CHAPTER 9 Meningiomas and Brain Edema
INTRODUCTION
According to the Central Brain Tumor Registry of the United States, meningiomas account for more than 30% of all primary brain tumors.1 It is well recognized that there is a significant difference in the incidence of meningiomas between females and males. Among females, meningiomas represent about 38% of all intracranial tumors compared to 20% of all tumors in males, a difference that is much higher for spinal extramedullary tumors.2 Age represents another relevant factor in their epidemiology, with the incidence of meningiomas increasing from 0.3/100,000 in childhood to more than 8.4/100,000 in the elderly population.3
Despite their prevalence, the vast majority of meningiomas are extra-axial, benign slow-growing tumors arising from arachnoid cap cells. Hence, many meningiomas, including those that are relatively large, are asymptomatic and do not require active intervention, especially in the elderly or in those with medical comorbidities. However, meningiomas can cause neurologic symptoms due to local growth and compression of adjacent brain structures and cranial nerves; irritation of the adjacent cortex leading to seizures; and pain syndromes due to involvement of cranial nerves, adjacent dura, and skull base structures. The majority of these symptoms evolve slowly and are related to the insidious growth of the benign meningioma. Elective surgery, supplemented with adjuvant radiation when indicated, usually provides long-term cure or tumor control with minimal morbidity, as discussed elsewhere. However, certain locations and biological subtypes of meningiomas still pose significant management challenges requiring a multidisciplinary approach and ongoing research into the molecular biology of these tumors.2
MENINGIOMA AND PERITUMORAL BRAIN EDEMA
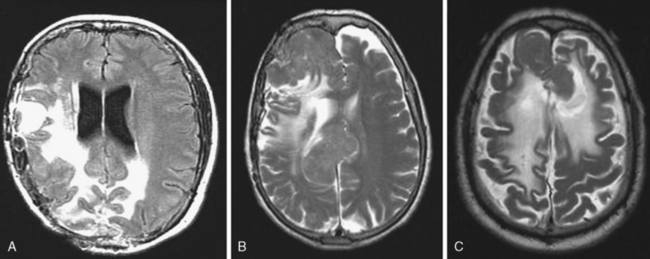
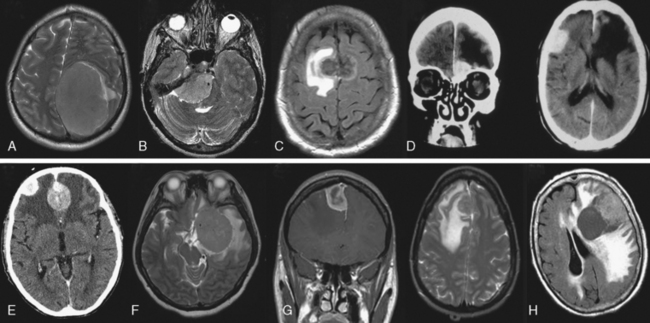
The presence of peritumoral brain edema (PTBE) associated with meningiomas is relatively common and has been quoted in different series to be present between 40% and 92% of the time.4–6 The incidence of PTBE resulting in significant neurologic deficit, thereby reducing the patient’s performance status and negatively affecting the surgical outcome, is unknown. Although this number is likely much lower, PTBE still represents a significant pre- and postoperative clinical issue in a sizable number of patients.7,8 As discussed in the text that follows, several structural, pathologic, and molecular correlates of meningiomas and associated PTBE have been proposed, with likely no one single etiology that adequately explains all cases. For example, although the incidence of significant PTBE is more with malignant meningiomas, the vast majority occur in the much more common totally benign meningioma (Figs. 9-1 and 9-2). Location around major venous sinuses or draining veins has been implicated as another association, but meningiomas with significant PTBE are found in the convexity, skull base, as well as those in the parasagittal region (see Fig. 9-2). Size of the meningioma has also been linked to PTBE, but large series have not clearly documented this to be true, as demonstrated by the significant PTBE in the smaller of two meningiomas in the same patient in (Fig. 9-2D).
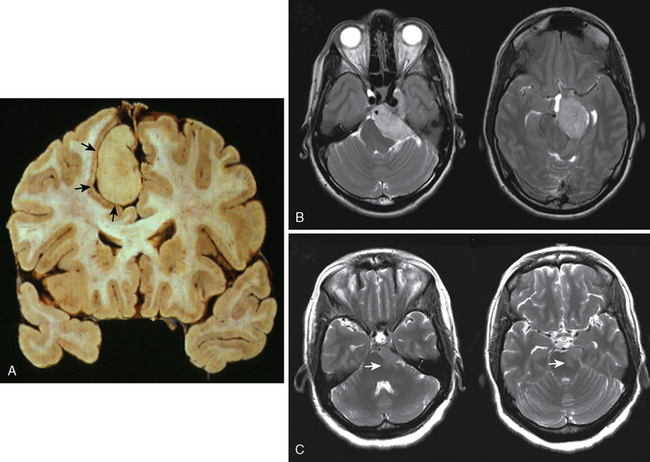
There is agreement that at a histologic level, ablation of the usually present intact arachnoid plane separating the tumor from adjacent brain (Fig. 9-3A) or subpial extension of the tumor, such as in malignant meningioma, is associated with increased incidence and severity of PTBE. The presence of T2 signal change in the parenchyma at the tumor–brain interface correlates well to the loss of a patent arachnoid plane (Fig. 9-3B, C). These subtle but important preoperative radiologic features should be recognized to properly plan the extent of resection with minimal exacerbation of neurologic deficits, especially in meningiomas that grow against eloquent regions of the brain, such as the brain stem (Fig. 9-3C).
MECHANISM(S) AND QUANTIFICATION OF BRAIN EDEMA
Vasogenic edema is the most relevant type of edema associated with intra- or extra-axial tumor-associated PTBE, including meningiomas.9 Vasogenic edema is characterized by an increase in extracellular fluid volume due to breakdown of the blood–brain barrier (BBB), with increased permeability of brain capillary endothelial cells to macromolecular serum proteins such as albumin. The main ultrastructural basis of the intact BBB is the presence of endothelial cell tight junctions or zona occludens, a key differentiating factor of CNS versus systemic vasculature. In addition to tight junctions, the fully mature BBB is also dependent on the glial foot processes that wrap around the vessels and lack of pinocytic transcellular vesicular transport in the CNS endothelial cells. The onset of vasogenic edema is more subacute to chronic compared to cytotoxic edema, as it requires disruption of the substrates of the BBB described in the preceding text. However, acute cytotoxic edema is usually followed within the next few hours to days by the development of vasogenic edema, as endothelial and glial cell death leads to disruption of the BBB. Breakdown of the ultrastructural substrates of the BBB mentioned earlier in the peritumoral brain is usually not secondary to a primary cytotoxic injury. It likely is a result of combination of potentially reversible mechanical, physiologic, and molecular alterations triggered by the tumor, as discussed in detail later. To better understand and potentially treat PTBE it is essential to be able to quantify it both in preclinical and clinical settings. Accordingly, the simple edema index defined by magnetic resonance imaging (MRI) volumetric measurements as:
has proven to be reliable measurement of communication between investigators.10–13 Accordingly, an edema index of 1 by definition implies lack of any PTBE.
POTENTIAL ETIOLOGIES OF MENINGIOMA-ASSOCIATED PTBE
Gender, Age, Size, and Location
It is well recognized that meningiomas express estrogen and progesterone receptors,14–16 perhaps linked to the underlying prevalence of these tumors in females and occasional increased growth noted with pregnancy. A correlation between number of sex hormone receptors and PTBE in meningiomas has been proposed.17 In this study, estrogen and progesterone receptors were measured in 22 meningiomas and correlated to the amount of PTBE estimated on computed tomography (CT) scans. Of the 22 cases, 19 were positive for progesterone receptors and all of these meningiomas exhibited significant PTBE. None of these 22 meningiomas was estrogen receptor positive. If indeed true, such a link between progesterone receptors and PTBE may have therapeutic implications, using antiprogesterone therapy in the treatment of meningioma-related PTBE. Although encouraging, several systematic studies have failed to consistently demonstrate such a link with sex hormones and gender on PTBE,18,19 in keeping with a clear lack of efficacy of antiprogesterone therapy to check the growth of meningiomas.
Similar to gender, increasing age has been suggested to confer a higher prevalence of significant PTBE in meningiomas and thereby contribute to a higher surgical morbidity.18 However, most authors have not been able to verify this observation, although increasing age does put the patient at much higher surgical risk, but due to systemic comorbidities and not increased PTBE.19 Tumor size has also failed to correlate unambiguously with the amount of PTBE. In a cohort of 175 patients, larger size meningiomas correlated with increased PTBE.20,21 However, in two separate series of 55 and 25 meningiomas, tumor size did not correlate with PTBE.18 Our own experience is similar, as demonstrated in Figure 9-2D, where significant PTBE was present in the smaller anterior skull base meningioma, necessitating surgery, versus the much larger but asymptomatic contralateral meningioma.
Location of meningioma and associated PTBE also remains controversial. Several authors have reported increased incidence of PTBE in frontal sphenoidal ridge meningiomas in comparison to meningiomas in other areas of brain.22,23 It is postulated that this resulted from impeded venous drainage through the middle cerebral vein. However, as discussed later, the degree of obstruction to venous drainage did not clearly show a relationship to PTBE. Similarly, tumors of the falx, convexity, and anterior fossa have also been linked with greater PTBE.19 However, other studies examining meningiomas originating from the convexity, falx, sphenoid ridge, tentorium, suprasellar region, cerebellopontine angle, and posterior fossa, did not find any correlation with PTBE.18 There does seem some consensus that posterior fossa meningiomas generally do not have significant PTBE on presentation.18,19,24,25 A plausible explanation for this observation may lie in the relative paucity of white matter, which is preferentially affected by vasogenic edema, in the posterior fossa compared to the supratentorial cortex.25 However, perhaps a more likely explanation is that meningioma and other tumors in the posterior fossa are diagnosed earlier, before PTBE, due to early onset of symptoms.
Tumor Margin, Subtype, and Grade
The gross appearance of tumor–brain margin has been postulated to be an important determinant of PTBE. Meningiomas with irregular margins are grouped as “lobulated,” whereas meningiomas with smooth margin can be considered “nonlobulated.” One report links meningiomas with tumor lobulation to have increased PTBE26 however, this was not verified in another study.18 Several studies have implicated histologic subtypes or the WHO grading of meningiomas with the occurrence of PTBE.10,12,27,28 In particular, “meningothelial” meningiomas, which potentially are more invasive and able to damage the leptomeninges and cortex, thereby allowing the transmission of edema into the white matter, have been associated with increased PTBE compared to the “fibroblastic” subtype.29 However, other studies do not corroborate these observations and do not find any correlation between PTBE and subtype of benign meningiomas.18,19,30 In contrast to subtypes of benign meningiomas, there is general agreement that atypical or malignant meningiomas induce a greater degree of PTBE. This may be related to their rapidity of growth with breach of the arachnoid plane and subpial extension, with and without frank brain invasion. In addition, these higher grades of meningiomas also secrete a larger number and greater quantities of edemogenic cytokines, as discussed later.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree