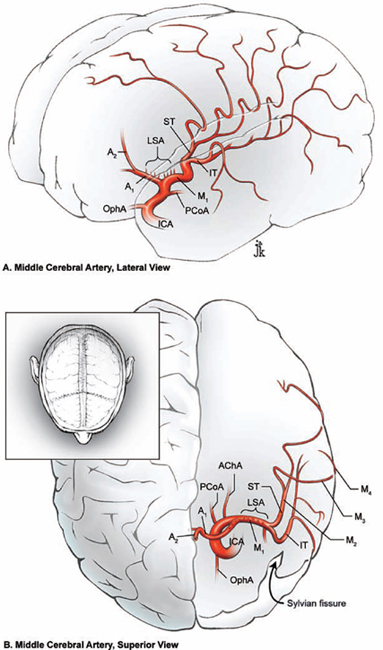
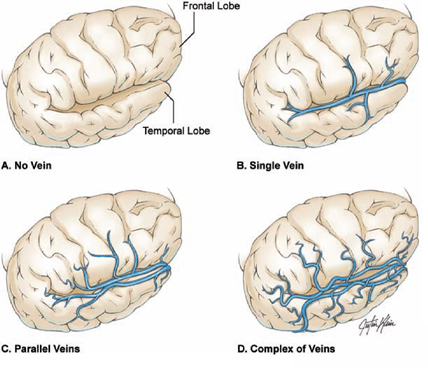
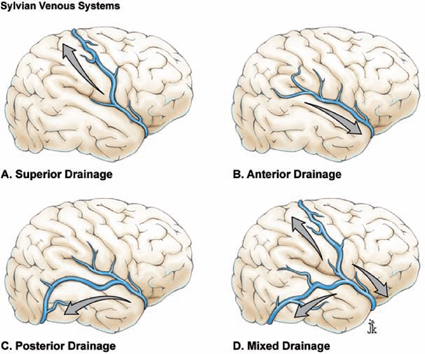
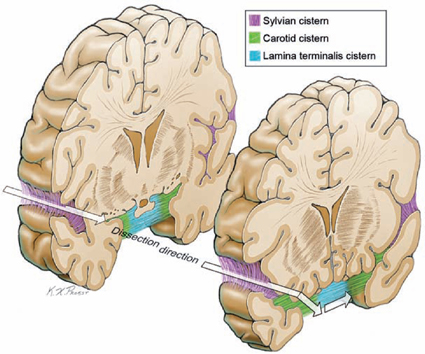
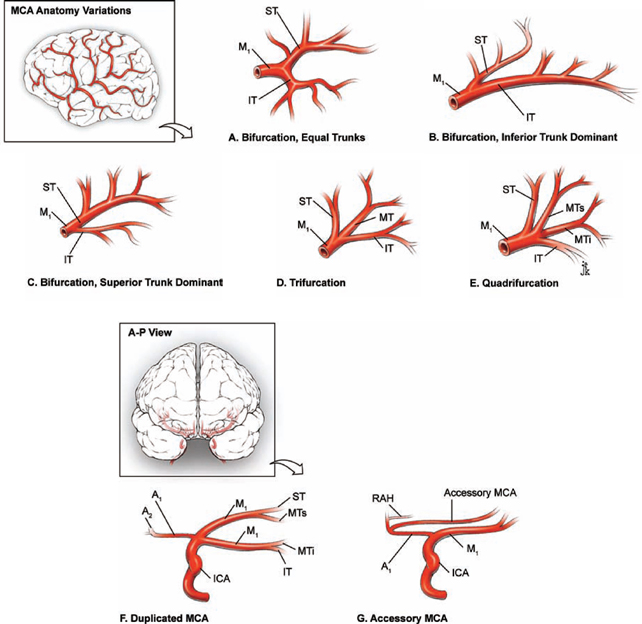
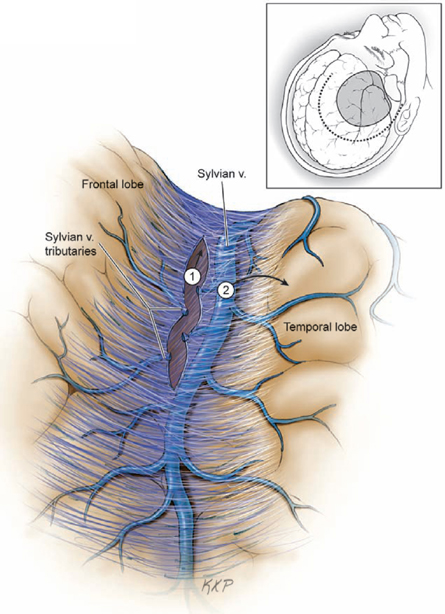
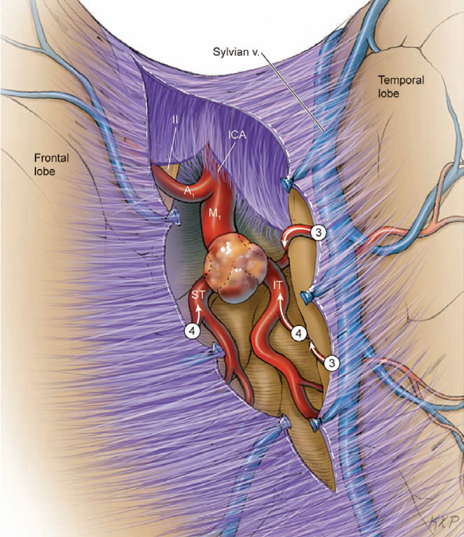
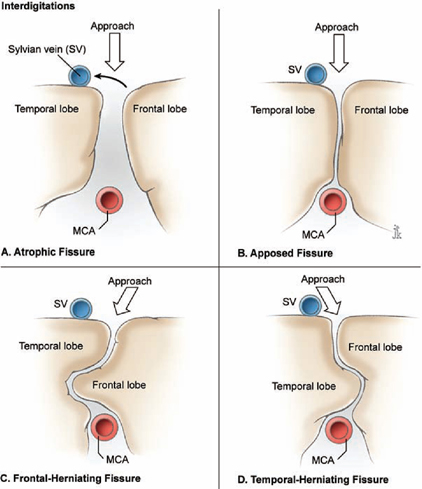
15 Middle Cerebral Artery Aneurysms Segmental anatomy is defined by the middle cerebral artery’s (MCA) complex curvature rather than its branches. The M1 segment begins at the terminal bifurcation of the internal carotid artery (ICA) and ends at the genu, a right-angle bend in the artery as it courses over a small gyrus of insular cortex, the limen insulae (Fig. 15.1). The M1 segment is named the sphenoidal segment because it parallels the course of the sphenoid ridge. The M2 segment, or insular segment, begins at the genu, runs in the insular cleft, and terminates at the circular sulcus of the insula where the arteries make their next right-angle turn. The turn in the circular sulcus may be exaggerated (90 to 180 degrees) as arteries transition from the insular surface to the medial frontoparietal opercular surface. The M3 segment, or opercular segment, begins at this genu where arteries leave the insular surface, run in the opercular cleft, and terminate at the cortical surface of the sylvian fissure. The M4 segment, or cortical segment, consists of branches supplying the lateral convexity from their emergence from the sylvian fissure to their final territory. The MCA therefore courses through the sylvian fissure from the ICA terminus to the lateral convexity, has four segments, makes three right-angle bends, alternates its orientation between horizontal and vertical, and branches distally to resemble a candelabra. The MCA bifurcates into superior and inferior trunks (Fig. 15.2), with the bifurcation located on the M1 segment if it is proximal to the genu at the limen insulae, on the M2 segment if it is distal to the genu, or at the M1–M2 junction if it is at the genu. Most MCA aneurysms are located at MCA bifurcations into superior and inferior trunks. MCA trifurcations into superior, middle, and inferior trunks are observed in less than 20% of patients, and MCA quadrifurcations are rare. Bifurcations with early secondary bifurcations of trunks can appear as quadrifurcations. Trunks can be symmetrical, but size relates to the number of distal branches, and one trunk often dominates. Anterior branches include the orbitofrontal artery, operculofrontal artery, and central sulcus artery; posterior branches include the posterior parietal artery, angular artery, and posterior temporal arteries. Trunks do most of their branching along the M2 segment, which removes these branches from the aneurysm dissection. The anterior temporal artery (ATA) originates from the inferior surface of the M1 segment and ascends the temporal lobe in the sylvian fissure. The ATA can also arise from the inferior trunk of the MCA bifurcation or from a common temporal trunk proximal to the MCA bifurcation that also gives rise to uncal and temporopolar arteries. Uncal and temporopolar arteries are normally small branches from the M1 segment proximal to the ATA. Although the common temporal trunk can create a “false bifurcation” and be misinterpreted as an early MCA bifurcation, the ATA usually is a reliable landmark during the dissection along the M1 segment toward the aneurysm. As the ATA courses over the surface of the temporal lobe to supply the temporal pole, it can drape the dome of a large or inferiorly projecting aneurysm and be misinterpreted as an inferior or middle trunk (“false trunk”). The ATA is not directly related to MCA aneurysm necks. It can be dissected off the dome to mobilize the aneurysm, or left on the dome with permanent clips applied around it. The lateral lenticulostriate arteries originate from the superior surface of the M1 segment, enter the lateral two thirds of the anterior perforated substance, and ascend to deep white matter structures that include the caudate, putamen, globus pallidus, superior half of the internal capsule, and corona radiata. Lenticulostriate arteries may be large stems with multiple secondary branches, solitary arteries that parallel the M1 segment, or small twigs perpendicular to the M1 segment. There are, on average, 10 lenticulostriates, and most arise from the pre-bifurcation portion of the M1 segment. Lenticulostriates can arise from the postbifurcation M1 segment or the M2 segment, depending on where the MCA bifurcates. The eloquent territory of lenticulostriate arteries demands careful preservation. A duplicated MCA is a second M1 segment that arises either from a supraclinoid ICA or its terminal bifurcation (Fig. 15.2). An accessory MCA is a second M1 segment that arises from the A1 anterior cerebral artery (ACA), usually near the anterior communicating artery (ACoA), resembling the recurrent artery of Heubner but for the presence of cortical branches (Fig. 15.2). Fig. 15.1 Microsurgical anatomy of the middle cerebral artery (MCA). Lateral (A) and superior (B) views showing the MCA segments: M1, sphenoidal segment; M2, insular segment; M3, opercular segment; and M4, cortical segments. AChA, anterior choroidal artery; ICA, internal carotid artery; IT, inferior trunk; LSA, lenticulostriate artery; OphA, ophthalmic artery; PCoA, posterior communicating artery; ST, superior trunk. The sylvian fissure is the gateway to aneurysms around the circle of Willis. Separation of the frontal and temporal lobes opens the subarachnoid network unlike any other maneuver, making the sylvian fissure split one of the aneurysm surgeon’s most important techniques. Superficial sylvian veins are the guardians of the sylvian fissure. Some patients have no veins, and an inviting sheet of arachnoid between the frontal and temporal lobes is all that covers the lateral sylvian cistern. Other patients have a complex of frontal, parietal, and temporal veins that course along the lips of the sylvian fissure (Fig. 15.3). The first step in splitting the sylvian fissure is to dissect beyond the veins. In general, superficial sylvian veins are mobilized to the temporal side of the fissure because they course inferiorly and bridge to the sphenoparietal sinus under the sphenoid ridge. Dissection along the temporal side of the veins would ultimately cross their outflow connections, whereas dissection along the frontal side can preserve these connections. Fig. 15.2 Normal variations of middle cerebral artery anatomy. (A) MCA bifurcation, equal trunks. (B) MCA bifurcation, inferior trunk dominant. (C) MCA bifurcation, superior trunk dominant. (D) MCA trifurcation. (E) MCA quadrifurcation. (F) Duplicated M1 MCA segment. (G) Accessory M1 MCA segment. Anterior branches include the orbitofrontal artery, operculofrontal artery, and central sulcus artery; posterior branches include the posterior parietal artery, angular artery, and posterior temporal arteries. A–P, anteroposterior; MT, middle trunk; MTi, middle trunk, inferior, MTs, middle trunk, superior; RAH, recurrent artery of Heubner. Cortical arachnoid is incised with the tip of an up-facing No. 11 scalpel blade, lifting this layer off the underlying veins and nicking it. One blade of a short microscissors enters the subarachnoid space through that nick and continues the incision, again lifting the arachnoid with the scissors blade to clear the underlying veins. Arachnoid is incised along the superficial sylvian vein from distal to proximal, coagulating and cutting venous tributaries from the frontal lobe (Fig. 15.4, step 1). The superficial sylvian vein is gradually detached from the frontal lobe and mobilized temporally (Fig. 15.4, step 2). Fig. 15.3 Normal variations of the superficial sylvian vein anatomy (right side). (A) Absence of superficial sylvian veins. (B) Single superf icial sylvian vein. (C) Parallel superficial sylvian veins. (D) Complex network of superficial sylvian veins. Fig. 15.4 Dissection steps in splitting the sylvian fissure (veins and superficial dissection, right side). Step 1, cortical arachnoid incision; step 2, temporal mobilization of the sylvian veins. Fig. 15.5 Venous systems draining the sylvian fissure: (A) superior, (B) anterior, (C) posterior, and (D) mixed systems. The superficial sylvian venous complex is composed of three interrelated venous systems (Fig. 15.5). An anterior sylvian venous system drains to the sphenoparietal sinus, cavernous sinus, and sphenobasal or sphenopetrosal sinuses; a posterior sylvian venous system drains to the lateral temporal veins, vein of Labbé, and transverse sinus; and a superior sylvian venous system drains to the frontoparietal veins, vein of Trolard, and the superior sagittal sinus (SSS). Convergence of these three venous systems along the sylvian fissure can create an obstructive tangle of veins, but it also establishes collateral venous connections that allow patients to tolerate sacrifice of a vein. Most of the time, a large sylvian vein can be rolled away from the frontal lobe and preserved. Sometimes the plane between paired sylvian veins may be the easiest pathway into the fissure. Occasionally, an adherent vein does not mobilize temporally and may need to be divided, provided that the dominant sylvian trunk is preserved and that it connects with other venous systems. Veins should be protected, but opening the sylvian fissure can require some venous pruning. The rarity of venous complications after splitting the sylvian fissure attests to the interconnections between the sylvian venous systems. Venous sacrifice can increase venous pressure in the sylvian veins and increase their fragility, so it should be delayed until the sylvian fissure split is further along. As dissection along the superficial sylvian vein reaches the temporal pole, cortical arachnoid of the distal sylvian cistern transitions to sphenoidal arachnoid of the proximal sylvian cistern. From the surgeon’s perspective, this sphenoidal arach noid is vertically oriented, and cortical arachnoid is horizontally oriented (Fig. 15.6). Sphenoidal arachnoid should be opened before proceeding to deep sylvian dissection because it couples the frontal and temporal lobes and resists deep spreading dissection. The steep view down this plane may require some frontal retraction with swollen brains. The sylvian veins frequently lie beneath sphenoidal arachnoid or can penetrate it en route to the sphenoparietal sinus. Subarachnoid hemorrhage can hide these veins, but lifting dissection with the microscissors protects underlying veins. Fig. 15.6 Subarachnoid dissection during the sylvian fissure split progresses from the distal sylvian cistern and its horizontal cortical arachnoid, to the proximal sylvian cistern and its vertical sphenoidal arachnoid. Opening the sylvian cistern leads to the carotid and lamina terminalis cisterns more medially. Fig. 15.7 Dissection steps in splitting the sylvian fissure (arteries and deep dissection). Step 3, following the cortical MCA branches to the opercular MCA branches; step 4, following the opercular MCA branches to the insular MCA branches. After mobilizing the superficial veins temporally and opening the sylvian cistern, an artery is identified as it emerges from the fissure. Arteries naturally separate the frontal and temporal lobes to define the dissection plane. This cortical artery is followed into the operculum of the sylvian fissure to develop the plane further (Fig. 15.7, step 3). Superficial sylvian dissection along the veins aligns the microscope at a shallow angle, whereas deep sylvian dissection along the opercular segments of the MCA branches aligns the microscope at a steep, downward angle, almost back toward the neurosurgeon. Cutting arachnoid bands between the frontal and temporal lobes initiates this dissection. The working area around an artery should be widened circumferentially like a funnel, rather than like a cylinder, to avoid constricted corridors. Similar working areas around adjacent opercular arteries can be developed and connected to neighboring areas of dissection (Fig. 15.7, step 3). Small opercular arteries lead to larger insular arteries, and insular arteries lead to the trunks of the MCA bi- or trifurcation (Fig. 15.7, step 4). The dissection becomes easier as it deepens because insular arteries widely separate the frontal and temporal lobes. Spreading dissection along the arteries parts the lobes from “inside out,” following a wide plane of separation deep in the sylvian fissure to narrow, more adherent areas superficially. Yasargil analogized this dissection to splitting an orange, where radial force directed outward from the center easily separates the orange wedges. The sylvian fissure is often most adherent superficially near the pterion where there are few arteries between the frontal and temporal lobes to separate the lobes. Lobules can even interdigitate, adding a rolling contour to this plane of contact (Fig. 15.8, frontal-herniating or temporal-herniating fissures). Spreading dissection from inside out is the best method for opening these difficult tissue planes. When tissues still do not separate easily, an artery might be found under sphenoidal arachnoid in the proximal fissure to reestablish the subarachnoid plane.
 Microsurgical Anatomy
Microsurgical Anatomy
 Splitting the Sylvian Fissure
Splitting the Sylvian Fissure
Veins and Superficial Dissection
Arteries and Deep Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree