Microcephaly
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Secondary/Acquired from
Hypoxic Ischemic Encephalopathy
TORCH Infections
Nonaccidental Trauma
Meningitis
Fetal Alcohol Syndrome
Less Common
Primary/Genetic with
Gyral Simplification
Cortical Dysplasia
Midline Anomaly
Cerebellar Hypoplasia
Hypomyelination
Rare but Important
Microlissencephaly
Pseudo-TORCH
Aicardi-Goutieres
Progeroid Syndromes
Cockayne
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Was head circumference ever normal?
Decreased cranio-facial ratio on sagittal view helpful, tape measure best
Helpful Clues for Common Diagnoses
Hypoxic Ischemic Encephalopathy
Patterns helpful, even if no history
Profound: Atrophy, gliosis posterior putamen, lateral thalami, rolandic cortex
Prolonged progressive: Typical watershed encephalomalacia
Mixed: Features of both, ± calcified thalami
TORCH Infections
Agents most frequently causing microcephaly
Cytomegalovirus (CMV) most common by far
Rubella (now rare)
Look for cortical dysplasia, periventricular Ca++, hypomyelination (typically associated with CMV)
Nonaccidental Trauma
History is crucial
BUT look for evidence of trauma/fractures on ALL available films
Brain imaging
Global atrophy or hemiatrophy
Hemosiderin
Meningitis
Early infancy: Group B strep the most damaging
Hypothalamus
Chiasm
Inferior basal ganglia
Diffuse cortex, often asymmetric
Fetal Alcohol Syndrome
Microcephaly
By tape measure or MR volumetrics
Anomalies may occur, but not specific
Diffusion tensor imaging (DTI) reported to show abnormal connectivity
Helpful Clues for Less Common Diagnoses
Gyral Simplification
Small, grossly normal brain
Looks like “small, but perfect brain”
Corpus callosum may appear thick, lack isthmus
Cortical Dysplasia
Any severe, diffuse dysplasia
Lissencephaly
Pachygyria
Midline Anomaly
Holoprosencephaly, agenesis CC
Assess corpus callosum presence, size, shape
Is there an isthmus?
Holoprosencephaly
Most severe are the smallest
Cerebellar Hypoplasia
May be clue to rare disorders
Microlissencephaly
TUBA1A mutations: Lissencephaly PLUS cerebellar hypoplasia
Assess degree of deficiency
Fastigial recess, primary fissure
Degree of vermian lobulation
Tegmento-vermian angle (is the inferior 4th ventricle open?)
Hypomyelination
Helpful Clues for Rare Diagnoses
Microlissencephaly
“Z-shaped” brainstem
Callosal agenesis
Surface often totally smooth
Very small brain
Pseudo-TORCH
Aicardi-Goutieres
Autosomal recessive, important to diagnose
Elevated CSF alpha-interferon
Early onset: TREX1 mutation
Late onset: RNASEH2B mutation
Imaging CMV-like
Ca++
Hypomyelination
Atrophy
Progeroid Syndromes
Cockayne
Cachectic dwarfism with mental retardation
Disorder of DNA repair
Several mutations known
Lack phenotype-genotype correlation
Facies & neuroimaging progressive
Basal ganglia/dentate Ca++
Demyelination
Atrophy
SELECTED REFERENCES
1. Gul A et al: Novel protein-truncating mutations in the aspm gene in families with autosomal recessive primary microcephaly. J Neurogenet. 21(3):153-63, 2007
2. Hassan MJ et al: Previously described sequence variant in CDK5RAP2 gene in a pakistani family with autosomal recessive primary microcephaly. BMC Med Genet. 2007
3. Kure-Kageyama H et al: A patient with simplified gyral pattern followed by progressive brain atrophy. Brain Dev. 29(6):383-6, 2007
4. Ornoy A et al: Fetal effects of primary and secondary cytomegalovirus infection in pregnancy. Reprod Toxicol. 21(4):399-409, 2006
5. Tang BL: Molecular genetic determinants of human brain size. Biochem Biophys Res Commun. 345(3):911-6, 2006
6. Sztriha L et al: Extreme microcephaly with agyria-pachygyria, partial agenesis of the corpus callosum, and pontocerebellar dysplasia. J Child Neurol. 20(2):170-2, 2005
7. Abdel-Salam GM et al: Aicardi-Goutieres syndrome: clinical and neuroradiological findings of 10 new cases. Acta Paediatr. 93(7):929-36, 2004
8. de Vries LS et al: The spectrum of cranial ultrasound and magnetic resonance imaging abnormalities in congenital cytomegalovirus infection. Neuropediatrics. 35(2):113-9, 2004
9. Riley EP et al: Teratogenic effects of alcohol: a decade of brain imaging. Am J Med Genet C Semin Med Genet. 127(1):35-41, 2004
Image Gallery
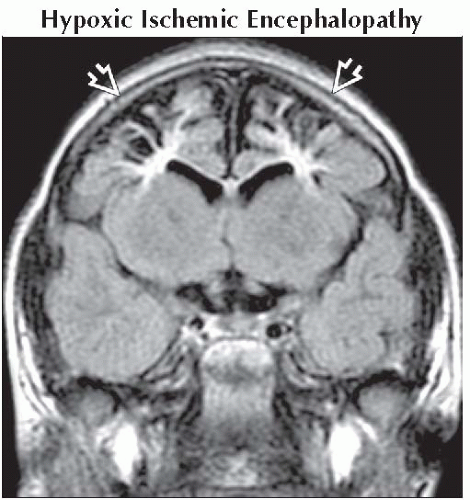 Coronal FLAIR MR shows cystic encephalomalacia
 in the border zone distribution in this 3 year old with a history of peripartum prolonged partial asphyxia. in the border zone distribution in this 3 year old with a history of peripartum prolonged partial asphyxia.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|