10 | Metastatic Tumors of the Cervical Spine |
 | Case Presentation |
History and Physical Examination
A 33-year-old female presented in 1997 with a 3.5 cm left breast mass detected on self-examination. A core biopsy was performed revealing infiltrating ductal carcinoma. A lumpectomy confirmed the core biopsy finding with the addition of lymphovascular invasion, and a sentinel node biopsy revealed carcinoma. The tumor was estrogen receptor positive, and progesterone and Her-2/neu negative. Metastatic workup was unrevealing and the diagnosis of stage 2 breast carcinoma was confirmed. She was treated with focal breast external beam radiation therapy (EBRT), followed by doxorubicin and cyclophosphamide, methotrexate, and, 5 fluorouracil (CMF) chemotherapy, and tamoxifen. She was started on monthly injections of the bisphosphonate, Zometa (Novartis International AG, Basel, Switzerland).1–3
In 2003, the patient presented with mild nocturnal and early morning cervical spine pain that would persist for an hour and then resolve. She had no other pain over the course of the day. Three months later, she had onset of severe neck pain while playing with her children. The pain was worse on neck extension and lateral rotation and was associated with lancinating, left-sided, occipital headaches. She was neurologically normal. On presentation to the emergency room, she was placed in a rigid cervical orthosis.
 | Radiological Findings |
Plain radiographs, magnetic resonance imaging (MRI) scan, and computed tomographic (CT) scans were obtained. A pathological fracture of the C2 body resulted in a significant fracture subluxation. Flexion and extension films were not obtained due to the severe pain and the degree of fracture subluxation (Fig. 10–1).
Complete spine MRI with and without contrast confirmed the pathological collapse of the C2 vertebral body with angulation of the odontoid process. There was no evidence of spinal cord compression, but a prevertebral, retropharyngeal soft tissue mass was seen. The thoracic and lumbar films showed no further evidence of bone infiltration or epidural or leptomeningeal disease.
CT scans of the cervical spine revealed infiltrative, lytic destruction of the C2 body, but the remainder of the spinal elements were intact. A CT scan of the head showed no contrast-enhancing lesions or edema. Additionally, the keel of the suboccipital bone was midline and measured 14 mm. Chest, pelvis, and abdomen CT scans showed two small pulmonary nodules but no pleural effusion. Blood work was normal.
Diagnosis
Metastatic C2 fracture with atlantoaxial subluxation
 | Background |
The initial presentation in this patient of nocturnal or early morning pain is consistent with biological or tumor-related pain and is not indicative of instability. This pain is the most common early presenting sign of a spine tumor. Purportedly, biological pain results from a diurnal variation in adrenal steroids causing exacerbations resulting from inflammatory mediators released by tumors. Biological pain can often be treated acutely with steroids and definitively with radiation. Presumably, 3 months later, the patient developed significant movement-related pain when she acutely developed a C1-2 fracture subluxation.
Many patients with atlantoaxial tumor present with severe movement-related pain either with or without a significant fracture subluxation.4 This pain is often worse in extension and virtually always has a component of pain on lateral rotation.5,6 As with the patient presented, 30% of patients will have occipital neuralgia.
Radiographic criteria are used to distinguish patients who are unstable and require an operation from those who will respond to EBRT alone.7–9 Pathological instability in the atlantoaxial spine is defined as pain in conjunction with plain radiographs showing a fracture subluxation with odontoid displacement greater than 5 mm or a hangman’s fracture, Effendi type 4, with greater than 11 degrees of angulation and 3.5 mm displacement.
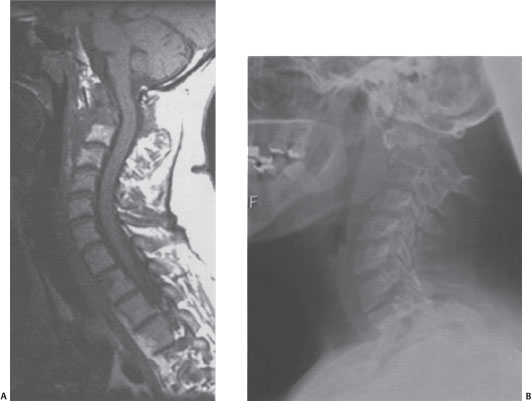
Figure 10–1 (A) Sagittal T1-weighted preoperative magnetic resonance and (B) plain radiographic preoperative images showing an unstable fracture subluxation.
Patients who have pain and significant fracture subluxations indicative of instability require operations for decompression and internal fixation. In a series reviewed at the Memorial Sloan-Kettering Cancer Center (MSKCC), patients who were irradiated despite meeting the criteria for instability inevitably had ongoing neck pain and ultimately required operations.7 Conversely, we have followed a few patients who met the radiographic criteria for instability but had no significant neck pain. These patients were not operated and only became unstable if they had local progression of disease. These patients can be followed with serial examinations and radiographs. The surgical outcomes for patients with instability are excellent in terms of pain relief and neurological and functional outcomes. Pain relief is often complete, from greater than 7 on a visual analog scale (severe pain) to less than 4 (mild pain).
 | Authors’ Preferred Method of Surgical Management |
This patient was dispositioned to surgery due to the acute fracture subluxation associated with severe pain on extension and lateral rotation of the neck denoting instability. She was loaded with Decadron 10 mg (Merck and Company, Inc., Whitehouse Station, NJ) followed by 4 mg every 6 hours. The patient was brought to the operating room and was induced with general anesthesia using fiberoptic intubation. Neurophysiological monitoring was employed. The patient was turned in the prone position after application of the Mayfield fixation device. After establishing somatosensory evoked potential (SEP) baselines, radiographic reduction was attempted by extending the head. The fracture could not be reduced and the patient’s head was affixed to the operating table in the May-field fixation device (Integra, Plainsboro, NJ). Due to the inability to reduce the fracture, the intraoperative decision was made to decompress the spinal canal via a laminectomy and perform an occipitocervical fixation.
The incision was opened from the inion to C7. Decompression was initially performed by removing the posterior arch of C1 and lamina of C2. Bilateral lateral mass screws were then placed from C3 to C6. A plate was affixed to the midline keel of the suboccipital bone using two 14 mm screws. The rods were contoured to engage the occipital plate and lateral mass screws. Local autologous bone graft and allograft chips were placed over the posterior elements after decortication. A drain was placed in the epidural space and exited through a separate stab wound. Neurophysiological monitoring was stable throughout the procedure. The patient was transferred to the recovery room neurologically normal (Fig. 10–2).
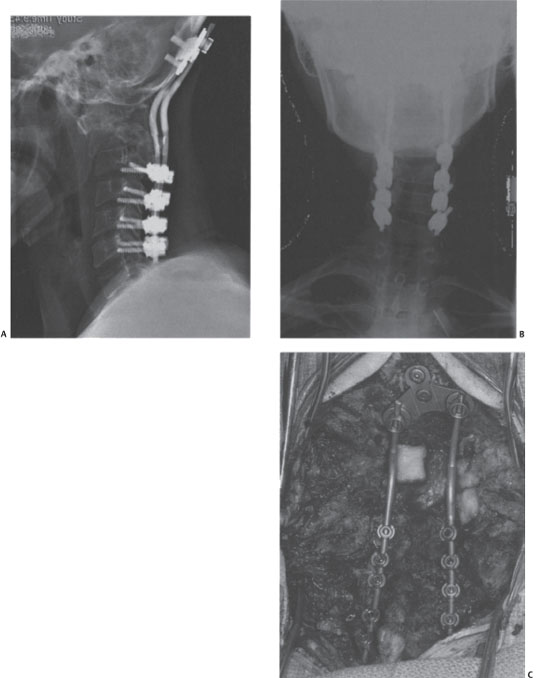
Figure 10–2 (A) Lateral and (B) anteroposterior plain radiographs showing occipitocervical fixation. The occipital plate was connected to the skull using 14 mm screws. The lateral mass screws were placed from C3 to C6. The C2 fracture subluxation was not reduced, but decompression was accomplished with a C1-2 laminectomy. (C) Intraoperative photograph showing the posterior decompression and occipitocervical fixation.



