Mental health services I
Case history 1
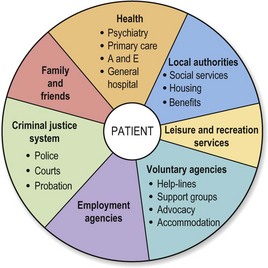
Most mental illnesses are caused by a combination of biological, psychological and social factors. Some patients have complex needs that cannot be met by a single mental health professional. When ill, patients are often unable to fulfil their usual role at home, work and elsewhere, and may neglect or harm themselves. Their behaviour may be odd, impulsive, disinhibited or violent, and this may damage relationships or lead to others being harmed. Social factors such as homelessness and unemployment may act as precipitating or maintaining factors in the illness, and clearly cannot be ignored in treatment. It is essential, therefore, that a mental health service should include psychiatric services, social services, housing agencies, voluntary agencies and others working closely together (Fig. 1). This style of inter-agency working is characteristic of psychiatry and distinguishes it from many other branches of medicine. Psychiatrists usually work in multidisciplinary teams, in a variety of settings, including hospitals and the community.
The changing face of psychiatry
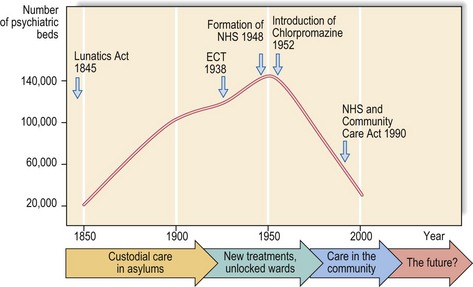
Since then there has been a steady move towards providing psychiatric treatment in the community. Psychiatric inpatient beds have been closed in large numbers (Fig. 2), and long stay residents of the old institutions have been rehoused, some to independent living and others to wards in the community, staffed hostels or supported lodgings. Where possible, patients are now treated in their own homes, outpatient clinics or day hospitals. Inpatient treatment will always be necessary for some and, ideally, should be provided in purpose-built units close to the community that the patient comes from, allowing regular contact with family and friends and a smooth transition from hospital to home when well.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree