Chapter 11 Median Nerve
Overview
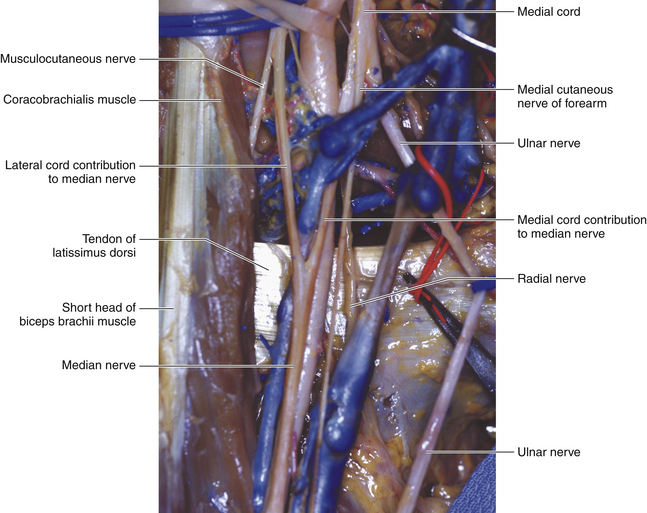
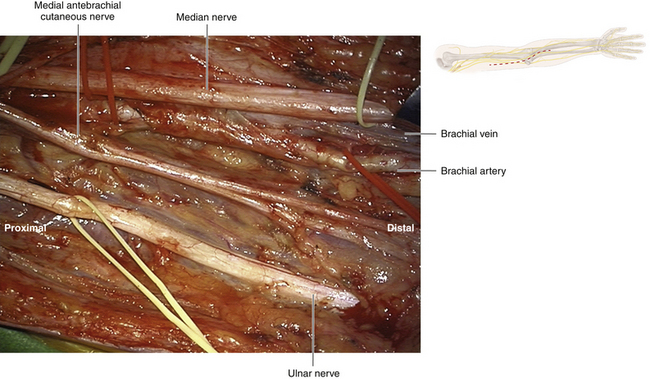
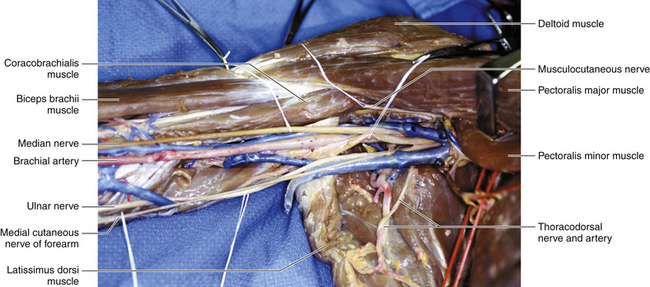
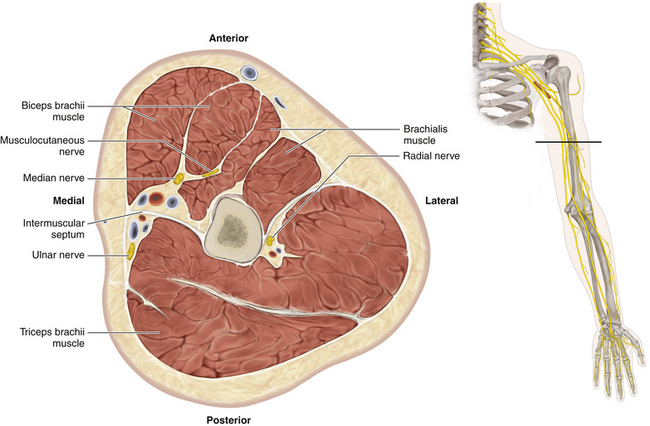
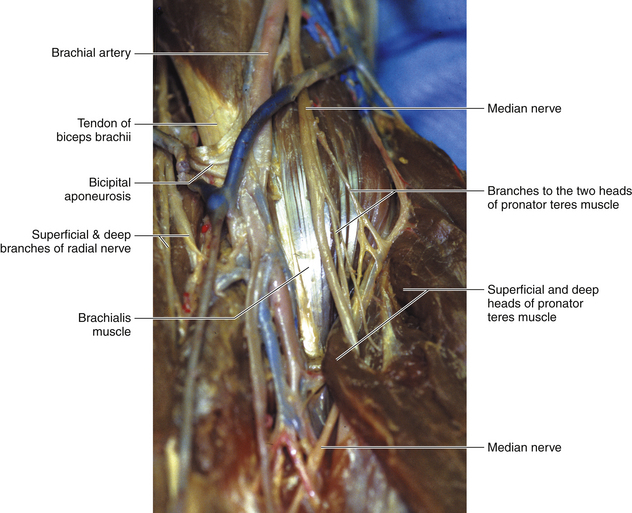
• The median nerve is derived from medial and lateral heads, so named according to their cord of origin. The medial cord contributes primarily motor fibers, and the lateral primarily sensory. The two heads clasp the brachial artery where the medial head runs across the front of the vessel, and the median nerve maintains this close relationship with the artery throughout the arm (Figures 11-1 and 11-2).
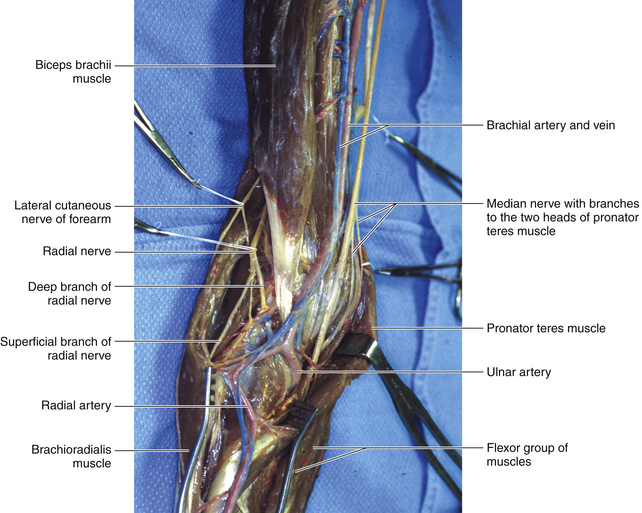
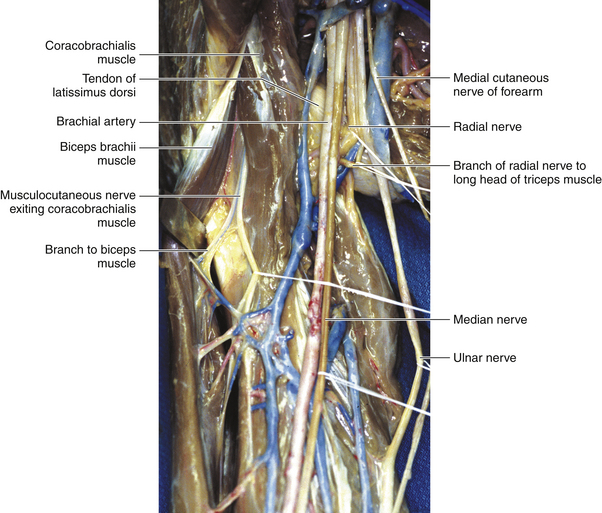
• The nerve runs at first lateral and later medial to the artery. The transition occurs at the level of the insertion of the deltoid. The ulnar artery runs posterior to the median nerve soon after the vessel is formed (Figure 11-3).
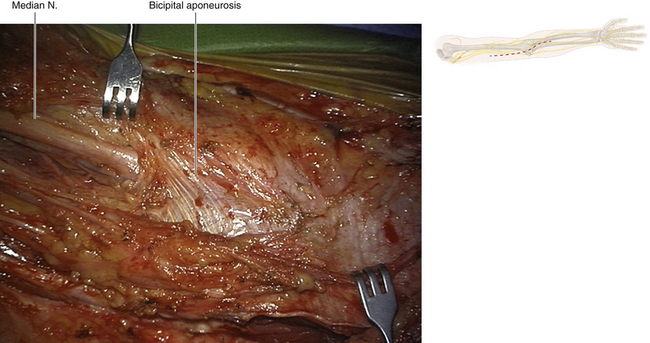
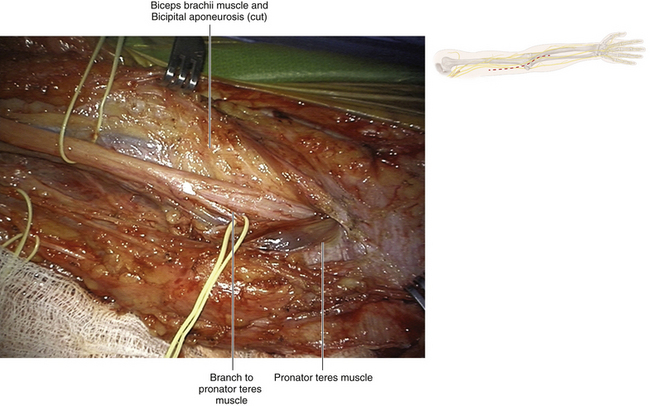
• Throughout its course, the nerve is deep to the investing fascia, which at the elbow is thickened by the bicipital aponeurosis (Figure 11-4).
Surgery
• The skin incision in the arm is placed over the course of the nerve. The pulsating brachial artery is the guide.
• The surgeon must distinguish the median, ulnar, radial, and cutaneous nerves in the proximal arm. The median nerve is lateral to and closely applied to the artery (Figures 11-5 and 11-6).
• Pathology frequently results in close adhesion of the adjacent nerve and artery. In the majority of cases, the nerve can be carefully separated by sharp dissection (Figure 11-7).
• If the surgeon encounters more than minimal adherence of the nerve to the artery, the artery must be dissected out both proximal and distal to the point of nerve injury. Tapes are loosely passed around the vessel at those points and serve as a guide to vascular occlusion, should this be required.
• Vascular clamps must be part of the peripheral nerve instrumentation set and the operating room nurse must know where a full vascular set is available, should this be required.
• In the event of hemorrhage, pressure is applied calmly and accurately, compressing the artery against the humerus. The assistant then applies the vascular clamps in an accurate and unhurried fashion, at the previously prepared sites proximal and distal to the arterial injury. Done in this manner, there is no further injury to the nerve or vessel; both, however, can easily occur if the surgeon has not prepared for brisk hemorrhage ahead of time.
• It is difficult to gain extra length when operating on the median nerve in the arm, so grafts are frequently required.
• The musculocutaneous nerve runs between the two heads of the coracobrachialis. A phylogenetically degenerate third head may persist and may compress the median nerve. A downward and medially pointing bone spur may be present on the anterior aspect of the distal humerus. This will be missed on a routine anteroposterior x-ray film but may be seen in profile on an oblique view. A ligament runs from this spur to the medial epicondyle (ligament of Struthers) and the ligament may compress the median nerve. (This situation is similar to a cervical rib, where the band from the tip of the rib is the culprit, rather than the rib itself.)
• Only on rare occasions is there a median branch communicating with the ulnar nerve (an arm-level Martin-Gruber anastomosis) or a branch from the median nerve to an antebrachial cutaneous nerve.
• This is in contrast to the frequent back-and-forth communications between the lateral and medial cords, and sometimes the posterior cord, as the median nerve is being formed proximally.
The Elbow and Proximal Forearm
• The surgeon must understand the anatomy and function of all forearm muscles so that an accurate clinical examination can be conducted. In addition, some specific points need to be stressed to allow the precise and accurate conduct of surgery.
• The two heads of the pronator teres (PT) insert into the radius by a common tendon. The upper lateral border of the superficial head of PT is clearly defined (Figure 11-8). The median nerve in the distal arm and cubital fossa lies medial to the biceps and its tendon and medial to the brachial artery (Figure 11-9). The nerve is resting on the brachialis. The median nerve runs between the two heads of PT; the muscle is supplied by a specific branch of the median nerve, which frequently leaves the main trunk more proximally. The fascia superficial to the muscle is thickened by the bicipital aponeurosis.
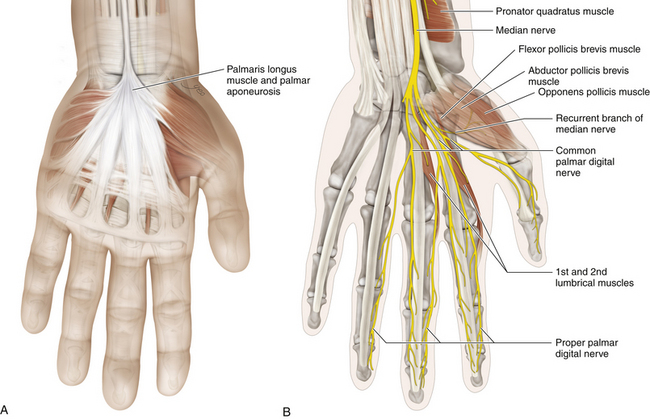
• The flexor carpi radialis (FCR) arises from the common flexor head and transforms into its large tendon at the midforearm level. The tendon crosses the median nerve superficially en route to its insertion, lateral to the median nerve at the wrist.
• The palmaris longus (PL) is a small muscle with a long tendon, which inserts into the palmar aponeurosis. The tendon is stuck to the superficial surface of the flexor retinaculum. Proximal to the wrist, the median nerve lies deep to the interval between the FCR and the PL (Figure 11-10).
The Median Nerve Passing Through the Pronator Teres
• After giving off a few branches to the pronator teres, the median nerve passes between the two heads of the PT and then crosses the ulnar artery anteriorly (Figure 11-11).
• Emerging from the distal border of the PT, the median nerve passes deep to an arch created by the two heads of the flexor digitorum superficialis (FDS) (Figure 11-12).
• The FDS arises from two heads on the radial and ulnar side of the forearm. The arch formed between the two heads covers the median nerve as it leaves the lower border of the PT. The nerve is stuck to the deep surface of the FDS and escapes lateral to the FDS tendons in the distal forearm. (Figure 11-13)
• The anterior interosseous nerve arises laterally from the median nerve.
• Below the PT and FDS, the course of the median nerve in the forearm continues in a straight line into the wrist, on the radial side of the tendon of the PL.
• Proximal to the anterior interosseous branch, the median nerve supplies the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis (Figure 11-14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree