Fig. 3.1
The FNA smear. Poorly cohesive cells condensed around thin vasculature. Fairly uniform cells with moderate anisonucleosis (inset) (×100 and ×1,000, DQ)
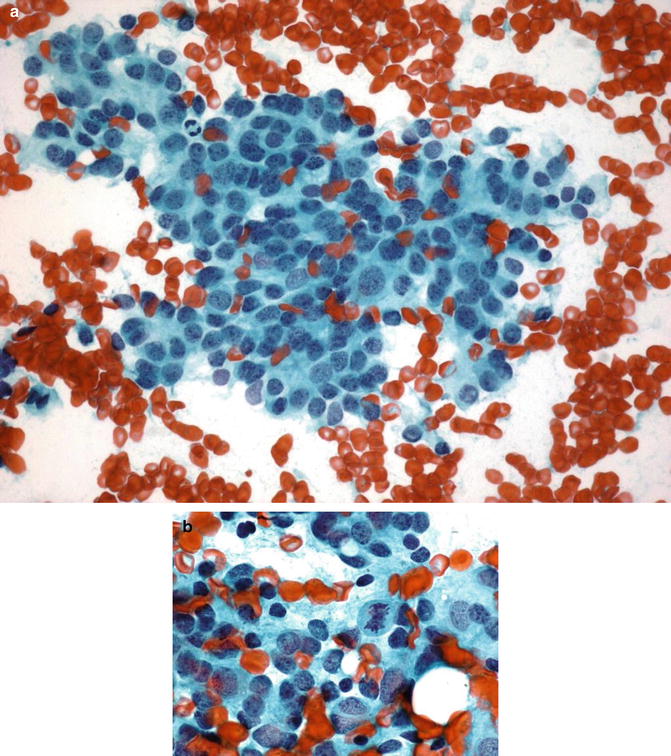
Fig. 3.2
The FNA smear. Round nuclei with evenly distributed chromatin and minimal membrane irregularity. Frequent mitosis (inset) (×400 and ×1,000, PAP)
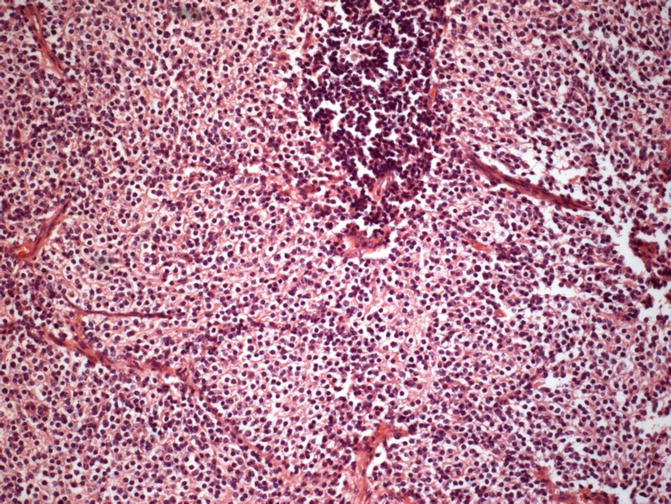
Fig. 3.3
Histologic section. Sheets of monotonous, small cells with clear cytoplasm and round nucleus, consistent with oligodendroglial tumor and residual lymph node tissue (×200, Hematoxylin-Eosin)
As a result, squash, smear or touch preparation cytology findings described in the primary oligodendroglial tumors are slightly different from FNAC findings of their metastatic lesions (Watson and Hajdu 1977; Can et al. 2012). For example, significant fibrillary ground, mini-gemistocytes and microcalcifications may not exist in metastases. The reason for this can be speculated as inappropriate microenvironment conditions of the target organ and/or insufficient time to generate their unique tissue pattern.
Cytological features of metastatic oligodendrogliomas, particularly of pure ones, necessitate differential diagnosis with SRCT group and it is quite difficult. In the literature, very few case reports in which definitive diagnosis has been made by cytological findings are available, though immunocytochemistry (ICC) is generally required (Lopez-Rios et al. 2000; Can et al. 2012). ICC can be performed on cytospin slides or smear preparations prepared from FNA material. Immunohistochemistry (IHC) can also be performed on parafin-embedded cell block samples prepared from FNA material. As oligodendroglial tumors are usually observed among adult age group, differential diagnosis of SRCT includes small cell neuroendocrin carcinoma, Ewing’s sarcoma/primitive neuroectodermal tumor (EWS/PNET), hematolymphoid malignancies, and rarely small cell variant-melanoma, small-cell osteosarcoma, mesenchymal chondrosarcoma. Any positivity of glial fibrillary acidic protein (GFAP), if present, is very helpful in diagnosis; however, in contrast, focally positive results are noted to be obtained particularly with polyclonal markers in some of the non-glial tumors (Budka 1986). Thus, microtubule-associated protein 2 (MAP-2), SOX10 and glial-lineage markers, such as Olig-1 and Olig-2, may be more helpful in the diagnosis than GFAP staining, although there is insufficient literature data regarding their expression in other SRCTs (Reifenberger et al. 2007). Neoplastic oligodendroglial cells are also positive for neuron specific enolase (NSE), synaptophysin, CD57 (leu-7), and vimentin, but these markers have lower specificity, especially when PNET is considered in the differential diagnosis. Again, oligodendroglial tumor cells are positive for nuclear and cytoplasmic S-100 protein, but this marker cannot be used for the differentiation of PNET, metastatic melanoma or chondrosarcoma. In the very limited literature data, oligodendrogliomas are negative for CD99, as a marker of PNET. Negative results for leukocyte common antigen (LCA), CD20, CD3, CD138 or CD38, myeloperoxidase (MPO), desmin, HMB45, epithelial membrane antigen (EMA), and cytokeratin can also be used in differential diagnosis. However, to know patient’s history will substantially prevent unnecessary and confusing immunochemistry applications.
Detection of 1p/19q co-deletion by fluorescent in situ hybridization (FISH), polymerase chain reaction (PCR) or comparative genomic hybridization techniques has diagnostic, prognostic and even predictive value for oligodendroglial tumors. 1p/19q co-deletion was also observed in recurrence and metastatic (in few case reports) oligodendroglial tumors (Wang et al. 2004; Bruggers et al. 2007; Campbell et al. 2008; Krijnen et al. 2010; Noshita et al. 2010; Can et al. 2012). For the first time, Wang et al. (2004) demonstrated 1p/19q co-deletion by using capillary electrophoresis and PCR techniques on a cell-bock specimen obtained from FNAC material of an oligodendroglioma case with intraparotid lymph node metastasis. Also, 1p/19q co-deletion by FISH can be performed on cytospin slides or cell blocks. However, it should be kept in mind that the presence of co-deletion is considered highly suggestive for the diagnosis, while its absence will not rule out the diagnosis at all.
Result
Clinical and FNAC findings of metastatic oligodendroglial tumors are briefly reviewed. As a take home message, systemic work-up for metastases should be done in the patient with history of primary central nervous tumor, especially when unexplained clinical symptoms are present and FNAC, is one of the rapid and direct diagnostic methods that should be considered for diagnosis of suspected metastatic mass. Metastatic oligodendrogliomas have some cytomorphologic characteristics that may lead to a definitive diagnosis with the combination of clinic-radiologic data. Moreover, some initial ancillary diagnostic studies such as 1p/19q co-deletion by FISH may provide additional prognostic and predictive information.
References
Campbell BA, Horsman DE, Maguire J, Young S, Curman D, Ma R, Thiessen B (2008) Chromosomal alterations in oligodendroglial tumours over multiple surgeries: is tumour progression associated with change in 1p/19q status? J Neurooncol 89:37–45PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






