Mechanics of Neurological Impingement
Brian J. C. Freeman
Anatomical stenosis of the lumbar spinal canal was first suggested as a cause for spinal stenosis syndromes by Sarpyener (1) and Verbiest (2,3). It is necessary to review the basic anatomy before discussing the classification of lumbar spinal stenosis and in particular the mechanics of neurological impingement in lumbar spondylosis, spondylolysis, and spondylolisthesis.
ANATOMY
The vertebral column houses osseoligamentous spaces that accommodate, protect, and transmit the delicate neurovascular structures. It is essential to define clearly what is meant by the terms spinal canal, nerve root canal, and intervertebral foramen.
Spinal Canal
The spinal canal is formed behind the articulated vertebral body by the posterior elements of the vertebral column. The normal lumbar spinal canal varies in shape as it descends. In the normal state it is circular in cross section in the upper part of the lumbar spine and trefoil in shape at the lower part. The lumbar spinal canal can be divided into a central portion and two lateral portions. The central portion is occupied by the thecal sac. Hoffman ligaments sequentially attach the thecal sac to the anterior wall of the vertebral canal and posterior longitudinal ligament especially at the disc level.
Nerve Root Canal
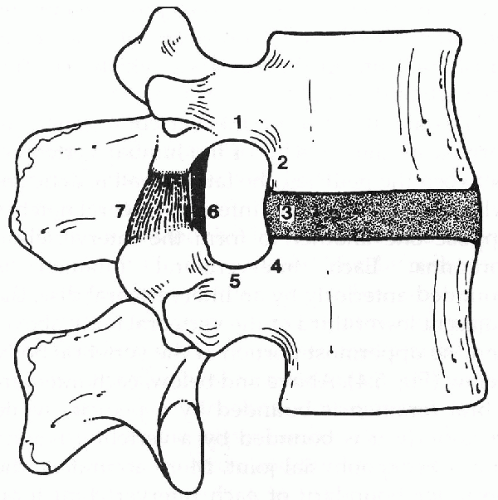
The nerve root canal is a tubular conduit that starts in the spinal canal at the point where the nerve root sheath comes off the dural sac and ends where the nerve root emerges from the intervertebral foramen (Fig. 4.1). The length of the canal varies, depending on the site of origin of the root sleeve from the dural sac. The L5-S1 root canal is considerably longer than those running at higher lumbar levels. The roof or posterior aspect of the canal is formed by the ligamentum flavum and contiguous borders of the superior articular process and superior margin of the lamina corresponding in number to the nerve root. Further laterally, the roof is formed by the pars interarticularis of this lamina and the ligamentum flavum related to it. The floor or anterior aspect is formed by the annulus fibrosus of the intervertebral disc, the posterior surface of the vertebral body, and their soft tissue coverings. The medial “wall” of the canal is formed by the dural sac and soft tissues of the epidural space including fat, blood vessel, and nerve. The lateral wall is formed first by the medial side and then by the inferior aspects of the pedicle.
The nerve root canal contains the nerve root bundle, radicular arteries, veins, and lymphatic vessels. The nerve root generally occupies the cranial portion of the foramina. The nerve root
canal has been compartmentalized by several authors into the entrance zone, the midzone, the exit zone, and the extraforaminal zone (4,5,6). These will now be described in detail:
canal has been compartmentalized by several authors into the entrance zone, the midzone, the exit zone, and the extraforaminal zone (4,5,6). These will now be described in detail:
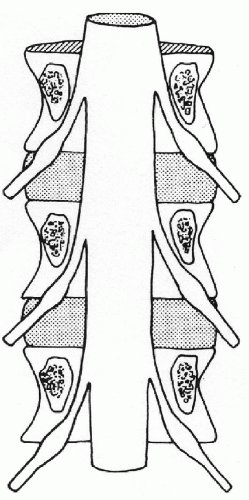 FIG. 4.1. Posterior view of the nerve root canals showing relationship of the nerve root to the pedicles. |
The entrance zone lies medial to the pedicle and the superior articular process. It is infundibular in shape and accommodates the root sleeve and the unsheathed nerve roots.
The midzone, also called the subpedicular or pedicle zone, extends from the medial to the lateral pedicle edge, is cylindrical in shape, and contains the nerve root and dorsal root ganglion.
The exit zone, also known as the foraminal zone or foramen proper, is a shallow annular hiatus, which Crock has compared to a doorway at the end of a passage (6).
The extraforaminal zone, or postcanal zone, is where far lateral disc herniations, extraforaminal ligaments, and membranes or bony structures such as the transverse process may compress, kink, or constrict lumbar nerves.
Intervertebral Foramen
The intervertebral foramen has the shape of an inverted teardrop. The superior boundary is the pedicle of the vertebra above. The inferior boundary is the pedicle situated caudal to the nerve root. The anterior wall is formed by the posterior aspect of the vertebral body, the intervertebral disc, and the body below. The posterior wall (or roof) is formed by the pars interarticularis, the ligamentum flavum attached to it, and the apex of the superior articular process of the vertebra situated at the inferior aspect of the foramen (Fig. 4.2).
DYNAMIC CHANGES
Dynamic radiographic studies such as flexion/extension radiographs and functional myelography have shown that the dimensions of the spinal canal change dramatically in flexion, extension, and rotation of the spine (7).
Rauschning has studied cadaveric lumbar spines frozen-in-situ in different functional positions (8). The sagittal dimensions of the spinal canal increase in flexion and decrease in extension. During flexion, the vertebral body moves closer anteriorly and farther apart posteriorly, stretching the posterior portion of the annulus fibrosis. The opposite occurs in extension of the spine: the ligamentum flava shorten, become thicker, and buckle and the annulus fibrosus bulges posteriorly causing a decrease of the sagittal dimension of the canal at the intervertebral level. The changes in size and shape of the vertebral canal that occur in flexion or extension are mainly caused by thickening and retraction of the ligamentum flava, and they involve the central spinal canal with the thecal sac undergoing constriction at the intervertebral level.
Dynamic changes in the nerve root canal do occur. They are caused by bulging of the posterolateral region of the disc into the subarticular portion of the nerve root canal and buckling of the anterior capsule of the facet joint. Rotational deformation of the vertebral canal affects the subarticular portion of the root canal. Torsion of a vertebra results in increased posterior bulging of the disc on the side toward which torsion occurs. On this side, the nerve root canal decreases in width.
Rauschning reported on 10 lumbar spines with slight to moderate degenerate changes frozen in postures known to cause neural compression (9). In specimens with normal intervertebral disc height, extension caused the superior articular process to slide superiorly and anteriorly pulling the thick capsular ligamentum flavum anteriorly, compressing and flattening the posterior aspect of the dorsal root ganglion. In this regard the L4/L5 motion segment displays the greatest mobility. In the presence of disrupted intervertebral discs, a vacuum phenomenon was observed in two facet joints when the specimen was frozen in rotation. The root sleeves were compressed and flattened by the bulging annulus fibrosus and the medial portion of the superior articular process and by infolding of the ligamentum flavum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree