♦ Preoperative
Operative Planning
- Review of imaging (MRI with gadolinium enhancement)
- Stereotactic MRI for surgical planning
- Reconstruct images with frameless stereotaxy system
- Plan operative trajectory that will avoid eloquent structures while allowing for most direct access to tumor
Equipment
- Major craniotomy tray
- Mayfield head holder
- High-speed drill
- Irrigating bipolar cautery
Operating Room Set-up
- Ultrasound with small probe and sterile cover for intraoperative use
- Stereotactic navigation system
- Operating microscope (if necessary)
Anesthetic Issues
- Scalp block prior to pinning
- Intravenous dexamethasone (usually 10 mg)
- Preoperative intravenous antibiotics 30 min prior to incision
- Maintenance of the patient’s anticonvulsant in high therapeutic range
- Specifically review medical history with anesthesiologist since many patients will have comorbidities; discuss possibility and management of increased intracranial pressure
♦ Intraoperative
Positioning
- In general, it is best to position the patient so that the side where the tumor resides is elevated. If stereotactic navigation is being used, it is important to position the patient so that the reference arc is visible to the cameras. For metastatic tumors in the speech and/or motor areas, awake craniotomy or intraoperative electrophysiological monitoring may be necessary.
- For frontal tumors, position patient supine with head above heart by elevating the patient’s back. For tumors near the midline, the singe pin should be placed on the side containing the tumor just posterior to and above the ear. The double pins should be placed on the contralateral side behind the ear, in the coronal plane. This is done to facilitate a bicoronal incision, if necessary.
- For temporal and parietal tumors, we recommend positioning the patient laterally. This is usually performed using a flexible bean bag and appropriate padding. An axillary roll should be used. Alternatively, the patient may be positioned supinely with a shoulder roll and the head turned contralateral to the side of the location of the tumor. Care must be taken not to turn the neck too much, thereby impeding venous outflow. The patient’s head should be clamped with the single pin placed on the forehead on the side contralateral to the tumor’s location. The double pins should be placed well behind the ipsilateral ear at the back of the head, with enough room to accommodate an incision that extends behind the ear.
- For occipital tumors, the patient may be positioned laterally, three quarters prone or prone. For three quarter prone positioning, we recommend use of a bean bag, with the patient’s body placed laterally. For better exposure, the head may be turned contralateral to the side where the tumor resides. For prone positioning, the patient may be placed on gel rolls.
- For frontal tumors, position patient supine with head above heart by elevating the patient’s back. For tumors near the midline, the singe pin should be placed on the side containing the tumor just posterior to and above the ear. The double pins should be placed on the contralateral side behind the ear, in the coronal plane. This is done to facilitate a bicoronal incision, if necessary.
Planning of Incision
- For medial or low frontal tumors, an incomplete bicoronal (i.e., the incision does not have to extend completely from ear to ear) incision may be used. This will facilitate access to the falx if necessary. Care should be taken not to violate the frontal sinus. This may be identified on preoperative imaging or by intraoperative stereotactic navigation.
- Alternative incisions include curvilinear or horseshoe-shaped configurations.
Craniotomy
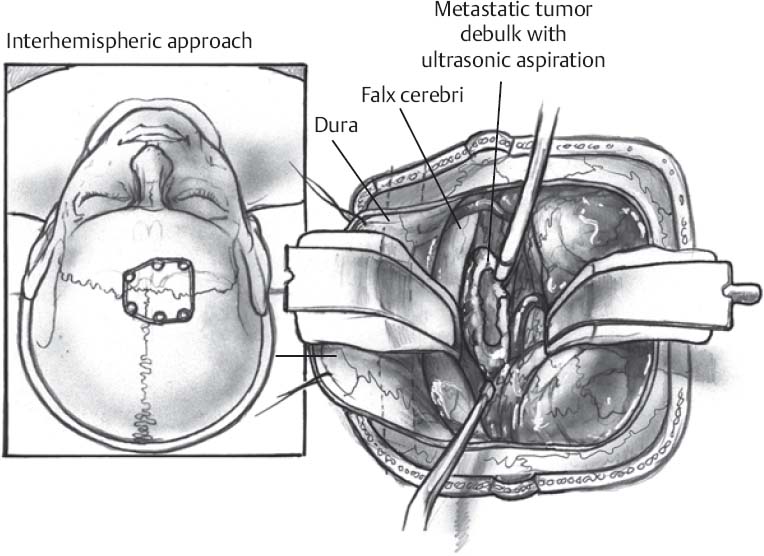
- Stereotactic navigation can be used to plan the craniotomy flap. If necessary, the flap may need to come to or cross the midline for medial frontal tumors. Stereotactic navigation may be used to identify the sagittal sinus and the frontal air sinus.
- Multiple burr holes may be used. The dura is stripped from the underside of each burr hole in every direction.
- Maximize the bony opening so that it is larger than the dural opening necessary to resect the tumor. A larger opening may be necessary if intraoperative electrophysiology is to be used (e.g., to expose motor cortex).
- The craniotomy is generally performed with a high-speed drill with a foot plate attachment. The flap is elevated with a periosteal elevator, and the dura is stripped from the bone with a dissector such as a Penfield no. 3.
- Tack-up sutures are placed around the perimeter of the bony opening to prevent epidural oozing.
- Ultrasound may be used at this point to identify the tumor. Metastatic tumors should be hyperechoic.
- The dura is generally opened in a curvilinear or cruciate fashion. If the sagittal sinus is exposed or forms a boundary of the craniotomy, the dura should be opened such that the base of the dural flap is along the sinus. The dura may then be tacked to the drapes or skin to keep it reflected.
- Once the dura is opened, neuronavigation or intraoperative ultrasound may be used to gain an appreciation of the location of the tumor if it is not visible at the brain surface.
- Ultrasound may be used at this point to identify the tumor. Metastatic tumors should be hyperechoic.
Tumor Resection
- If the tumor is in an area of eloquent cortex, awake craniotomy techniques (e.g., to localize speech areas) or electrophysiologic monitoring (e.g., to identify the motor cortex through phase reversal) may be necessary.
- A transsulcal approach may be used to avoid a corticectomy. Care must be taken, however, to avoid injury to the traversing vessels in the sulcus.
- The goal is gross-total resection of the tumor. This should be performed by removing the entire tumor and minimizing resection of normal adjacent tissue. The tumor is dissected from surrounding brain; in general, retraction should be applied to the tumor and not the surrounding brain.
- For large tumors, intralesional resection is necessary to debulk the mass (Fig. 54.1). Other tumors may have a capsule with enough integrity to facilitate en bloc removal.
Only gold members can continue reading. Log In or Register to continue







