated herniated disk 5. Delayed presentation of dislocation Fig. 4.2 Unilateral facet injury at C5–C6 and C6–C7 demonstrating both facet fracture and dislocation. (© 2006 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 14(2), pp. 81–85 with permission.) Relative indications for operative management include the following4: 1. Unstable fracture patterns 2. Facet fractures with impingement of nerve root (s) 3. Fractures that displace while undergoing nonsurgical treatment 4. Delayed presentation of fracture Internal fixation allows early stabilization, reduction and maintenance of anatomical alignment, and stabilization following the operative decompression of neural structures (Fig. 4.2). Controversies over whether closed reduction and the application of a halo brace is as effective as operative reduction and fusion in the management of facet fractures and dislocations have been debated in the literature. The level of evidence of comparative studies published in the literature is summarized in Table 4.1. There are no level 1 evidence studies comparing operative versus nonoperative management. A predictive classification system for subaxial injuries of the spine incorporating fracture morphology, status of the DLC, and neurological status has been developed and validated.34 The Subaxial Injury Classification (SLIC) severity scoring system gives increasing point values for increased severity of injury within each category (Table 4.2). Injuries that score 5 or more require surgery, 3 or less are treated nonsurgically, and if injuries score 4, the treatment options are equivocal.34 The SLIC scoring system guides a surgeon to operative or nonoperative management through a qualitative systematic review, and associated consensus opinion of a select group of experts35 (Fig. 4.3 and Fig. 4.4).
Management of Cervical Facet Fractures: Surgical Indications and Approach
 Mechanism of Injury and Demographics
Mechanism of Injury and Demographics
 Diagnosis
Diagnosis
 Treatment
Treatment
 Closed Reduction
Closed Reduction
 Closed Immobilization
Closed Immobilization
 Surgical Indications
Surgical Indications
Level 1 Evidence
Level 2 Evidence
Level | Study | Topic |
|---|---|---|
I | No papers |
|
II | Vaccaro et al34 | Describes the subaxial injury classification of cervical subaxial injuries |
| Dvorak et al35 | Evidence-based algorithm of care for cervical subaxial injuries |
III | Dvorak et al13 | Outcome study of 90 cervical facet fractures treated surgically and nonopertively; operative patients had better outcomes |
| Beyer et al36 | Operative patients had better results in this comparative study |
| Lifeso and Colucci9 | Anterior surgery demonstrated better results than posterior or nonoperative |
| Aebi et al37 | Anterior surgery is feasible with good results |
Table 4.2 Subaxial Injury Classification Scale
| Points |
|---|---|
Morphology |
|
No abnormality | 0 |
Compression + burst | 1 + 1 = 2 |
Distraction (e.g., facet perch, hyperextension) | 3 |
Rotation or translation (e.g., facet dislocation, unstable teardrop or advanced-stage flexion-compression injury) | 4 |
Discoligamentous complex |
|
Intact | 0 |
Indeterminate (e.g., isolated interspinous widening, magnetic resonance imaging signal change only) | 1 |
Disrupted (e.g., widening of anterior disk space, facet perch, or dislocation) | 2 |
Neurological status |
|
Intact | 0 |
Root injury | 1 |
Complete cord injury | 2 |
Incomplete cord injury | 3 |
Continuous cord compression (neuromodifier in the setting of a neurological deficit) | +1 |
Source: Dvorak MF, Fisher CG, Fehling MG, et al. The surgical approach to subaxial cervical spine injuries. Spine (Phila Pa 1976) 2007;32(23):2620–2629. Reprinted with permission.
Level 3 Evidence
In a cross-sectional outcome study by Dvorak et al, nonoperatively treated unilateral facet injuries of the subaxial cervical spine had greater residual pain and disability than those of healthy uninjured controls.13 Furthermore, nonoperatively treated unilateral facet dislocations had poorer long-term outcomes than operatively treated cases despite being injuries of lesser initial severity.13
A retrospective comparative study of 34 patients with uni-lateral facet injuries showed that patients treated operatively had better overall results for rate of fusion, rate of anatomical reduction, rate of preserved reduction, and long-term pain relief than similar injuries treated nonoperatively.36
Lifeso and Colucci evaluated a retrospective control cohort of 29 cases of unilateral fracture dislocations with rota-tory listhesis.9 All 21 cases treated by nonoperative means had failure of reduction, persistent pain, and/or neurology. The 20 treated with posterior wiring had a 45% rate of loss of reduction despite the presence of apparently solid posterior fusions.9 In the 18 prospectively evaluated anterior cervical diskectomy and fusion (ACDF) patients, they found a 100% rate of fusion and no failures at a minimum of 2-years follow-up.
Fig. 4.3 Subaxial Injury Classification (SLIC) algorithm for unilateral or bilateral facet subluxation or perched facets. DLC, discoligamentous complex; MRI, magnetic resonance imaging. (From Dvorak MF, Fisher CG, Fehling MG, et al. The surgical approach to subaxial cervical spine injuries. Spine (Phila Pa 1976) 2007;32(23):2620–2629. Reprinted with permission.)
Aebi et al found that facet fractures and dislocations have better neurological outcomes when reduced within 6 hours of injury.37 Aebi et al later demonstrated that anterior surgery could be utilized to treat posterior injuries with good outcomes.37
Level IV Evidence
MRI can be used to assess the soft tissue structures of the cervical spine, even in the setting of a reduced unilateral facet or bilateral facet dislocation.19 Integrity of the anterior longitudinal ligament (ALL) tends to suggest a unilateral facet dislocation has occurred as opposed to a bilateral facet injury when both the ALL and posterior longitudinal ligament (PLL) have been disrupted.19
Closed reduction of unilateral and bilateral facet dislocations has been shown to be safe by Cotler et al.29 In his series of 24 facet dislocations, nine of 13 bilateral facet dislocations and seven of 11 unilateral facet dislocations were successfully reduced utilizing traction and gentle manipulation with muscle relaxation in the awake patient. Likewise, Rizzolo et al state that reduction with traction in the alert patient is a safe procedure.15
Rorabeck et al demonstrated that unilateral facet injuries are generally unstable and have poor outcomes when left dislocated or treated without spinal fusion.16 He suggested that if closed reduction of these lesions was successful, then nonoperative bracing was reasonable; however, if there was evidence of late instability, a fusion was indicated.16 Patients who had lesions that could not be reduced operatively had good outcomes from single-level in situ fusion.
Hadley et al’s series of 31 patients with facet fracture dislocations treated by closed reduction and/or halo immobilization had seven (23%) failures at an average of 18 months’ follow-up.1 In Hadley’s concomitant retrospective series of 24 patients with open reduction internal fixation as management who had long-term follow-up, only one developed instability (progressive kyphosis). He reported that each of the 27 cases undergoing operative reduction had successful realignment, with 60% of these regaining some neurological function. In the cohort of 66 attempted closed reductions, 38 (58%) were successful, with neurological improvement in 78% of these. In the 28 (42%) unsuccessful closed reductions, seven had neurological deterioration.
Bucholz in a series of 57 subaxial fractures had a failure rate of halo immobilization of 23% overall, and 45% for dislocated presentations.20 The majority of these failures were recurrent dislocations while still in the halo immobilization, and fractures involving the middle (C3–C4 and C4–C5), more mobile cervical spine. Other large series of facet dislocations managed with closed reduction and halo immobilization have demonstrated similar poor results.28,30
Mortality rates for cervical fractures managed with a halo brace range from 0.5 to 6.5%.20
In ~50% of cases of unilateral or bilateral facet dislocation, reduction of the facets can be achieved by closed means.1,3 Most other cervical dislocations can be reduced by diskectomy and anterior instrumentation.38
Fig. 4.4 Subaxial Injury Classification (SLIC) algorithm for bilateral facet fracture dislocation/subluxation. DLC, discoligamentous complex; MRI, magnetic resonance imaging. (From Dvorak MF, Fisher CG, Fehling MG, et al. The surgical approach to subaxial cervical spine injuries. Spine (Phila Pa 1976) 2007;32(23):2620–2629. Reprinted with permission.)
Patients treated by closed immobilization tend to develop greater rates of instability, long-term pain, and loss of reduction than patients treated with operative fusion.1,3,8,10,16,18 Improved anatomical reduction and secondary decompression of neurological structures correlated with improved outcomes of operatively managed cases over nonoperatively managed cases.18
Spector et al examined CT scans of 24 patients with 26 unilateral facet fractures that were initially treated nonoperatively. They statistically analyzed measurements of fracture fragment width and height compared with the intact contralateral facets. Subsequently they predicted that “fracture fragments greater than 1 cm in height or a fracture fragment representing greater than 40% of the height of the intact lateral mass was associated with failure of nonoperative management.”39
Consensus Statements
The Spine Trauma Study Group (STSG) has published a consensus statement regarding measurement techniques for lower cervical spine injuries.40 Standardized terminologies were stated for measurement of kyphosis, vertebral body translation, vertebral body height loss, maximal spinal canal compromise and spinal cord compression, facet fracture fragment size, and percentage facet subluxation.
Conclusions
Facet fractures and dislocations encompass a diverse group of injuries that hold the potential of either good functional outcomes or catastrophic outcomes. Closed reduction can be performed safely in the presence of set prerequisites. Halothoracic immobilization is unreliable and has an unacceptable rate of failure for facet fracture dislocations.
Bilateral facet fractures and/or dislocations are almost always unstable; hence operative stabilization is currently seen as the most appropriate management.
Occasional minor undisplaced facet fractures without concomitant dislocation can be managed with external orthoses and vigilant radiographic follow-up.
Pearls
• Completely undisplaced fractures may be treated in a cervical orthosis, but the outcomes of surgical stabilization for most other fractures or any subluxations or dislocation remain superior to nonsurgical treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree